Abstract
Purpose
To identify, evaluate and synthesise studies examining the barriers and enablers for survivors of critical illness to participate in physical activity in the ICU and post-ICU settings from the perspective of patients, caregivers and healthcare providers.
Methods
Systematic review of articles using five electronic databases: MEDLINE, CINAHL, EMBASE, Cochrane Library, Scopus. Quantitative and qualitative studies that were published in English in a peer-reviewed journal and assessed barriers or enablers for survivors of critical illness to perform physical activity were included. Prospero ID: CRD42016035454.
Results
Eighty-nine papers were included. Five major themes and 28 sub-themes were identified, encompassing: (1) patient physical and psychological capability to perform physical activity, including delirium, sedation, illness severity, comorbidities, weakness, anxiety, confidence and motivation; (2) safety influences, including physiological stability and concern for lines, e.g. risk of dislodgement; (3) culture and team influences, including leadership, interprofessional communication, administrative buy-in, clinician expertise and knowledge; (4) motivation and beliefs regarding the benefits/risks; and (5) environmental influences, including funding, access to rehabilitation programs, staffing and equipment.
Conclusions
The main barriers identified were patient physical and psychological capability to perform physical activity, safety concerns, lack of leadership and ICU culture of mobility, lack of interprofessional communication, expertise and knowledge, and lack of staffing/equipment and funding to provide rehabilitation programs. Barriers and enablers are multidimensional and span diverse factors. The majority of these barriers are modifiable and can be targeted in future clinical practice.
Similar content being viewed by others
Introduction
Survivorship following critical illness results in significant morbidity in terms of long-lasting post-ICU physical, cognitive and mental health morbidity [1]. Muscle weakness and impaired physical functioning are key limitations, which impact on a patient’s return to work and quality of life. Exercise and physical activity (as an intervention) is safe, feasible and potentially efficacious in survivors of critical illness at improving patient outcomes especially when applied early in the ICU [2, 3]. Physical activity (PA) is defined as “bodily movement produced by skeletal muscles that results in energy expenditure” [4]. It encompasses mobilisation, exercise training, rehabilitation and general activities of daily living. Despite supportive practice guidelines [5, 6], international point prevalence studies have demonstrated that low PA levels exist in the ICU [7–9]. A current gap exists between the perceived need and desire to enhance PA levels and actual implementation of PA interventions into routine care.
Recent publications have profiled barriers to early mobilisation specifically in the ICU setting, existing both at the patient and hospital level [10, 11]. However, a broader understanding of the specific barriers is needed. Such data are highly relevant to inform changes in clinical practice, service delivery, policy and research aiming to enhance PA levels and survivorship outcomes. The aim of this review is to evaluate studies examining the barriers and enablers for survivors of critical illness to participate in PA in the ICU and post-ICU setting from the perspective of patients, caregivers and healthcare providers (HCPs). We hypothesize that the barriers and enablers will be diverse and multifactorial at the patient, healthcare provider and institutional level. This research was presented at the European Society of Intensive Care Medicine Conference in 2016 with associated published abstract [12].
Methods
Guidelines and protocol registration
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines [13] and Enhanced Transparency of Reporting the Synthesis of Qualitative Research framework [14] guided this review. The protocol was registered on PROSPERO (CRD42016035454).
Eligibility criteria
Studies assessing barriers or enablers to individuals with critical illness participating in PA interventions were included (and could be from the perspective of the patient, caregiver or HCP) (Table 1).
Information sources and search
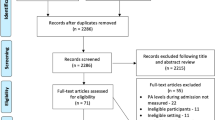
Five electronic databases (Fig. 1) were searched by one reviewer (SP) using a pre-planned systematic comprehensive and reproducible search strategy (ETable 1) to identify all published studies against defined eligibility criteria. Databases were accessed via The University of Melbourne and the last search was run on 26 December 2016.
PRISMA flow diagram of study selection process [13]. CINAHL Cumulative Index to Nursing and Allied Health Literature, EMBASE the Excerpta Medica Database
Study selection
Eligibility assessment was performed in a standardised manner. Two independent reviewers (SP, LK) screened titles, abstracts and full-text articles (Fig. 1) against defined eligibility criteria (Table 1). Disagreement was resolved by consensus with a third reviewer (CG) when needed.
Data collection process and data items
Data extraction was independently performed by two authors (BC, JM) for quantitative studies using bespoke data collection forms, and cross-checked by a second (CB, LK). Data items included author details, year published, aims, study design, methods, participant characteristics and results (including barriers and enablers to PA). For qualitative studies all text under the headings ‘results/conclusions’ was extracted manually by two independent reviewers (SP, CG) and cross-checked.
Risk of bias in individual studies
Independent reviewers (SP, CG) assessed the quality of the quantitative evidence using the Oxford Centre for Evidence-based Medicine scale for rating of individual studies. Qualitative studies were assessed using the consolidated criteria for reporting qualitative research (COREQ) checklist [15]. Results of studies were given the same weight regardless of their assessed risk of bias.
Synthesis of results
A meta-analysis was not possible because of the heterogeneity in study design and measures. Quantitative data on barriers and enablers to PA were synthesised using thematic synthesis [16]. Two independent reviewers (SP, CG) performed line-by-line coding of text from the qualitative studies, and similar concepts were grouped and new codes developed when necessary. Free codes were organised into descriptive major themes and sub-themes using an inductive approach [16]. Discrepancies were discussed between reviewers and consensus was achieved on all occasions. A third reviewer (CB) cross-checked the data to ensure the relevant data was accurately captured and integrated into appropriate themes (CB).
Results
Study selection and characteristics
A total of 4122 studies were screened resulting in the final inclusion of 89 papers (ETable 4), including 77 quantitative (87%) and 12 qualitative (13%) studies (ETable 4). Studies were conducted in 11 different countries (ETable 2); the most common were USA (n = 54, 61%); Australia (n = 13, 15%) and UK (n = 10, 11%). Overall, 17,547 patients, 4425 HCPs and 56 caregivers were included in this review. The majority of papers (93%, n = 83) were focused on the ICU setting alone, with only 7% focused on assessing barriers or enablers in the post-ICU setting. Over half (55%) of included studies were published since 2014.
Quality assessment of included studies
The majority of included quantitative studies were either case series with or without intervention or cross-sectional study (n = 48/77, 62%) (ETable 4). Qualitative studies scored poorly for lack of reporting of the interviewer’s characteristics and relationship between interviewers and participants within Domain 1 ‘Team and Reflexivity’. The median [interquartile] score for qualitative studies was 21 [11–22], ETable 5.
Synthesis of results
Five major themes and 28 sub-themes for barriers and enablers to PA were identified across the 89 papers included (Fig. 2, ETable 3). Quotes from primary qualitative studies are provided to reflect themes. Each theme will now be discussed descriptively. The relevant sub-themes for each theme are summarised in ETable 3; please refer to this for further detail.
Summary of findings—themes influencing delivery of physical activity in patients with critical illness. This figure highlights the five themes and 28 sub-themes that were identified in this systematic review. admin administrative, Dx diagnosis, ETT endotracheal tube, HCPs healthcare providers, QI quality improvement, MV mechanical ventilation, rehab rehabilitation
Theme 1: patient physical and psychological influences
There was conflicting evidence for the association between illness severity, age, weight and presence of comorbidities and receipt of rehabilitation in the ICU (ETable 3). Symptoms of pain, fatigue and weakness were identified as barriers to PA [8, 9, 17–21]. Fatigue and patient refusal were common reasons for early cessation or lack of PA [17, 18, 22–26] and weakness was a common barrier to mobilisation [8, 9, 20].
Sedation was a frequently identified barrier in the ICU [8, 9, 17, 19–21, 23–25, 27–41]. Other barriers included agitation [8, 20, 23, 25, 42], delirium [18, 21, 33, 34, 37] and patient alertness [8, 26, 27, 36, 42]. Studies found that sedation, delirium and alertness influenced the patient’s ability to engage in PA [7, 43]. Early PA was facilitated when combined with good sedation and delirium practice and in some studies this occurred as part of the awakening and breathing coordination, delirium monitoring and management, early mobility (ABCDE) bundle [21, 34, 44–47]. Adequate sleep was recognised as a facilitator for patient engagement in PA [48]. Physiotherapists identified patient anxiety, fear, lack of motivation, confidence, and patient knowledge about ICU-acquired weakness (ICUAW) as factors impeding adherence to interventions [43]. Gaining patient trust, setting goals with the patient, addressing anxiety concerns and involving caregivers were recognised as enablers [41].
Theme 2: safety influences
Haemodynamic and respiratory physiological stability were significant influences [8, 9, 17–22, 24, 25, 27, 33, 39, 42, 49–52]. Medical contraindications, complications and medical procedures/investigations were barriers and contributed to missed therapy sessions, particularly in the ICU [9, 17, 18, 24, 49]. The development of physiological stability guidelines for rehabilitation was an enabler [21, 33].
Safety concerns regarding lines were perceived as a barrier to mobilisation [19, 21, 24, 27, 31, 33, 53], in particular the presence of pulmonary artery catheters [20, 53], femoral lines [18, 20, 42] or haemodialysis [7, 17, 18, 30, 51].
However, several studies specifically reported the safety of PA with lines in situ and found no adverse events [54–58]. In one study physiotherapists and nursing staff identified unnecessary lines and poor choice of line location as barriers [41]. Planning to ensure device and line securement was an identified enabler [21].
“The position of certain lines is frustrating, for example when the vascaths have been inserted femorally and you are ready to start them sitting, its just basic planning.” [41]
Presence of an endotracheal tube (ETT) was a common barrier to mobilisation [7, 17, 20, 24]. Commonly reported barriers to mobilising mechanically ventilated (MV) patients included time required, concerns for airway dislodgement, risk of physiological instability, concomitant sedation and delirium [9, 36, 42, 52]. Concern for patient [21, 22, 27, 33, 44, 45, 52, 59], staff [37] and caregiver [44] safety was a consideration; and both nurses and physiotherapists noted concern for their own safety (risk of musculoskeletal injury) was a barrier to out-of-bed activities [37].
Theme 3: culture and team influences
Barriers to PA included cultural/traditional practices [33, 41, 59], staff attitudes [19], resistance to change [34], staff morale [60] and lack of interprofessional respect [60]. Factors which facilitated culture change to enable increased PA included need for clinician belief in the importance of rehabilitation and commitment to changing practice; team-building meetings; shared performance data emphasising evidence and safety; active multidisciplinary collaboration and training [22, 45, 46, 48, 59, 60]. The inclusion of visible goal targets positively influenced mobilisation levels [46]. Staff were also motivated by seeing patients mobilising and challenging themselves [61]. The need to overcome family perceptions that patients were too sick for rehabilitation was also identified as a potential enabler [59].
“If you get buy-in from all of the different disciplines, its definitely easy. If you’re a rehab team who wants to do this and you don’t have buy-in by your nurses and physicians and respiratory, it’s not gonna happen.” [45]
Lack of interprofessional communication [41, 60, 62] and coordination [25] were barriers and the reverse was an enabler [34, 45, 59]. Enabling strategies included daily ward rounds to discuss mobility [19, 44, 62], rounding checklists [60], team meetings [45], documented PA goals [26, 41, 44], prompts and continuous feedback on outcomes to the team [19, 34, 60, 61]. Communication difficulties with ventilated patients led to frustration, anxiety and poor adherence from the patient in relation to engagement in PA [43].
“Communication and teamwork are probably the biggest things.” [45]
Absence of leadership and champions of PA was a barrier [21, 25] and designation of an overall leader and discipline champions was an enabler [21, 27, 33, 34, 45, 59, 60, 62].
“You need…strong advocates or champions in multiple disciplines. I think having a champion—someone who is really pushing it through, pushing it forward especially on the physician side of things—makes a big difference.” [45]
Role clarity and accountability were highlighted as enablers, and lack of role delineation was a barrier to PA [25, 41, 60, 61]. All staff believed mobility could not be carried out by one discipline and the importance of the MDT and role clarification was highly emphasised [33, 45, 61]. Physiotherapists were identified as instrumental members of this team [59]. Lack of knowledge and training was a barrier across the multidisciplinary team [19, 21, 22, 33, 34, 40, 41, 60, 62] and enablers included education about the benefits of PA, addressing safety concerns, site visits to successful programs and benchmarking against other programs [21, 33, 41, 45, 46, 59–63].
Theme 4: motivation and beliefs about physical activity—from patients, family and HCPs
Patients reported experiencing a number of positive outcomes associated with PA. These included improved physical and psychological outcomes, reduced boredom and isolation, and expressed enjoyment and satisfaction in participating in PA programs [64, 65] all of which were seen as enablers. Patients who underwent inpatient PA programs wanted to continue post discharge, as they believed it was an important part of their recovery [66]. Patients reported feeling cared about and supported by staff and an increased ability to be self-reliant as a result of participating in a supervised outpatient PA program [64].
“A sense of achievement…every time you went…” [64]
However those exposed to an outpatient pulmonary rehabilitation model felt it was not specific to their needs as survivors of critical illness [67].
Caregivers felt that PA was extremely necessary and beneficial and rated the necessity of physiotherapy higher than patients did themselves [68]. However, they underestimated the enjoyment and overestimated the level of difficulty of PA in the ICU as reported by patients [68]. Caregivers also perceived PA to be less beneficial in individuals who had been MV for more than 2 weeks, but caregivers did not want less therapy to be provided [68].
Healthcare providers expected or had experienced positive clinical outcomes from their patients being active [43, 45, 52, 53]. These included improved physical and psychological outcomes [43, 45, 52, 53]; reduced delirium and improved sleep [45] and both reduced MV duration and hospital and ICU length of stay [45, 52]. Consistently across studies there was an overwhelming belief by HCPs that increased PA was beneficial [26, 43, 45, 52, 53]. Staff satisfaction due to feeling responsible for improving patient outcomes with PA was an enabler [45].
“Physical therapy and occupational therapy have shown that it shortened length of stay. It has helped get patients off the ventilator more quickly, even get them out of the ICU more quickly…” [45]
“To see those small improvements in a patient creates a lot of job satisfaction…a rewarding feeling.” [45]
In some studies HCPs reported the perception that there was limited evidence and importance to justify increased PA [33, 40, 46]. Two studies also reported staff scepticism and lack of awareness of longer-term impact of critical illness [33, 46]. There were conflicting views on the benefits of PA in individuals who were MV, in particular the role of mobilisation whilst MV with an ETT, with concerns that the risks outweighed potential benefits for this subgroup [37, 52, 62].
Theme 5: environmental influences
In the ICU setting lack off, or presence of, automatic referral for physiotherapy was a barrier or enabler in some countries [19, 22, 25, 33, 37, 40, 41, 59, 69]. The importance of managerial support and funding for staff resources and to support protocol change was highlighted [41, 45, 46, 70].
“If the hospital doesn’t buy the idea that mobilisation in the ICU is useful, then we won’t be able to do it.” [45]
The type of ICU the patient was in (i.e. respiratory versus medical, trauma; proactive mobility unit) was identified as an enabler for some patient groups in some studies [30, 46]. In different units this may be reflective of the culture; significant factors which were in favour of out-of-bed PA included large volume ICUs, academic and presence of advanced care providers in one study [36], but favoured community providers in another study [71]. Limited or increased access to PA equipment and/or other resources was identified as a barrier [17, 19, 21, 22, 24, 26, 33, 34, 40, 44, 60] and enabler [21, 33], respectively. It has also been reported that available equipment was not associated with out-of-bed activities [27] and that minimum (rather than specialised) equipment is sufficient [45].
“You need a certain amount of equipment, basic equipment…fundamental resources. You don’t need bells and whistles.” [45]
Time and competing priorities were raised frequently as barriers and often led to lower prioritisation compared to other daily care needs, particularly in the ICU setting [8, 17–19, 23, 25, 27, 29, 31, 37, 40–42, 44, 49, 72–74].
The presence of a mobility protocol and/or mobility teams strongly facilitated PA [9, 22, 37, 39, 44, 73, 74] and lack of clear recommendations was a key barrier [73, 74]. In addition the implementation of quality improvement projects to develop/implement a mobility program or protocol was an enabler to PA in a number of studies across different settings internationally [19, 21, 25, 31, 33, 34, 60–62, 69, 75–78].
Lack of funding was a significant barrier particularly for outpatient PA programs [26, 46, 70]. There was a strong message from patients for the wish to continue rehabilitation after discharge home, and delay to receive rehabilitation was frustrating [64, 66]. Other patients reported severe challenges in accessing services [64, 79]. Patients who did access PA programs after hospital discharge responded positively to bright and cheerful environments, use of music, and access to clinicians knowledgeable on ICU-specific issues [65]. Preference for group exercise was seen, albeit in small patient numbers [64].
“It was something else that I had to contend with on top of trying to get better.” [64]
“I felt there was about a two week delay for his rehabilitation to start. And the reason I’m emphasizing on the delay is because two weeks after an ICU stay for a survivor is a long, long time.” [66]
Lack of dedicated staffing (especially at weekends), workload burden and willingness were barriers, and these were a consistent issue in the ICU and post-ICU settings [19, 21, 22, 26, 29, 31–33, 37, 40, 44, 45, 59, 60, 62, 70]. Presence of a dedicated rehabilitation team was one of the most important enabling factors identified [31, 41, 45, 60].
“In the end sometimes they’re just left in bed because I can’t get a second pair of hands.” [41]
In the absence of increased funding or staffing, two studies reported the possibility of achieving improved patient outcomes through restructuring of roles, responsibilities and care pathways [25, 46]. However it is not clear whether staffing levels are associated with mobility activities, with conflicting results from two studies [7, 27].
Discussion
In the largest body of research synthesised to date on this topic we have identified that the barriers to PA for survivors of critical illness are diverse and span five major themes: (1) patient physical and psychological influences; (2) safety influences; (3) culture and team influences; (4) motivations and beliefs regarding the benefits and risks of PA; and (5) environmental influences. Our review is unique in that we have examined this issue across the care pathway from ICU to community. Many of the barriers and enablers identified were consistent across both quantitative and qualitative study design and across different geographical settings worldwide, thus improving the generalizability of findings. Our results are consistent with previous research investigating barriers specifically in the ICU setting [10], and extend our understanding of the challenges in both the ICU and post-ICU settings. We have identified a number of potentially modifiable barriers and a variety of enablers, which need to be targeted to inform future research, clinical practice, service delivery and policy to improve survivorship outcomes (Fig. 3).
Barriers and enablers to delivery of physical activity interventions in individuals with critical illness. ABCDE awakening and breathing coordination, delirium monitoring and management, early mobility, est established, HCP healthcare provider, MDT, multidisciplinary, PA physical activity, Pt patient. This figure provides an overview of the identified barriers and enablers across the 89 papers included in this review. The barriers highlighted in bold are modifiable barriers which can be targeted in specific interventions and policies to improve delivery of PA interventions in individuals with critical illness
Upon reflection of the main barriers identified in this review a central enabling factor across both the ICU and post-ICU setting which needs to be addressed is knowledge transfer and education of HCPs, patients and caregivers. This education includes the need to raise awareness of the burden and impact of post-intensive care syndrome, and the importance and benefit of PA interventions commencing early and continuing post discharge from the ICU setting. Expertise development and skill training to equip the clinicians to undertake successful PA interventions are also required.
Behavioural change and translation research models need to be explored to identify potential interventions and policies which can be targeted to increase PA levels in survivors of critical illness [80]. There are a variety of different models that currently exist and could be adopted in the clinical setting to improve implementation of PA interventions. For the purposes of this review we will discuss one model known as the COM-B model (capability, opportunity, motivation-behaviour) which is frequently utilised to facilitate evidence translation and development of interventions to change behaviour, in this instance healthcare or patient behaviour [80]. The model can assist in identifying specific intervention strategies and supporting policies to solidify behaviour change based on the identified ‘barrier’ sources of behaviour. To our knowledge this specific behavioural change model has not been used in the ICU literature previously, and our data offer a roadmap for effective improvements in engagement and delivery of PA-based interventions. To change behaviour, one or multiple aspects of the COM-B model can be targeted [80]. For example, identified capability-related barriers included physical (symptoms, illness severity, delirium, weakness) and psychological (anxiety, lack of confidence) factors; opportunity-related barriers included lack of access to services (staffing and equipment) and competing priorities; and motivation-related barriers included fear of PA, perceived importance and unit culture practices (Fig. 4). In contrast enablers for PA mapped to the COM-B domains included good sedation and delirium management, safety frameworks, adoption of ABCDE bundles (capability); development of mobility daily care plans, team meetings, administration buy-in, creation of leadership and ‘mobility’ champions/protocols (opportunity); and anticipated benefits from PA (motivation). Based on this framework and our results, potential interventions may include education (of patients, caregivers and HCPs), persuasion (of HCPs and patients) of the importance and need for PA interventions, environmental restructuring, modelling and enablement [80]. Future research and clinical practice need to focus on educational models, which can be implemented for HCPs across the MDT and consumers (patients and caregivers). This includes integration of education about PA for survivors of critical illness into both university curricula and clinical training to enable greater understanding of the importance of engagement and MDT collaboration in PA interventions; and to equip the MDT with the necessary skills and expertise to engage patients in PA in the ICU and post-ICU settings. It is also important that the general public awareness of the burden of ICU survivorship and importance of PA is raised, and greater engagement from patients and caregivers to understand and develop feasible and realistic PA-based interventions is required.
We found many transferrable positive examples of quality improvement projects where individual health services or groups have gone through an implementation process to examine local institutional barriers and enablers. A site-by-site or service-by-service approach to implement PA across the care continuum is likely needed, based on individual variation of barriers and enablers, which may be affected by a disparity between perceived and actual barriers. It is clear that a team-based approach with both bottom-up (discipline champions, knowledge and skills of HCPs, patients and caregivers) and top-down support (managerial/hospital support) is key to affecting change.
Barriers and enablers need to be additionally considered across the trajectory of recovery. Several studies highlighted that there is a significant gap in access to rehabilitation post ICU [26, 46, 67]. The majority of studies included in this review focused on the ICU setting alone; there is a greater need to understand the changing barriers for individuals following critical illness once they leave the hospital setting to reintegrate into the community setting. From the studies which examined post ICU it appears that patients may prefer individualised rehabilitation based on illness trajectory rather than being included in a generic or even respiratory-specific rehabilitation program such as pulmonary rehabilitation [67]. Methods to deliver PA programs within existing infrastructure to utilise resources more efficiently should be explored. We should also consider low-cost, high-efficacy interventions such as telemonitoring and telephone-based interventions to increase community PA levels, which are being investigated in other patient populations [81].
Critique of the method
This review is strengthened by inclusion of qualitative and quantitative data. Qualitative data enriches our understanding of subjective influences, which are not captured within quantitative methodologies. We followed a robust protocol that was registered a priori, adopted review guidelines, and incorporated duplicate screening and data extraction to enhance review rigour. However there are several limitations with this review: our results were presented using thematic analysis, and thus did not rate or weight the barriers and enablers in terms of frequency of occurrence because of the differences in study design and methodologies across included studies. There is a risk of publication bias in this review as we only included studies published in English in a peer-reviewed journal. All studies were included regardless of risk of bias and thus results should be interpreted with caution. Future directions include understanding why the identified barriers in this review exist and examining whether the adoption of behavioural change or translational models to provide targeted interventions to address these barriers is effective in improving patient engagement in PA interventions in the ICU and post-ICU setting.
Conclusion
Barriers and enablers to PA in patients with critical illness are multidimensional and span diverse factors. Considering these factors in a structured behavioural change framework has elucidated potential strategies for enhancing interventions, clinical service delivery and policy frameworks to increase PA in patients with critical illness.
Abbreviations
- ABCDE:
-
Awakening and breathing coordination, delirium monitoring and management, early mobility
- COM-B:
-
Capability, opportunity, motivation behavioural change wheel
- COREQ:
-
Consolidated criteria for reporting qualitative studies
- ECMO:
-
Extracorporeal membrane oxygenation
- ENTREQ:
-
Enhancing transparency in reporting the synthesis of qualitative research
- HCP:
-
Healthcare provider
- ICU:
-
Intensive care unit
- ICUAW:
-
Intensive care unit acquired weakness
- MDT:
-
Multidisciplinary team
- MV:
-
Mechanical ventilation
- NOS:
-
Newcastle Ottawa scale
- PA:
-
Physical activity
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
- QI:
-
Quality improvement
References
Herridge MS, Moss M, Hough CL, Hopkins RO, Rice TW, Bienvenu OJ, Azoulay E (2016) Recovery and outcomes after the acute respiratory distress syndrome (ARDS) in patients and their family caregivers. Intensive Care Med 42(5):725–738
Kayambu G, Boots R, Paratz J (2013) Physical therapy for the critically ill in the ICU: a systematic review and meta-analysis. Crit Care Med 41(6):1543–1554
Hashem M, Nelliot A, Needham D (2016) Early mobilization and rehabilitation in the ICU: moving back to the future. Respir Care 61(7):971–979
Caspersen CJ, Powell KE, Christenson GM (1985) Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep 100(2):126–131
National Institute for Health and Clinical Excellence (2009) Rehabilitation after critical illness. NICE clinical guideline, vol 83. National Institute for Health and Clinical Excellence, Manchester
Berry A, Beattie K, Bennett J, Cross , Cushway S, Hassan A, Longhurst E, Moore R, Phillips D, Plowman E, Scott J, Thomas L, Elliott D (2014) Physical activity and movement: a guideline for critically ill adults, in SHPN. Agency for Clinical Innovation, Chatswood
Berney SC, Rose JW, Bernhardt J, Denehy L (2015) Prospective observation of physical activity in critically ill patients who were intubated for more than 48 hours. J Crit Care 30(4):658–663
Berney S, Harrold M, Webb S, Seppelt I, Patman S, Thomas P, Denehy L (2013) Intensive care unit mobility practices in Australia and New Zealand: a point prevalence study. Crit Care Resusc 15(4):260–265
Nydahl P, Ruhl A, Bartoszek G, Dubb R, Filipovic S, Flohr H-J, Kaltwasser A, Mende H, Rothaug O, Schuchhardt D, Schwabbauer N, Needham D (2014) Early mobilization of mechanically ventilated patients: a 1-day point-prevalence study in Germany. Crit Care Med 42(5):1178–1186
Dubb R, Nydahl P, Hermes C, Schwabbauer N, Toonstra A, Parker Kaltwasser A, Needham D (2016) Barriers and strategies for early mobilization in intensive care units. Ann Am Thorac Soc 36:2238–2243
Honiden S, Connors G (2015) Barriers and challenges to the successful implementation of an intensive care unit mobility program: understanding systems and human factors in search for practical solutions. Clin Chest Med 36(3):431–440
Parry SM et al (2016) What are the factors that impact on physical activity and rehabilitation for survivors of critical illness: A systematic review of quantitative and qualitative studies. Intensive Care Med Exp 4 (Suppl 1): A40
Moher D, Liberati A, Tetzlaff J, Altman D, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097. doi:10.1371/journal.pmed.1000097
Tong A, Flemming K, McInnes E, Oliver S, Craig J (2012) Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol 12(181):1–8
Tong A, Sainsbury P, Craig J (2007) Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 19(6):349–357
Thomas J, Harden A (2008) Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol 8:45
Harrold M, Salisbury L, Webb S, Allison G (2015) Early mobilisation in intensive care units in Australia and Scotland: a prospective, observational cohort study examining mobilisation practises and barriers. Crit Care 19(1):336
Pohlman M, Schweickert W, Pohlman A, Nigos C, Pawlik A, Esbrook C, Spears L, Miller M, Franczyk M, Deprizio D, Schmidt G, Bowman A, Barr R, McCallister K, Hall J, Kress J (2010) Feasibility of physical and occupational therapy beginning from initiation of mechanical ventilation. Crit Care Med 38(11):2089–2094
Castro E, Turcinovic M, Platz J, Law I (2015) Early mobilization: changing the mindset. Criti Care Nurs 35(4):e1–e5
TEAM Study Investigators, Hodgson C, Bellomo R, Berney S, Bailey M, Buhr H, Denehy L, Harrold M, Higgins A, Presneill J, Saxena M, Skinner E, Young P, Webb S (2015) Early mobilization and recovery in mechanically ventilated patients in the ICU: a bi-national, multi-centre, prospective cohort study. Crit Care 19:81
Needham D, Korupolu R (2010) Rehabilitation quality improvement in an intensive care unit setting: implementation of a quality improvement model. Topic Stroke Rehabil 17(4):271–281
Morris P, Goad A, Thompson C, Taylor K, Harry B, Passmore L, Ross A, Anderson L, Baker S, Sanchez M, Penley L, Howard A, Dixon L, Leach S, Small R, Hite R, Haponik E (2008) Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Crit Care Med 36(8):2238–2243
Berney S, Haines K, Skinner E, Denehy L (2012) Safety and feasibility of an exercise prescription approach to rehabilitation across the continuum of care for survivors of critical illness. Phys Ther 92(12):1524–1535
Knott A, Stevenson M, Harlow S (2015) Benchmarking rehabilitation practice in the intensive care unit. J Intensive Care Soc 16(1):24–30
Dammeyer J, Baldwin N, Packard D, Harrington S, Christofferson B, Christopher J, Strachan C, Iwashyna J (2013) Mobilizing outcomes: implementation of a nurse-led multidisciplinary mobility program. Crit Care Nurs Quart 36(1):109–119
Appleton R, MacKinnon M, Booth M, Wells J, Quasim T (2011) Rehabilitation within Scottish intensive care units: a national survey. J Intensive Care Soc 12(3):221–227
Winkelman C, Peereboom K (2010) Staff-perceived barriers and facilitators. Crit Care Nurse 30(2):S13–S16
Mendez-Tellez P, Dinglas V, Colantuoni E, Ciesla N, Sevransky J, Shanholtz C, Pronovost P, Needham D (2013) Factors associated with timing of initiation of physical therapy in patients with acute lung injury. J Crit Care 28(6):980–984
McWilliams D, Pantelides K (2008) Does physiotherapy led early mobilisation affect length of stay in ICU? Assoc Chart Physiother Respir Care J 40:5–10
Dinglas V, Colantuoni E, Ciesla N, Mendez-Tellez P, Shanholtz C, Needham D (2013) Occupational therapy for patients with acute lung injury: factors associated with time to first intervention in the intensive care unit. Am J Occup Ther 67(3):355–362
Harris C, Shahid S (2014) Physical therapy-driven quality improvement to promote early mobility in the intensive care unit. Bayl Univ Med Cent Proc 27(3):203–207
Zanni J, Korupolu R, Fan E, Pradhan P, Janjua K, Palmer J, Brower R, Needham D (2010) Rehabilitation therapy and outcomes in acute respiratory failure: an observational pilot project. J Crit Care 25(2):254–262
Engel H, Tatebe S, Alonzo P, Mustille R, Rivera M (2013) Physical therapist-established intensive care unit early mobilization program: quality improvement project for critical care at the University of California San Francisco Medical Center. Phys Ther 93:975–985
Bassett R, McCutcheon Adams K, Danesh V, Groat P, Haugen A, Kiewel A, Small C, Van-Leuven M, Venus S, Ely E (2015) Rethinking critical care: decreasing sedation, increasing delirium monitoring, and increasing patient mobility. Jt Comm J Qual Patient Saf 41(2):62–74
Jolley S, Caldwell E, Hough C (2014) Factors associated with receipt of physical therapy consultation in patients requiring prolonged mechanical ventilation. Dimens Criti Care Nurs 33(3):160–167
Jolley S, Dale C, Hough C (2015) Hospital-level factors associated with report of physical activity in patients on mechanical ventilation across Washington State. Ann Am Thorac Soc 12(2):209–215
Jolley S, Regan-Baggs J, Dickson R, Hough C (2014) Medical intensive care unit clinician attitudes and perceived barriers towards early mobilization of critically ill patients: a cross-sectional survey study. BMC Anaesthesiol 14:84
Tadyanemhandu C, Manie S (2015) Profile of patients and physiotherapy patterns in intensive care units in public hospitals in Zimbabwe: a descriptive cross-sectional study. BMC Anaesthesiol 15:136
Davis J, Crawford K, Wierman H, Osgood W, Cavanaugh J, Smith K, Mette S, Orff S (2013) Mobilization of ventilated older adults. J Geriatr Phys Ther 36(4):162–168
Malone D, Ridgeway K, Nordon-Craft A, Moss P, Schenkman M, Moss M (2015) Physical therapist practice in the intensive care unit: results of a national survey. Phys Ther 95(10):1335–1344
Barber E, Everard T, Holland A, Tipping C, Bradley S, Hodgson C (2015) Barriers and facilitators to early mobilisation in intensive care: a qualitative study. Aust Crit Care 28(4):177–182
Leditschke A, Green M, Irvine J, Bissett B, Mitchell I (2012) What are the barriers to mobilizing intensive care patients? Cardiopulm Phys Ther 23(1):26–29
Williams N, Flynn M (2013) An exploratory study of physiotherapist’s views of early rehabilitation in critically ill patients. Physiother Practi Res 34(2):93–102
Bakhru R, Wiebe D, McWilliams D, Spuhler V, Schweickert W (2015) An environmental scan for early mobilization practices in US ICUs. Crit Care Med 43(11):2360–2369
Eakin M, Ugbah L, Arnautovic T, Parker A, Needham D (2015) Implementing and sustaining an early rehabilitation program in a medical intensive care unit: a qualitative analysis. J Crit Care 30(4):698–704
Hopkins R, Spuhler V, Thomsen G (2007) Transforming ICU culture to facilitate early mobility. Crit Care Clin 23(1):81–96
Miller M, Govindan S, Watson S, Hyzy R, Iwashyna T (2015) ABCDE, but in that order? A cross-sectional survey of Michigan intensive care unit sedation, delirium, and early mobility practices. Ann Am Thorac Soc 12(7):1066–1071
Hopkins R, Spuhler V (2009) Strategies for promoting early activity in critically ill mechanically ventilated patients. AACN Adv Crit Care 20(3):277–289
Bailey P, Thomsen G, Spuhler V, Blair R, Jewkes J, Bezdijian L, Veale K, Rodriguez L, Hopkins R (2007) Early activity is feasible and safe in respiratory failure patients. Crit Care Med 35(1):139–145
Brummel N, Girard T, Ely E, Pandharipande P, Morandi A, Hughes C, Graves A, Shintani A, Murphy E, Work B, Pun B, Boehm Gill L, Dittus R, Jackson J (2014) Feasibility and safety of early combined cognitive and physical therapy for critically ill medical and surgical patients: the activity and cognitive therapy in ICU (ACT-ICU) trial. Intensive Care Med 40(3):370–379
Garzon-Serrano J, Ryan C, Waak K, Hirschberg R, Tully S, Bittner E, Chipman D, Schmidt U, Kasotakis G, Benjamin J, Zafonte R, Eikermann M (2011) Early mobilization in critically ill patients: patient’s mobilization level depends on health care provider’s profession. Phys Med Rehabil 3(4):307–313
Holdsworth C, Haines K, Francis J, Marshall A, O’Connor D, Skinner E (2015) Mobilization of ventilated patients in the intensive care unit: an elicitation study using the theory of planned behavior. J Crit Care 30(6):1243–1250
King J, Crowe J (1998) Mobilization practices in Canadian critical care units. Physiotherapy 50(3):206–211
Perme C, Lettvin C, Throckmorton T, Mitchell K, Masud F (2011) Early mobility and walking for patients with femoral arterial catheters in intensive care unit: a case series. J Acute Care Phys Ther 2(1):30–34
Perme C, Nalty T, Winkelman C, Nawa R, Masud F (2013) Safety and efficacy of mobility interventions in patients with femoral catheters in the ICU: a prospective observational study. Cardiopulm Phys Ther 24(2):12–17
Dalmuji A, Zanni J, Mantheiy E, Colantuoni E, Kho M, Needham D (2013) Safety and feasibility of femoral catheters during physical rehabilitation in the intensive care unit. J Crit Care 28(4):535.e9–535.e15
Wang Y, Haines T, Ritchie P, Walker C, Ansell T, Ryan D, Lim P, Vij S, Acs R, Fealy N, Skinner E (2014) Early mobilization on continuous renal replacement therapy is safe and may improve filter life. Crit Care 18(4):R161
Toonstra A, Zanni J, Sperati J, Nelliot A, Mantheiy E, Skinner E, Needham D (2016) Feasibility and safety of physical therapy during continuous renal replacement therapy in the intensive care unit. Ann Am Thorac Soc 13(5):699–704
Bassett R, Vollman K, Brandwene L, Murray T (2012) Integrating a multidisciplinary mobility programme into intensive care practice (IMMPTP): a multicentre collaborative. Intensive Crit Care Nurs 28(2):88–97
Carrothers K, Barr J, Spurlock B, Ridgely M, Damberg C, Ely E (2013) Contextual issues influencing implementation and outcomes associated with an integrated approach to managing pain, agitation, and delirium in adult ICUs. Crit Care Med 41(9 Suppl 1):S128–S135
Reames C, Price D, King E, Dickinson S (2016) Mobilizing patients along the continuum of critical care. Dimens Crit Care Nurs 35(1):10–15
Balas M, Burke W, Gannon D, Cohen M, Colburn L, Bevil C, Franz D, Olsen K, Ely E, Vasilevskis E (2013) Implementing the awakening and breathing coordination, delirium monitoring/management, and early exercise/mobility bundle into everyday care: opportunities, challenges, and lessons learned for implementing the ICU pain, agitation, and delirium guidelines. Crit Care Med 41(9 Suppl 1):S116–S127
Messer A, Corner L, Forst S (2015) Implementation of a progressive mobilization program in a medical-surgical intensive care unit. Crit Care Nurse 35(5):28–42
Walker W, Wright J, Danjoux G, Howell S, Martin D, Bonner S (2015) Project post intensive care exercise (PIX): a qualitative exploration of intensive care unit survivors’ perceptions of quality of life post-discharge and experience of exercise rehabilitation. J Intensive Care Soc 16(1):37–44
Deacon K (2012) Re-building life after ICU: a qualitative study of the patient’s perspective. Intensive Crit Care Nurs 28(2):114–122
Czerwonka A, Herridge M, Chan L, Chu L, Matte A, Cameron J (2015) Changing support needs of survivors of complex critical illness and their family caregivers across the care continuum: a qualitative pilot study of towards RECOVER. J Crit Care 30(2):242–249
Connolly B, Thompson A, Douiri A, Moxham J, Hart N (2015) Exercise-based rehabilitation after hospital discharge for survivors of critical illness with intensive care unit–acquired weakness: a pilot feasibility trial. J Crit Care 30(3):589–598
Sottile P, Nordon-Craft A, Malone D, Schenkman M, Moss M (2015) Patient and family perceptions of physical therapy in the medical intensive care unit. J Crit Care 30(5):891–895
Needham D, Korupolu R, Zanni J, Pradhan P, Colantuoni E, Palmer J, Brower R, Fan E (2010) Early physical medicine and rehabilitation for patients with acute respiratory failure: a quality improvement project. Arch Phys Med Rehabil 91(4):536–542
Connolly B, Douiri A, Steier J, Moxham J, Denehy L, Hart N (2014) A UK survey of rehabilitation following critical illness: implementation of NICE clinical guidance 83 (CG83) following hospital discharge. BMJ Open 4:e004963
Hodgin K, Nordon-Craft A, McFann K, Mealer M, Moss M (2009) Physical therapy utilization in intensive care units: results from a national survey. Crit Care Med 37(2):561–568
Schweickert WD, Pohlman MC, Pohlman AS, Nigos C, Pawlik AJ, Esbrook CL, Spears L, Miller M, Franczyk M, Deprizio D, Schmidt GA, Bowman A, Barr R, McCallister KE, Hall JB, Kress JP (2009) Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet 373(9678):1874–1882
Dafoe S, Stiller K, Chapman M (2015) Staff perceptions of the barriers to mobilizing ICU patients. Internet J Allied Health Sci Pract 13(2):1–13
Dafoe S, Chapman M, Edwards S, Stiller K (2016) Overcoming barriers to the mobilisation of patients in an intensive care unit. Anaesth Intensive Care 44(2):185–324
Dinglas V, Parker A, Reddy D, Colantuoni E, Zanni J, Turnbull A, Nelliot A, Ciesla N, Needham D (2014) A quality improvement project sustainably decreased time to onset of active physical therapy intervention in patients with acute lung injury. Ann Am Thorac Soc 11(8):1230–1238
Fraser D, Spiva L, Forman W, Hallen C (2015) Original research: implementation of an early mobility program in an ICU. Am J Nurs 115(12):49–58
Wahab R, Yip N, Chandra S, Nguyen M, Pavlovich K, Benson T, Vilotijevic D, Rodier D, Patel K, Rychcik P, Perez-Mir E, Boyle S, Berlin D, Needham D, Brodie D (2016) The implementation of an early rehabilitation program is associated with reduced length of stay: a multi-ICU study. J Intensive Care Soc 17(1):2–11
Hanekom S, Louw Q, Coetzee A (2013) Implementation of a protocol facilitates evidence-based physiotherapy practice in intensive care units. Physiotherapy 99(2):139–145
Lee C, Herridge M, Matte A, Cameron J (2009) Education and support needs during recovery in acute respiratory distress syndrome survivors. Crit Care 13:R153
Michie S, van Stralen M, West R (2011) The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 23(6):42
Tabak M, Vollenbroek-Hutten M, van der Valk P, van der Pale J, Hermens H (2014) A telerehabilitation intervention for patients with chronic obstructive pulmonary disease: a randomized controlled pilot trial. Clin Rehabil 28(6):582–591
Authors contribution statement
All authors contributed to the acquisition, analysis and interpretation of data and were involved in the critical revision of the manuscript for important intellectual content. SP and CG contributed to study concept and design. SP, CG, PM, ZP, CB and BC drafted the manuscript. SP is funded by a National Health and Medical Research Council (NHMRC) Early Career Fellowship and was a recipient of a short-term European Respiratory Society (ERS) travelling fellowship. CG is partially funded by a NHMRC Translating Research into Practice Fellowship co-funded by Cancer Australia. BC is funded by a National Institute of Health Research (NIHR) Postdoctoral Fellowship. BC and NH are supported by the NIHR Biomedical Research Centre based at Guy’s and St. Thomas’ NHS Foundation Trust and King’s College London. The views expressed are those of BC and NH and are not necessarily those of the NHS, the NIHR or the Department of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no other formal conflicts of interest to declare.
Additional information
Take-home message: This systematic review has identified the barriers and enablers for performance of physical activity by survivors of critical illness. Barriers and enablers are multidimensional and span diverse factors. The majority of these barriers are modifiable and can be targeted in future clinical practice.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Parry, S.M., Knight, L.D., Connolly, B. et al. Factors influencing physical activity and rehabilitation in survivors of critical illness: a systematic review of quantitative and qualitative studies. Intensive Care Med 43, 531–542 (2017). https://doi.org/10.1007/s00134-017-4685-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-017-4685-4