Abstract
Purpose
As iron is essential for both immune function and microbial growth, alterations in iron status could influence the risk of infections. We assessed the associations of iron status with risk of bloodstream infections (BSIs) and BSI mortality.
Methods
We measured serum iron, transferrin saturation (Tsat) and total iron-binding capacity (TIBC) in 61,852 participants in the population-based HUNT2 study (1995–97). Incident BSIs (1995–2011) were identified through linkage with the Mid-Norway Sepsis Register, which includes prospectively registered information on BSI from local and regional hospitals. We assessed the risk of a first-time BSI and BSI mortality with the iron indices using Cox proportional hazards regression analysis.
Results
During a median follow-up of 14.8 years, 1738 individuals experienced at least one episode of BSI, and 370 died within 30 days after a BSI. In age- and sex-adjusted analyses, BSI risk was increased among participants with indices of iron deficiency, serum iron ≤ 2.5th percentile (HR 1.72, 95% CI 1.34–2.21), Tsat ≤ 2.5th percentile (HR 1.48, 95% CI 1.12–1.96) or TIBC ≥ 97.5th percentile (HR 1.46, 95% CI 1.06–2.01). The associations remained similar after adjusting for comorbidities and exclusion of BSI related to cancer, rheumatic illnesses and inflammatory bowel disease. BSI mortality showed similar associations.
Conclusion
Indices of severe iron deficiency are associated with an increased risk of a future BSI.
Similar content being viewed by others
Bloodstream infections and iron deficiency represent an important burden of disease. Our study assessed iron status and risk of bloodstream infections in the HUNT2 survey with 61,852 individuals and 15 year follow-up, showing increased risk of BSI among individuals with low iron status. |
Introduction
Bloodstream infections (BSIs) cause sepsis and critical illness and are major causes of morbidity and mortality worldwide [1, 2]. Due to its large impact on global health, there have been increased initiatives to identify modifiable risk factors for BSI [1, 3]. So far, we know that the risk of acquiring BSI depends on both host factors such as social and demographic factors (e.g., age, nutrition, lifestyle and poverty) [1, 4] as well as biologic factors such as host genetic susceptibility, chronic medical disorders (e.g., cancers, obesity, diabetes) [3, 5] and the ability to mount an adequate immune response to the invading bacteria [6]. Moreover, differences in virulence and antimicrobial susceptibility of infecting microbes also influence the incidence and mortality of BSI [1].
Recent advances in adaptive and innate immunity have demonstrated an essential role of systemic and cellular iron-regulating mechanisms in protecting hosts from infection [7]. On the other hand, most microbes also depend on iron for their pathogenicity, and some bacteria (e.g., Escherichia coli, Staphylococcus aureus and Pseudomonas) have evolved the ability to scavenge iron from host iron-binding proteins such as transferrin [7]. Iron is tightly bound to transferrin to control the balance between the host’s need for iron in cellular metabolism and restricting invading bacteria from obtaining iron [7]. Disturbances in this delicate homeostasis between free iron in serum and transferrin-bound iron could clearly influence the risk of BSI and sepsis [8].
Most studies of the association between disturbances in iron metabolism and risk of infections have been performed in children with iron deficiency anemia in developing countries. While some studies have shown an increased risk of infections such as respiratory tract infections [9], others have found that iron-deficient individuals seem to be less prone to infections such as malaria [10]. There is evidence to suggest a U-shaped relationship indicating that both low and high iron levels could increase infection risk [7, 11]. In the adult western population, few studies exist on the association between iron levels and susceptibility to infections. As most of these studies have used indirect markers of iron levels in serum (e.g., anemia, hypochromasia), there is also a lack of studies on the association between free iron in serum and transferrin-bound iron (i.e., iron status) and the risk of infections.
In this era of rising antibiotic resistance, we need new measures to prevent severe infections [12]. To the best of our knowledge, no study has examined the associations of iron status with the risk and mortality of BSI in a long-term follow-up in the general population. The large Norwegian population-based HUNT2 study cohort has prospective follow-up data on blood culture-positive infections over 15 years used as a specific indicator of sepsis [13, 14]. In this cohort of 61,852 adults, we assessed the association of iron status with risk of BSI and BSI mortality [15].
Methods
Study population
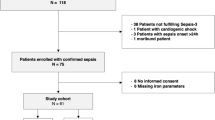
The second Nord-Trøndelag Health Survey (HUNT2, 1995–1997) invited all inhabitants ≥ 20 years old (n = 93,865) in Nord-Trøndelag county to a clinical examination that included non-fasting blood sampling, and the participants completed questionnaires covering a range of health-related topics [16] (http://www.ntnu.edu/hunt/databank). A total of 65,236 (69.5%) persons participated. Iron status measurements were performed as a population-screening for hereditary hemochromatosis, and the study revealed an estimated hereditary hemochromatosis prevalence of 0.7% [19]. No routine follow-up was carried out in pathologically low iron indices in the HUNT2 study, but later diagnostic and/or treatment cannot be ruled out. For this study, we selected all participants in HUNT2 with baseline measurements of serum iron, transferrin saturation percentage (Tsat) and total iron-binding capacity (TIBC). Using the 11-digit unique personal identification number of Norwegian citizens, the HUNT2 study cohort was linked to the Mid-Norway Sepsis Register with prospectively recorded information on all BSI events at Levanger and St. Olavs hospitals from 1 January 1995, and Namsos hospital was included in the register from 1 September 1999. The HUNT study database is regularly updated with information on site of residence and vital status from the Norwegian population register. Nord-Trøndelag county in central Norway has a population of 130,000 where 70% is served by Levanger hospital and 30% by Namsos hospital, and the tertiary referral center is St. Olavs hospital in Trondheim. The population is stable (net out-migration 0.3% per year) and ethnically homogeneous (97% Caucasians) [17]. Among the 65,236 HUNT2 participants, prior to start of follow-up (which was the entry date in HUNT2 between August 1995–June 1997 for residents having Levanger as their primary hospital and 1 September 1999 for residents having Namsos as their primary hospital) [17], 47 (0.07%) had a positive blood culture, 1140 (1.8%) migrated or died, and 2197 (3.4%) had incomplete information on iron status or comorbidities, leaving 61,852 participants for analysis (see Supplementary Figure 1).
Laboratory measurements
Fresh non-fasting serum samples were analyzed at the Central Laboratory at Levanger hospital using a Hitachi 911 Autoanalyser (Mito, Japan). Iron concentrations were measured after reduction of transferrin with ascorbic acid, complexed with bathophenanthrolin and quantitated colorimetrically (Boehringer, Germany). TIBC was calculated from serum transferrin analyzed by immunoturbidimetric methodology from DAKO A/S, Denmark. The method was calibrated against the international standard CRM 470. Transferrin saturation percentage was calculated as 100 × (serum iron/2 × TIBC)%. Serum creatinine was analyzed using the Jaffé method (Roche Diagnostics, Germany). eGFR was estimated from recalibrated creatinine values using the Modification of Diet in Renal Disease (MDRD formula), as previously described [18].
Outcome ascertainment
Participants were followed up for BSI identified at the two hospitals (Levanger and Namsos) in Nord-Trøndelag county or at the tertiary referral center, St. Olavs hospital in Trondheim. We used BSI mortality as an indicator of risk of severe BSI and defined death from BSI as death occurring within 30 days after detection of a BSI. Outcome variables were first-time BSI and death from BSI. In participants with multiple positive blood cultures, a new episode of BSI was defined as positive blood culture > 30 days after the previous one. Blood cultures solely with microorganisms commonly associated with skin contamination such as coagulase negative Staphylococcus species, Corynebacterium species and Propionibacterium species were not considered as BSI [19].
Covariates
HUNT2 participants self-reported a range of chronic illnesses including cardiovascular disease (history of myocardial infarction, stroke and/or angina), lung disease (asthma or chronic obstructive pulmonary disease) and diabetes. Chronic kidney disease was defined as estimated glomerular filtration rate (eGFR) < 60 ml/min/1.73 m2. Body mass index (BMI) was calculated as weight (kg) divided by the squared value of height (m2) and categorized as recommended by WHO (< 18.5, 18.5–24.9, 25–29.9, 30.0–34.9, 35.0–39.9 and ≥ 40.0 kg/m2). We retrieved information on cancer diagnoses from the Cancer Registry of Norway for all patients with BSI (from 1 January 1953 until 1 January 2014). Information on rheumatic illnesses (e.g., rheumatoid arthritis, ankylosing spondylitis) and inflammatory bowel disease (e.g., ulcerative colitis, Crohn’s disease) was retrieved from medical records in patients with BSI. This information had been retrieved for 1216 BSI patients (68%); 1145 were BSI patients at Levanger hospital, and 111 of them had this diagnosis. Thus, the prevalence of rheumatic illness was 0.09%, which correlates with other prevalence studies [20, 21].
Statistical analyses
Levels of serum iron, Tsat and TIBC were categorized into values ≤ 2.5th percentile (low) or ≥ 97.5th percentile (high); the values in between were categorized into quintiles. The HUNT study population is representative of the Norwegian adult population, and we therefore based our iron values on the distribution in the entire cohort. For each category of iron indices, we used the Stata stcompadj command to estimate the age-adjusted cumulative incidence of first-time BSI, accounting for death as a competing risk. For each outcome, we used Cox regression analysis to estimate hazard ratios (HRs) with 95% confidence intervals (CIs) by categories of the iron indices using the middle quintile as reference. In the analysis of BSI risk, participants were followed until their first BSI, migration out of Nord-Trøndelag county, death or end of follow-up at 31 December 2011, whichever occurred first. In the analyses of BSI mortality, participants were followed until migration out of Nord-Trøndelag county, death or 31 December 2011, whichever occurred first. The proportional hazards assumption was examined using log-log plots and tests of Schoenfeld residuals. In a first model we adjusted for age (using attained age as the time scale) [22] and sex (by stratification). In a second model we additionally adjusted for BMI and chronic illnesses as these conditions may increase the risk of BSI [3], can cause “anemia of chronic disease” and altered iron status [23]. In a separate analysis, we omitted potentially cancer-related BSI from the outcome definition, indicated by a cancer diagnosis within 5 years prior to a BSI or 2 years after. Both cancer and cancer treatment could confound iron status and BSI risk. In a sensitivity analysis, we excluded the first 2 years of follow-up after HUNT2 participation from the follow-up to reduce possible confounding by prevalent but unknown disease at the time of serum measurements. Another sensitivity analysis was performed to investigate the impact of rheumatic illnesses and inflammatory bowel disease. We omitted BSI potentially related to this group of diseases from the outcome definition in 1145 cases of BSI at Levanger hospital, and Cox regression models were performed solely in participants having Levanger as their primary hospital (n = 43,280). All analyses were performed with Stata version 15.1 (Statacorp, Texas, USA).
Ethics
This study was approved by the Regional Committee for Medical and Health Research Ethics of Central Norway (REK no 2012/153), and all participants signed an informed consent.
Results
Among 61,852 participants, 1738 (2.9%) experienced at least one episode of BSI during median follow-up of 14.8 years, and 370 (0.6%) persons died from BSI. This corresponds to an incidence rate of 221/100,000 person-years and mortality rate of 47/100,000 person-years. Participants who experienced BSI were more likely to be male, older and obese (Table 1).
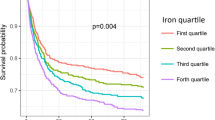
In age- and sex-adjusted analyses, BSI risk was increased among participants with indices of iron deficiency: low serum iron (HR 1.72, 95% CI 1.34–2.21), low Tsat (HR 1.48, 95% CI 1.12–1.96) or high TIBC (HR 1.46, 95% CI 1.06–2.01). The associations remained essentially similar after adjustments for BMI and chronic illnesses and also after exclusion of cancer-related BSI (n = 368) from the outcome definition (Table 2). In a sensitivity analysis where we omitted BSI-related rheumatic illnesses and inflammatory bowel disease (n = 111) from the outcome definition, the associations remained essentially similar (Supplementary Table 1). The results were also similar when we started follow-up 2 years after baseline (Supplementary Table 2), showing that the increased risk of BSI in iron-deficient subjects is not only present shortly after the time of diagnosis. The cumulative incidence curves also confirm that the excess risk at indices of iron deficiency continued throughout the follow-up period (Fig. 1). There was no association between indices of high iron levels and increased risk of BSI and no association between differences in iron status between the 2.5th and 97.5th percentiles and BSI risk (Table 2).
Analyses of BSI mortality showed similar associations as those we observed for a first-time BSI, but the low number of BSI deaths precluded precise estimates. Thus, age- and sex-adjusted BSI mortality was increased among participants with low serum iron (HR 1.52, 95% CI 0.86–2.66), low Tsat (HR 1.41, 95% CI 0.75–2.67) and high TIBC (HR 1.67, 95% CI 0.76–3.68), and the associations did not attenuate after adjustment for BMI and comorbidities (Table 3).
Discussion
In this large population-based cohort, indices of iron deficiency were associated with increased risk of a future BSI. Interestingly, individuals who were iron depleted continued to have an increased risk of BSI during a 15-year follow-up, even after adjusting for chronic medical disorders and excluding BSIs that occurred in relation to malignancies and chronic inflammatory disorders. To the best of our knowledge, our study is the first to show an increased risk of future BSI in individuals with iron depletion not related to cancers or chronic illnesses.
Former studies on the association between iron status and risk of infection have indicated a U-shaped risk profile where both iron deficiency and excess iron are linked to increased infection risk [7, 11]. To explore this hypothesis, we categorized our iron indices into quintiles using the middle quintile as reference and in the extreme ends ≤ 2.5th percentile or ≥ 97.5th percentile. A reason why we see no clear association between high iron status and risk of infection in our study could be that the low number of BSI cases in the high iron status categories precluded precise estimates of the associations between iron excess and increased risk of BSI. Moreover, all subjects with high iron status in HUNT2 were scheduled for further examinations, and those diagnosed with hereditary hemochromatosis were followed closely at the hospital for this condition thereafter.
In line with our findings, a systematic review reported that five out of six studies found higher occurrence of infections among patients with iron deficiency [24]. There are several plausible pathophysiologic explanations for an increased risk of BSI at low iron levels. Recent work has shown that iron plays a crucial role in the hypoxia-inducible-factor (HIF) transcription factor/prolyl hydroxylase domain pathway. HIFα induces a number of aspects of host immune function, from boosting phagocyte microbicidal capacity to driving T cell differentiation and cytotoxic activity [25]. Indeed, reduced T cell function [26], reduced bactericidal activity of macrophages [27] and decreased ability to produce inflammatory cytokines [28] have been shown in iron-depleted persons.
Our study suggests that the immune defense mechanisms may be relatively more depressed than the ability of bacteria to sequester iron in low iron environments, resulting in a net increased risk of BSI in iron-deficient individuals.
Major strengths of our study include its large size, the population-based design and long-term follow-up. Information on potential confounding factors such as chronic illnesses and malignancies, as well as linkage to microbiologic records, also add strength to our study. Moreover, in a sensitivity analysis we showed that the increased risk of BSI among iron-depleted subjects still was present after excluding the BSI events during the first 2 years of follow-up, which reduces the possibility that confounding from preclinical disease may explain the association and indicates that iron deficiency could be persistent in our subjects.
Iron status in the context of infection risk must take in account anemia of chronic disease, counting for 20% of anemias in the elderly (≥ 65 years) [29]. We have therefore adjusted for these confounding factors by adjusting for chronic illnesses, age and BMI, as these factors could influence both BSI risk and iron status [3, 23]. By retrieving data from the Cancer Registry of Norway, we also obtained valid and essentially complete information on cancer diagnoses among BSI cases. Importantly, the associations between low iron status and increased BSI risk remained similar after these adjustments. Also in sensitivity analyses leaving out patients with rheumatic illnesses and inflammatory bowel, we obtained similar results to the main analysis.
Linkage to microbial records with information on bacterial species enabled us to exclude pathogens commonly associated with contamination of blood cultures. The majority of positive blood cultures in this material are thus likely to represent serious infections. Although we did not have clinical information about the course of infection for all participants, a review of medical records of the patients with S. aureus and Streptococcus pneumoniae BSI in this cohort has shown that ~ 98% met the 2001 sepsis criteria [13, 14]. Thus, we find it likely that the patients with BSI clinically could be characterized as septic.
There are some limitations of our study. One is that our definition of BSI mortality as any death occurring within 30 days after detection of a BSI could be confounded by other causes of death not being related to the event of BSI. The lack of information on ferritin and hemoglobin concentrations is also a limitation. Ferritin is widely accepted as a standardized assessment of global iron stores, but is largely influenced by inflammation [30]. Hemoglobin concentration becomes abnormal only in long-standing iron deficiency and is influenced by a wide range of medical conditions [30]. Some studies have shown that Tsat or TIBC alone is an alternative diagnostic test for iron deficiency [31, 32]. We believe that our study has proved that serum iron, Tsat and TIBC, although prone to diurnal variation and fasting status, are useful for studying the association between iron metabolism and the future risk of BSI.
Another limitation is the one single measurement of the iron indices in our study and that we do not have measurements at the time when BSI was acquired. As iron status was measured up to 15 years before the outcome, it could have changed during the follow-up period, possible by later identification and correction by supplementation. However, any potential misclassification of iron indices caused by diurnal variation, non-fasting blood sampling or the single measurement would most likely be non-differential, i.e., not related to later risk of BSI, and is therefore likely to have led to underestimation of the associations. In nutritional surveys among adults from Norway during the same period as our study, the intake of iron was below the recommended daily amount [33], suggesting that iron deficiency was stable at the population level. A recent population study from Portugal found a high prevalence of iron deficiency and that it was largely undiagnosed [34].
Although our study adds weight to the growing body of evidence linking iron deficiency and risk of infections, we should be careful recommending iron supplements in individuals with mild-to-moderate iron deficiency to prevent infections. While there are studies suggesting that iron supplementation may decrease the risk for some infections [35], a recent systematic review showed increased susceptibility to infections with intravenous versus oral or no iron administration [36]. The controversies shown in iron supplemental studies demonstrate how delicate iron homeostasis is and that iron supplement should be given with caution.
In summary, we show an increased risk of BSI in individuals with low iron status in a 15-year follow-up study. As iron deficiency and BSI represent an important burden of disease globally, our findings suggest increased research on the effect of identifying and correcting iron deficiency to prevent BSI and sepsis.
References
Cohen J, Vincent JL, Adhikari NK, Machado FR, Angus DC et al (2015) Sepsis: a roadmap for future research. Lancet Infect Dis 15:581–614
Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M et al (2017) Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med 43:304–377
Henriksen DP, Pottegard A, Laursen CB, Jensen TG, Hallas J et al (2015) Risk factors for hospitalization due to community-acquired sepsis—a population-based case-control study. PLoS One 10:e0124838
Paulsen J, Askim A, Mohus RM, Mehl A, Dewan A et al (2017) Associations of obesity and lifestyle with the risk and mortality of bloodstream infection in a general population: a 15-year follow-up of 64 027 individuals in the HUNT Study. Int J Epidemiol 46:1573–1581
Wang HE, Shapiro NI, Griffin R, Safford MM, Judd S et al (2012) Chronic medical conditions and risk of sepsis. PLoS One 7:e48307
Reddick LE, Alto NM (2014) Bacteria fighting back: how pathogens target and subvert the host innate immune system. Mol Cell 54:321–328
Ganz T, Nemeth E (2015) Iron homeostasis in host defence and inflammation. Nat Rev Immunol 15:500–510
Perner A, Gordon AC, De Backer D, Dimopoulos G, Russell JA et al (2016) Sepsis: frontiers in diagnosis, resuscitation and antibiotic therapy. Intensive Care Med 42:1958–1969
Hussain SQ, Ashraf M, Wani JG, Ahmed J (2014) Low hemoglobin level a risk factor for acute lower respiratory tract infections (ALRTI) in children. J Clin Diag Res 8:Pc01–Pc03
Gwamaka M, Kurtis JD, Sorensen BE, Holte S, Morrison R et al (2012) Iron deficiency protects against severe Plasmodium falciparum malaria and death in young children. Clin Infect Dis 54:1137–1144
Drakesmith H, Prentice AM (2012) Hepcidin and the iron-infection axis. Science 338:768–772
Bassetti M, Poulakou G, Ruppe E, Bouza E, Van Hal SJ et al (2017) Antimicrobial resistance in the next 30 years, humankind, bugs and drugs: a visionary approach. Intensive Care Med 43:1464–1475
Askim A, Mehl A, Paulsen J, DeWan AT, Vestrheim DF et al (2016) Epidemiology and outcome of sepsis in adult patients with Streptococcus pneumoniae infection in a Norwegian county 1993–2011: an observational study. BMC Infect Dis 16:223
Paulsen J, Mehl A, Askim A, Solligard E, Asvold BO et al (2015) Epidemiology and outcome of Staphylococcus aureus bloodstream infection and sepsis in a Norwegian county 1996–2011: an observational study. BMC Infect Dis 15:116
Mohus RM, Askim Å, Paulsen J, Mehl A, Dewan A et al (2016) Association of iron status and risk of bloodstream infections in a general Norwegian population. The HUNT study. ESICM. https://services.y-congress.com/mediatheque/app/esicm/media.html?home_page_uri=posters.html¤t_section=null&mediaId=21856&channel=16552. Accessed 15 June 2018
Krokstad S, Langhammer A, Hveem K, Holmen TL, Midthjell K et al (2013) Cohort Profile: the HUNT study, Norway. Int J Epidemiol 42:968–977
Holmen JM, Krüger K, Langhammer Ø, Holmen A, Bratberg TL et al (2003) The Nord-Trøndelag Health Study 1995–97 (HUNT 2): objectives, contents, methods and participation. Norsk Epidemilogi 13:14
Hallan S, Astor B, Lydersen S (2006) Estimating glomerular filtration rate in the general population: the second Health Survey of Nord-Trondelag (HUNT II). Nephrol Dial Transplant 21:1525–1533
Hall KK, Lyman JA (2006) Updated review of blood culture contamination. Clin Microbiol Rev 19:788–802
Ihlebaek C, Brage S, Natvig B, Bruusgaard D (2010) Occurrence of musculoskeletal disorders in Norway. Tidsskr Nor Legeforen 130:2365–2368
Ng SC, Shi HY, Hamidi N, Underwood FE, Tang W et al (2018) Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet 390:2769–2778
Thiebaut AC, Benichou J (2004) Choice of time-scale in Cox’s model analysis of epidemiologic cohort data: a simulation study. Stat Med 23:3803–3820
Weiss G, Goodnough LT (2005) Anemia of chronic disease. N Engl J Med 352:1011–1023
Tansarli GS, Karageorgopoulos DE, Kapaskelis A, Gkegkes I, Falagas ME (2013) Iron deficiency and susceptibility to infections: evaluation of the clinical evidence. Eur J Clin Microbiol Infect Dis 32:1253–1258
Palazon A, Goldrath A, Nizet V, Johnson RS (2014) HIF transcription factors, inflammation, and immunity. Immunity 41:518–528
Jonker FA, Boele van Hensbroek M (2014) Anaemia, iron deficiency and susceptibility to infections. J Infect 69(Suppl 1):S23–S27
Ekiz C, Agaoglu L, Karakas Z, Gurel N, Yalcin I (2005) The effect of iron deficiency anemia on the function of the immune system. Hematol J 5:579–583
Sipahi T, Akar N, Egin Y, Cin S (1998) Serum interleukin-2 and interleukin-6 levels in iron deficiency anemia. Pediatr Hematol Oncol 15:69–73
Guralnik JM, Eisenstaedt RS, Ferrucci L, Klein HG, Woodman RC (2004) Prevalence of anemia in persons 65 years and older in the United States: evidence for a high rate of unexplained anemia. Blood 104:2263–2268
Lopez A, Cacoub P, Macdougall IC, Peyrin-Biroulet L (2016) Iron deficiency anaemia. Lancet 387:907–916
Peyrin-Biroulet L, Williet N, Cacoub P (2015) Guidelines on the diagnosis and treatment of iron deficiency across indications: a systematic review. Am J Clin Nutr 102:1585–1594
Hawkins RC (2007) Total iron binding capacity or transferrin concentration alone outperforms iron and saturation indices in predicting iron deficiency. Clin Chim Acta 380:203–207
Johansson L, Solvoll K (1999) Norkost 1997 Landsomfattende kostholdsundersøkelse blant menn og kvinner i alderen 16-79 år. Statens ernæringsråd 2:1–84
Fonseca C, Marques F, Robalo Nunes A, Belo A et al (2016) Prevalence of anaemia and iron deficiency in Portugal: the EMPIRE study. Intern Med J 46:470–478
de Silva A, Atukorala S, Weerasinghe I, Ahluwalia N (2003) Iron supplementation improves iron status and reduces morbidity in children with or without upper respiratory tract infections: a randomized controlled study in Colombo, Sri Lanka. Am J Clin Nutr 77:234–241
Litton E, Xiao J, Ho KM (2013) Safety and efficacy of intravenous iron therapy in reducing requirement for allogeneic blood transfusion: systematic review and meta-analysis of randomised clinical trials. BMJ 347:f4822
Acknowledgements
The Nord-Trøndelag Health Study (the HUNT study) is a collaboration of the HUNT research center (Faculty of Medicine, NTNU), Nord-Trøndelag County Council, Central Norway Health Authority and the Norwegian Institute of Public Health. We sincerely thank the microbiology departments of Levanger, Namsos and St. Olavs hospitals for providing microbial data and the Department for Research at Nord-Trøndelag Hospital Trust for assistance with data linkage.
Funding
This work was supported by a grant from The Liaison Committee for education, research and innovation in Central Norway.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
Nothing to declare.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mohus, R.M., Paulsen, J., Gustad, L. et al. Association of iron status with the risk of bloodstream infections: results from the prospective population-based HUNT Study in Norway. Intensive Care Med 44, 1276–1283 (2018). https://doi.org/10.1007/s00134-018-5320-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-018-5320-8