Abstract
Background
While the relationship between combat exposure and alcohol problems is well-established, the role of perceptions of trauma is less understood. The goal of this study was to explore associations between National Guard (NG) and reserve soldiers’ perceptions of combat experiences as traumatic and alcohol problems, and to examine marital satisfaction as a possible protective factor.
Methods
The Operation: SAFETY study recruited US Army Reserve and NG soldiers and their partners to complete a questionnaire covering many physical and mental health, military service, and substance use topics. Negative binomial regression models examined the impact of perceived trauma of combat experiences on alcohol problems (N = 198). The potential role of marital satisfaction as a resiliency factor was also examined.
Results
The perception of combat experiences as traumatic was associated with increased risk of alcohol problems (risk ratio [RR] = 1.06, 95% confidence interval [CI] 1.01, 1.12; p = 0.024). Combat exposure itself showed no relationship. Marital satisfaction had a significant interaction with perceived combat trauma on alcohol problems (RR = 0.90, 95% CI 0.81, 0.99, p = 0.046), such that soldiers who perceived combat exposure as moderately-highly traumatic were less likely to have alcohol problems when they rated their marital satisfaction highly.
Conclusions
Our results demonstrate that the perception of combat experiences as traumatic may be a greater contributor to adverse outcomes, such as alcohol problems, than mere combat exposure. They also demonstrate the importance of marital satisfaction as a resiliency factor, particularly at the highest levels of trauma.

Similar content being viewed by others
References
Green KT, Beckham JC, Youssef N, Elbogen EB (2014) Alcohol misuse and psychological resilience among US Iraq and Afghanistan era veterans. Addict Behav 39(2):406–413. https://doi.org/10.1016/j.addbeh.2013.08.024
Hoge CW, Auchterlonie JL, Milliken CS (2006) Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA 295(9):1023–1032. https://doi.org/10.1001/jama.295.9.1023
Bray RM, Hourani LL (2007) Substance use trends among active duty military personnel: findings from the United States Department of Defense Health Related Behavior Surveys, 1980–2005. Addiction 102(7):1092–1101. https://doi.org/10.1111/j.1360-0443.2007.01841.x
Milliken CS, Auchterlonie JL, Hoge CW (2007) Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq war. J Am Med Assoc 298(18):2141–2148. https://doi.org/10.1001/jama.298.18.2141
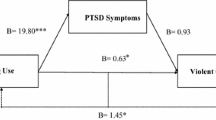
Wright KM, Foran HM, Wood MD, Eckford RD, McGurk D (2012) Alcohol problems, aggression, and other externalizing behaviors after return from deployment: understanding the role of combat exposure, internalizing symptoms, and social environment. J Clin Psychol 68(7):782–800. https://doi.org/10.1002/jclp.21864
Jacobson IG, Ryan MA, Hooper TI, Smith TC, Amoroso PJ, Boyko EJ, Gackstetter GD, Wells TS, Bell NS (2008) Alcohol use and alcohol-related problems before and after military combat deployment. J Am Med Assoc 300(6):663–675. https://doi.org/10.1001/jama.300.6.663
Seal KH, Cohen G, Waldrop A, Cohen BE, Maguen S, Ren L (2011) Substance use disorders in Iraq and Afghanistan veterans in VA healthcare, 2001–2010: Implications for screening, diagnosis and treatment. Drug Alcohol Depend 116(1–3):93–101
Homish GG, Homish DL, Cummings KJ, Heavey SC (2015) Military Deployments, Combat Exposure and Partner Drinking Paper presented at the Research Society on Alcoholism San Antonio, Texas, June 2015
Bray RM, Brown JM, Williams J (2013) Trends in binge and heavy drinking, alcohol-related problems, and combat exposure in the US military. Subst Use Misuse 48(10):799–810. https://doi.org/10.3109/10826084.2013.796990
Wilk JE, Bliese PD, Kim PY, Thomas JL, McGurk D, Hoge CW (2010) Relationship of combat experiences to alcohol misuse among US soldiers returning from the Iraq war. Drug Alcohol Depend 108(1–2):115–121. https://doi.org/10.1016/j.drugalcdep.2009.12.003
Eisen SV, Schultz MR, Vogt D, Glickman ME, Elwy AR, Drainoni ML, Osei-Bonsu PE, Martin J (2012) Mental and physical health status and alcohol and drug use following return from deployment to Iraq or Afghanistan. Am J Public Health 102 Suppl 1:S66–S73. https://doi.org/10.2105/AJPH.2011.300609
Brown GW, Bifulco A, Harris TO (1987) Life events, vulnerability and onset of depression: some refinements. Br J Psychiatry 150:30–42
Ozer EJ, Best SR, Lipsey TL, Weiss DS (2003) Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychol Bull 129(1):52–73
Carlier IVE, Lamberts RD, Gersons BPR (2000) The dimensionality of trauma: a multidimensional scaling comparison of police officers with and without posttraumatic stress disorder. Psychiatry Res 97(1):29–39. https://doi.org/10.1016/S0165-1781(00)00211-0
Renshaw KD (2011) An integrated model of risk and protective factors for post-deployment PTSD symptoms in OEF/OIF era combat veterans. J Affect Disord 128(3):321–326. https://doi.org/10.1016/j.jad.2010.07.022
Iversen AC, Fear NT, Ehlers A, Hughes JH, Hull L, Earnshaw M, Greenberg N, Rona R, Wessely S, Hotopf M (2008) Risk factors for post-traumatic stress disorder among UK Armed Forces personnel. Psychol Med 38(04):511–522
Leonard KE, Eiden RD (2007) Marital and family processes in the context of alcohol use and alcohol disorders. Annu Rev Clin Psychol 3:285–310. https://doi.org/10.1146/annurev.clinpsy.3.022806.091424
Ferrier-Auerbach AG, Kehle SM, Erbes CR, Arbisi PA, Thuras P, Polusny MA (2009) Predictors of alcohol use prior to deployment in National Guard Soldiers. Addict Behav 34(8):625–631. https://doi.org/10.1016/j.addbeh.2009.03.027
Leonard KE, Homish GG (2008) Predictors of heavy drinking and drinking problems over the first 4 years of marriage. Psychol Addict Behav 22(1):25–35. https://doi.org/10.1037/0893-164X.22.1.25
Epstein EE, McCrady BS (1998) Behavioral couples treatment of alcohol and drug use disorders: current status and innovations. Clin Psychol Rev 18(6):689–711
McCrady BS, Wilson AD, Munoz RE, Fink BC, Fokas K, Borders A (2016) Alcohol-focused behavioral couple therapy. Fam Process 55(3):443–459. https://doi.org/10.1111/famp.12231
McCrady BS, Epstein EE, Cook S, Jensen N, Hildebrandt T (2009) A randomized trial of individual and couple behavioral alcohol treatment for women. J Consult Clin Psychol 77(2):243–256. https://doi.org/10.1037/a0014686
Heinz AJ, Wu J, Witkiewitz K, Epstein DH, Preston KL (2009) Marriage and relationship closeness as predictors of cocaine and heroin use. Addict Behav 34(3):258–263. https://doi.org/10.1016/j.addbeh.2008.10.020
Vest BM, Cercone Heavey S, Homish DL, Homish GG (2017) Marital satisfaction, family support, and pre-deployment resiliency factors related to mental health outcomes for reserve and national guard soldiers. Mil Behav Health 5(4): 313–323. https://doi.org/10.1080/21635781.2017.1343694
Tracie Shea M, Reddy MK, Tyrka AR, Sevin E (2013) Risk factors for post-deployment posttraumatic stress disorder in national guard/reserve service members. Psychiatry Res 210(3):1042–1048. https://doi.org/10.1016/j.psychres.2013.08.039
Tsai J, Harpaz-Rotem I, Pietrzak RH, Southwick SM (2012) The role of coping, resilience, and social support in mediating the relation between ptsd and social functioning in veterans returning from Iraq and Afghanistan. Psychiatry-Interpers Biol Process 75(2):135–149
Castaneda LW, Harrell MC, Varda DM, Curry Hall K, Beckett MK, Stern S (2008) Deployment experiences of guard and reserve families: implications for support and retention. RAND Corporation, Santa Monica, CA.
Devonish JA, Homish DL, Vest BM, Daws RC, Hoopsick RA, Homish GG (2017) The impact of military service and traumatic brain injury on the substance use norms of Army Reserve and National Guard Soldiers and their spouses. Addict Behav 72:51–56. https://doi.org/10.1016/j.addbeh.2017.03.012
Heavey SC, Homish DL, Goodell EA, Homish GG (2017) US reserve soldiers’ combat exposure and intimate partner violence: not more common but it is more violent. Stress Health: J Int Soc Investig Stress. 33(5): 617–623. https://doi.org/10.1002/smi.2748
Babor TF, Del Boca FK (1992) Just the facts: enhancing measurement of alcohol consumption using self-report methods. In: Litten RZ, Allen JP (eds) Measuring alcohol consumption: psychosocial and biochemical methods. Humana Press, Totowa, pp 3–20
Locke HJ, Wallace KM (1959) Short marital-adjustment and prediction tests: their reliability and validity. Marriage Fam Living 21(3):251–255
Vogt D, Smith BN, King DW, King LA (2012) Manual for the deployment risk and resilience inventory-2 (DRRI-2): a collection of measures for studying deployment-related experiences of military veterans. National Center for PTSD, Boston, MA
Vrana S, Lauterbach D (1994) Prevalence of traumatic events and post-traumatic psychological symptoms in a nonclinical sample of college students. J Trauma Stress 7(2):289–302. https://doi.org/10.1002/jts.2490070209
Homish GG, Leonard KE, Cornelius JR (2010) Individual, partner, and relationship factors associated with the nonmedical use of prescription drugs. Addiction 105(8):1457–1465
Goldmann E, Calabrese JR, Prescott MR, Tamburrino M, Liberzon I, Slembarski R, Shirley E, Fine T, Goto T, Wilson K, Ganocy S, Chan P, Serrano MB, Sizemore J, Galea S (2012) Potentially modifiable pre-, peri-, and postdeployment characteristics associated with deployment-related posttraumatic stress disorder among ohio army national guard soldiers. Ann Epidemiol 22(2):71–78. https://doi.org/10.1016/j.annepidem.2011.11.003
Polusny MA, Erbes CR, Murdoch M, Arbisi PA, Thuras P, Rath MB (2011) Prospective risk factors for new-onset post-traumatic stress disorder in National Guard soldiers deployed to Iraq. Psychol Med 41(4):687–698. https://doi.org/10.1017/S0033291710002047
Fischer EP, Sherman MD, McSweeney JC, Pyne JM, Owen RR, Dixon LB (2015) Perspectives of family and veterans on family programs to support reintegration of returning veterans with posttraumatic stress disorder. Psychological services 12(3):187–198. https://doi.org/10.1037/ser0000033
Collinge W, Kahn J, Soltysik R (2012) Promoting reintegration of National Guard veterans and their partners using a self-directed program of integrative therapies: a pilot study. Mil Med 177(12):1477–1485
Lewis M, Lamson A, White M (2016) The state of dyadic methodology: an analysis of the literature on interventions for military couples. J Couple Relatsh Ther 15(2):135–157. https://doi.org/10.1080/15332691.2015.1106998
Monk JK, Ogolsky BG, Bruner V (2016) Veteran couples integrative intensive retreat model: an intervention for military veterans and their relational partners. J Couple Relatsh Ther 15(2):158–176
Acknowledgements
Research reported in this publication was supported by the National Institute on Drug Abuse of the National Institutes of Health under award number R01DA034072 (GGH). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Portions of this work were presented at a symposium at the 39th Annual Meeting of the Research Society on Alcoholism, New Orleans, Louisiana, June 2016.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical standards
The State University of New York at Buffalo’s Institutional Review Board as well as the Army Human Research Protections Office, Office of the Chief, Army Reserve as well as the Adjutant General of the National Guard approved the study protocol. All participants provided informed consent.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Vest, B.M., Homish, D.L., Hoopsick, R.A. et al. What drives the relationship between combat and alcohol problems in soldiers? The roles of perception and marriage. Soc Psychiatry Psychiatr Epidemiol 53, 413–420 (2018). https://doi.org/10.1007/s00127-017-1477-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-017-1477-7