Abstract
Objectives
During the acute treatment of diabetic ketoacidosis we (a) determined the temporal incidence of hyperchloraemia, and (b) quantified the influence of hyperchloraemia on interpretation of common blood gas derived acid base parameters, namely base deficit and bicarbonate.
Designand setting
Retrospective chart review in two regional paediatric intensive care units.
Measurements and Results
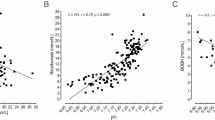
Stewart's physicochemical theory was used to develop regression equations quantifying the acidifying effect of hyperchloraemia on both base deficit and bicarbonate. These were then applied retrospectively to blood chemistry results from 18 children (median age 12.7 years, weight 43 kg) with diabetic ketoacidosis. Plasma ketonaemia was estimated using the albumin-corrected anion gap. The incidence of hyperchloraemia, as documented by a ratio of plasma chloride to sodium of greater than 0.79, increased from 6% at admission to 94% after 20 h of treatment. Correction for chloride produced a dramatic improvement in the relationship between changes in the anion gap vs. both base deficit (from R 2 = 0.55 to R 2 = 0.95) and bicarbonate (from R 2 = 0.51 to R 2 = 0.96) during treatment. After 20 h of treatment the mean base deficit had decreased from 24.7 mmol/l to 10.0 mmol/l however, the proportion that was due to hyperchloraemia increased from 2% to 98%.
Conclusions
It is now possible using a simple correction factor to quantify the confounding effect of hyperchloraemia on both base deficit and bicarbonate in diabetic ketoacidosis. This bedside tool may be a useful adjunct to guide therapeutic interventions.




Similar content being viewed by others
References
Dunger DB, Sperling MA, Acerini CL, Bohn DJ et al. (2004) ESPE/LWPES consensus statement on diabetic ketoacidosis in children and adolescents. Arch Dis Child 89:188–194
Emmett M, Narins RG (1977) Clinical use of the anion gap. Medicine (Baltimore) 56:38–54
Adrogue HJ, Wilson H, Boyd AE, III, Suki WN, Eknoyan G (1982) Plasma acid-base patterns in diabetic ketoacidosis. N Engl J Med 307:1603–1610
Oh MS, Banerji MA, Carroll HJ (1981) The mechanism of hyperchloraemic acidosis during the recovery phase of diabetic ketoacidosis. Diabetes 30:310–313
Halperin ML, Bear RA, Hannaford MC, Goldstein MB (1981) Selected aspects of the pathophysiology of metabolic acidosis in diabetes mellitus. Diabetes 30:781–787
Paulson WD (1986) Anion gap-bicarbonate relation in diabetic ketoacidosis. Am J Med 81:995–1000
Adrogue HJ, Eknoyan G, Suki WK (1984) Diabetic ketoacidosis: role of the kidney in the acid-base homeostasis re-evaluated. Kidney Int 25:591–598
O'Dell E, Tibby SM, Durward A, et al. (2005) Validation of a method to partition the base deficit in meningococcal sepsis: a retrospective study. Crit Care 9:R464–470
Hammeke M, Bear R, Lee R, Goldstein M, Halperin M (1978) Hyperchloraemic metabolic acidosis in diabetes mellitus: a case report and discussion of pathophysiologic mechanisms. Diabetes 27:16–20
Oh MS, Carroll HJ, Goldstein DA, Fein IA (1978) Hyperchloraemic acidosis during the recovery phase of diabetic ketosis. Ann.Intern.Med 89:925–927
Stewart PA (1983) Modern quantitative acid-base chemistry. Can J Physiol Pharmacol 61:1444–1461
Gilfix BM, Bique M, Magder S (1993) A physical chemical approach to the analysis of acid-base balance in the clinical setting. J Crit Care 8:187–197
Figge J, Jabor A, Kazda A, Fencl V (1998) Anion gap and hypoalbuminemia. Crit Care Med 26:1807–1810
Durward A, Skellet S, Mayer A, Taylor D, et al. (2001) The value of the Cl:Na ratio in differentiating the aetiology of metabolic acidosis. Intensive Care Med 27:828–835
Wilkes P (1998) Hypoproteinaemia, strong ion difference and acid-base status in critically ill patients. J Appl Physiol 84:1740–1748
Hood VL, Tannen RL (1998) Protection of acid-base balance by pH regulation of acid production. N Engl J Med 339:819–826
Astrup P (1956) A simple electrometric technique for the determination of carbon dioxide tension in blood and plasma, total content of carbon dioxide in plasma and bicarbonate content in ‘separated’ plasma at a fixed carbon dioxide tension. Scand Clin Lab Invest 8:33
Wagner A, Risse A, Brill HL, et al. (1999) Therapy of severe diabetic ketoacidosis. Zero-mortality under very-low-dose insulin application. Diabetes Care 22:674–677
Mahoney CP, Vlcek BW, DelAguila M (1999) Risk factors for developing brain herniation during diabetic ketoacidosis. Pediatr Neurol 21:721–727
Roberts MD, Slover RH, Chase HP (2001) Diabetic ketoacidosis with intracerebral complications. Paediatric Diabetes 2:109–114
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Law of mass action
When a weak acid dissociates incompletely in an aqueous solution, the relationship between the dissociated and undissociated components is constant. The Henderson equation is a well-known modification of this law, namely k = [H+] [HCO3 −]/[H2CO3], where k is defined as the hydrogen ion concentration at which half of the carbonic acid is dissociated. The Stewart approach also applies the law of mass action to carbonic acid but includes other major weak acids found in human plasma (albumin, phosphate), as well as incorporating the dissociation equilibrium for water: K w = [H+] [OH−]/[H2O].
Mass conservation
In an aqueous solution the amount of each component substance remains constant unless (a) a substance is added or removed or (b) the substance is generated or destroyed.
Preservation of electroneutrality
In an aqueous solution, the sum of all positively charged ion concentrations always equals the sum of all negatively charged ion concentrations.
AcidBasics II software uses the Stewart equations to calculate pH from its three independent variables, namely pCO2, strong ion difference ([Na+] + [K+] + [Mg2+] + [Ca2+] − [Cl−] − [lactate−]) and total weak acid (phosphate and albumin charge) at a temperature of 37°C. If pH is known and all variables other than sodium and chloride are kept constant the magnitude of pH change as chloride is varied relative to sodium can be calculated. Since bicarbonate is dependent on pH, its theoretical charge (mEq/L) can be accurately calculated using across varying degrees of hypo/hyperchloraemia (chloride 70–130 mmol/L) by keeping all other variables in Stewart's equation constant. A linear regression equation can be plotted between (Na-Cl) and calculated bicarbonate to explain the degree to which bicarbonate is directly influenced by hyperchloraemia. For example sodium of 140 mEq/L and chloride 120 mEq/L (difference 20 mEq/L) will result in a bicarbonate concentration of 0.93 × 20 mEq/L − 5.9 = 12.7 mEq/L using this regression equation. A similar approach can be used to calculate the influence of hyperchloraemia on the base deficit. For example a difference of 20 mEq/L between Na and Cl results in a base deficit of −1.2 × 20 mEq/L + 42.5 = −18.5 mEq/L. Stewart's methodology is necessary since the traditional Henderson-Hasselbalch model assumes bicarbonate is an independent variable and is not influenced by chloride, hence it offers no method for the quantification of hyperchloraemic acidosis.
Rights and permissions
About this article
Cite this article
Taylor, D., Durward, A., Tibby, S.M. et al. The influence of hyperchloraemia on acid base interpretation in diabetic ketoacidosis. Intensive Care Med 32, 295–301 (2006). https://doi.org/10.1007/s00134-005-0009-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-005-0009-1