Abstract
Since the 1970s, C-peptide has been used as a surrogate marker for monitoring the progression of type 1 and type 2 diabetes and to determine the effects of interventions designed to preserve or improve residual beta cell function. C-peptide measurement is a well-established surrogate of residual beta cell activity and of clinical significance as it is associated with HbA1c, risk for microvascular complications and the incidence of hyperglycaemia in longitudinal studies. Measurement of C-peptide after a mixed meal tolerance test is considered the gold standard of measuring beta cell function in type 1 diabetes, but the method is laborious and inconvenient. In this issue of Diabetologia, Wentworth et al (https://doi.org/10.1007/s00125-018-4722-z) report an algorithm for estimating C-peptide (CPEST) based on six routine clinical measures. These do not include stimulated C-peptide measurement and outperform other prevailing algorithms for estimating residual beta cell function. Going forward it is very likely that this new algorithm will serve as a simple measure of beta cell function in routine practice and as a more acceptable primary outcome measure in future trials of disease-modifying therapies.
Similar content being viewed by others
Introduction
In the pancreatic beta cell, INS mRNA is translated as pre-proinsulin, and removal of its signal peptide produces proinsulin. Proinsulin consists of an amino-terminal B chain, a carboxy-terminal A chain and a connecting peptide in the middle known as the C-peptide. Proinsulin is enzymatically cleaved into C-peptide and the mature form of insulin, which are secreted in equimolar concentrations when the beta cell is appropriately stimulated. Insulin has a shorter half-life (3–5 min) than C-peptide, which is degraded more slowly (half-life of 20–30 min). Insulin is essentially cleared by the liver, while C-peptide is eliminated by the kidney [1]. Thus, measurement of C-peptide in peripheral blood is an established way of evaluating insulin secretion.
C-peptide is also a useful tool in the classification of diabetes. It can help differentiate type 1 diabetes, type 2 diabetes, latent autoimmune diabetes in the adult (LADA) and MODY. However, current guidelines provide a pragmatic clinical approach to classification of diabetes. Guidelines from the ADA (in conjunction with the American Association for Clinical Chemistry and the National Academy of Clinical Biochemistry) [2] and from the American Association of Clinical Endocrinologists (AACE) [3] restrict the use of C-peptide in the diagnosis of diabetes to uncommon or unclear cases of type 1 or type 2 diabetes, or when there is doubt over the diagnosis of type 1 or type 2 diabetes. Thus, C-peptide is still felt to be more important in research than in daily clinical practice. It does, however, provide an excellent marker of residual beta cell activity and even random or fasting levels may be of clinical significance as they have been associated in longitudinal studies with HbA1c, risk for microvascular complications and the incidence of hyperglycaemia [4,5,6,7]. Moreover, C-peptide is often evaluated as the primary outcome in type 1 diabetes intervention trials [8].
Measuring C-peptide
C-peptide levels can be measured in different states (random, fasting or stimulated), by several methods and in different fluids (venous blood or urine) (Table 1). The urine tests include a spot test, a 24 h urinary collection or urinary C-peptide creatinine ratio [9, 10]. Despite these tests being non-invasive, they have the drawbacks of being inaccurate in people with decreased kidney function, being sex-dependent (creatinine clearance) and/or requiring good compliance (24 h sampling). Serum measurement also poses a challenge because C-peptide is susceptible to proteolytic cleavage and therefore special precautions are recommended when sampling for C-peptide analysis [11]. The lack of C-peptide measurement standardisation is another issue [12]. Therefore, measurement of C-peptide in larger trials where C-peptide is used as an outcome variable is often centralised.
Random C-peptide is measured at any time of the day without taking food intake into consideration, whereas fasting C-peptide is measured after an 8–10 h fast. C-peptide can also be evaluated postprandially, often 90 min after a standard meal [13, 14]. Stimulated C-peptide can be measured after specific stimulation with glucagon, mixed meal, oral or intravenous glucose, two-phase glucose clamp, tolbutamide, sulfonylurea or amino acids [8, 11, 12, 15,16,17,18]. In general, serum C-peptide testing after stimulation is superior to random C-peptide, fasting C-peptide and urine testing [13], though random C-peptide has been shown to differentiate individuals with type 1 vs type 2 diabetes [19]. The mixed meal tolerance test (MMTT) and the glucagon stimulation test (GST) provide good estimates of beta cell function and are the most widely used. In the MMTT a liquid meal is ingested in the fasting state and C-peptide is measured over 2–4 h. In the glucagon stimulation test, glucagon is injected intravenously, and C-peptide is measured over the next 10 min. Based on a workshop held in 2001, the ADA concluded that MMTT and GST were the tests recommended for stimulated C-peptide testing [11].
More recently, two parallel trials conducted by the European C-peptide Trial Study Group and Type 1 Diabetes TrialNet Research Group were conducted to evaluate the properties and tolerability of these tests [20]. Both studies showed that MMTT is a more sensitive test of residual beta cell function, with the peak C-peptide being significantly greater than in the GST. In people with recent onset type 1 diabetes, the MMTT C-peptide values steadily increased over the first hour and then more slowly over the next hour, whereas the GST values reached a peak at 6 min and then declined [20]. The greater sensitivity of MMTT is likely to be due to an effect of incretins because the oral glucose stimulus increases the actions of glucose-dependent insulinotropic polypeptide and glucagon-like peptide 1 compared with a similar intravenous stimulus. Originally described in 1977 [21], the GST is still the most commonly used stimulation method [13]. Mild nausea is a common side effect of the GST, especially in younger individuals [20]. It may be that the observed side effects and lower peak values in the GST are due to the use of a fixed glucagon dose rather than a weight-based dose in most studies [20]. Because of the higher peak value, MMTT may be preferable in the research setting, whereas due to its short duration the GST may be the choice in the clinical setting [13, 20]. In the TrialNet study, most participants preferred the MMTT [20]. However, the GST was preferred by individuals more concerned with time and who experienced less nausea [20]. Based on these features, a recent review by Leighton et al recommended the GST in clinical practice [13].
Several studies have reported that individuals with type 1 diabetes who show some remaining beta cell activity are considerably less prone to developing microvascular complications than those who are C-peptide deficient [22]. In the Diabetes Control and Complications Trial (DCCT), improved glycaemic control, lower risks of microvascular complications and less hyperglycaemia were directly related to stimulated C-peptide response at baseline in the intensive therapy group [11, 23]. Others have found that age at diagnosis is the strongest predictor of detectable residual beta cell activity (C-peptide) after 3–6 years of type 1 diabetes [24, 25]. In a study of 919 individuals with type 1 diabetes, the overall frequency of detectable non-fasting C-peptide was 29%, decreasing with time from diagnosis regardless of age at diagnosis [26]. Of those with undetectable non-fasting C-peptide, 19% were C-peptide positive upon stimulation [26]. Also BMI Z score may affect basal and stimulated C-peptide levels, whereas sex has only been significantly associated with stimulated C-peptide [27].
Thus, several factors influence C-peptide levels, making modelling of residual beta cell activity challenging. Nevertheless, efforts have been made to come up with a simpler, still accurate, measure of beta cell function as a more practical and cost-effective approach. A simple evaluation of residual beta cell function that can be used in clinical practice and trials as well as in research will be of great value.
Modelling residual beta cell function
Back in 2009, Mortensen et al proposed an algorithm to estimate dynamic changes in residual beta cell function based on HbA1c and insulin dose [28]. They defined partial remission as an insulin-dose-adjusted HbA1c (IDAA1c) ≤9. IDAA1c was defined as: HbA1c (%) + [4 × insulin dose (U kg−1 [24 h]−1)]. This algorithm was validated in subsequent studies, and the IDAA1c has prevailed as a measurement for partial remission [29,30,31,32,33]. It has also been proposed that a total daily dose of insulin of ≤0.3 U kg−1 day−1 performed equally well as IDAA1c in predicting remission [34], though not thoroughly tested. In a study by Boyle et al, HbA1c, insulin used or the combination of both, using IDAA1c, were not reliable surrogates of beta cell function compared with C-peptide response to MMTT stimulation in individuals with type 1 diabetes [35]. Recently, a novel approach to monitoring longitudinal changes in fasting and postprandial C-peptide from dried blood spots collected in the home setting was reported [14]. This simple methodology, which allows frequent sampling, is an interesting supplement or alternative, to algorithms developed for estimation of residual beta cell function. It shows good correlation with plasma C-peptide, but more studies are needed to evaluate this innovative approach.
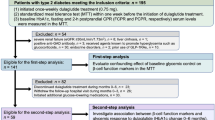
The study by Wentworth et al [36] in this issue of Diabetologia provides a novel algorithm for assessing beta cell function based on routine clinical variables. The model is developed on data from eight randomised intervention trials of individuals with recent-onset type 1 diabetes. The model is based on disease duration, BMI, insulin dose, HbA1c, fasting plasma C-peptide (FCP) and fasting plasma glucose (FPG). The algorithm for this estimated C-peptide (CPEST) is: loge (CPEST + 1) = 0.317 + 0.00956 × BMI − 0.000159 × duration + 0.710 × FCP − 0.0117 × FPG − 0.0186 × HbA1c − 0.0665 × insulin, where BMI is in kg/m2, duration in days, FCP in nmol/l, FPG in mmol/l, HbA1c in % and insulin in U/kg [36].
The authors tested several models and show that one model (M6) based on disease duration, BMI, insulin dose, HbA1c, fasting plasma C-peptide and fasting plasma glucose is accurate (area under the ROC curve: 0.89) and superior to previously used models, including IDAA1c. Like other models for estimating residual beta cell function, this model was developed based on data from young individuals (≤21 years of age), where more residual beta cell activity is expected [24, 25]. It is also shown that the model-based estimation of C-peptide requires only a limited increase in sample size (16–17%), compared with standard trial design, if used as a primary outcome measurement [36]. Another interesting feature is that the CPEST is suitable for assessing beta cell function during disease-modifying therapy. The study benefited from the fact that important measurements were centralised in the TrialNet and Immune Tolerance Network (ITN) studies so the generalisation of this may still be an issue. Further development of standardised C-peptide assays is important to adapt these new algorithms in clinical practice [12].
Interestingly, age does not add to the model (e.g. M6 vs M7) though several studies have shown that age is a very strong predictor of genetic risk, disease progression rate and beta cell function [14, 25, 37, 38]. C-peptide is significantly related to age-at-onset with a younger age of onset resulting in a more rapid decline in C-peptide [28, 39]. Also, age continues to affect C-peptide levels up to 4 years from diagnosis [35]. It has also been shown that sex is significantly associated only with stimulated C-peptide [27]. Inclusion of age and sex did not improve the model (M6 vs M8) [36]. Thus, apparently the other clinical measures accounted for the effect of age and sex on beta cell function. It is still to be tested how well the model works in the range of very low C-peptide levels that still respond to hyperglycaemia with increased C-peptide production [40] and if it performs equally well over the full spectrum of C-peptide values [27].
Conclusion
In summary, the identification of biomarkers that can predict the path of beta cell function in recent onset type 1 diabetes will be of major importance as it would inform which participants are likely to benefit most from intervention. Higher residual beta cell function early in the disease has strong long-term beneficial effects [11]. Type 1 diabetes is a heterogeneous disease and it is likely that a more tailored, stratified approach is required to improve and optimise treatment success.
The study by Wentworth et al [36] provides a simple, novel algorithm for beta cell function in clinical settings without the need of a stimulation test [36]. Importantly, it has also been demonstrated to work for individuals on different immune modulation regimens, thus, providing a convenient measurement of beta cell function in clinical intervention trials.
Abbreviations
- CPEST :
-
Estimated C-peptide
- GST:
-
Glucagon stimulation test
- IDAA1c :
-
Insulin-dose-adjusted HbA1c
- MMTT:
-
Mixed meal tolerance test
References
Jones AG, Hattersley AT (2013) The clinical utility of C-peptide measurement in the care of patients with diabetes. Diabet Med 30(7):803–817. https://doi.org/10.1111/dme.12159
Sacks DB, Arnold M, Bakris GL et al (2011) Position statement executive summary: guidelines and recommendations for laboratory analysis in the diagnosis and management of diabetes mellitus. Diabetes Care 34(6):1419–1423. https://doi.org/10.2337/dc11-9997
Handelsman Y, Bloomgarden ZT, Grunberger G et al (2015) American Association of Clinical Endocrinologists and American College of Endocrinology – clinical practice guidelines for developing a diabetes mellitus comprehensive care plan – 2015. Endocr Pract 21(Suppl 1):1–87. https://doi.org/10.4158/EP15672.GLSUPPL
Lachin JM, McGee P, Palmer JP, Group DER (2014) Impact of C-peptide preservation on metabolic and clinical outcomes in the Diabetes Control and Complications Trial. Diabetes 63(2):739–748. https://doi.org/10.2337/db13-0881
Madsbad S, Alberti KG, Binder C et al (1979) Role of residual insulin secretion in protecting against ketoacidosis in insulin-dependent diabetes. BMJ 2(6200):1257–1259. https://doi.org/10.1136/bmj.2.6200.1257
Steele C, Hagopian WA, Gitelman S et al (2004) Insulin secretion in type 1 diabetes. Diabetes 53(2):426–433. https://doi.org/10.2337/diabetes.53.2.426
Steffes MW, Sibley S, Jackson M, Thomas W (2003) Beta-cell function and the development of diabetes-related complications in the diabetes control and complications trial. Diabetes Care 26(3):832–836. https://doi.org/10.2337/diacare.26.3.832
Greenbaum CJ, Harrison LC, Immunology of Diabetes Society (2003) Guidelines for intervention trials in subjects with newly diagnosed type 1 diabetes. Diabetes 52(5):1059–1065. https://doi.org/10.2337/diabetes.52.5.1059
Bowman P, McDonald TJ, Shields BM, Knight BA, Hattersley AT (2012) Validation of a single-sample urinary C-peptide creatinine ratio as a reproducible alternative to serum C-peptide in patients with type 2 diabetes. Diabet Med 29(1):90–93. https://doi.org/10.1111/j.1464-5491.2011.03428.x
Gjessing HJ, Matzen LE, Faber OK, Froland A (1989) Fasting plasma C-peptide, glucagon stimulated plasma C-peptide, and urinary C-peptide in relation to clinical type of diabetes. Diabetologia 32(5):305–311. https://doi.org/10.1007/BF00265547
Palmer JP, Fleming GA, Greenbaum CJ et al (2004) C-peptide is the appropriate outcome measure for type 1 diabetes clinical trials to preserve beta-cell function: report of an ADA workshop, 21-22 October 2001. Diabetes 53(1):250–264. https://doi.org/10.2337/diabetes.53.1.250
Little RR, Wielgosz RI, Josephs R et al (2017) Implementing a reference measurement system for C-peptide: successes and lessons learned. Clin Chem 63(9):1447–1456. https://doi.org/10.1373/clinchem.2016.269274
Leighton E, Sainsbury CA, Jones GC (2017) A practical review of C-peptide testing in diabetes. Diabetes Ther 8(3):475–487. https://doi.org/10.1007/s13300-017-0265-4
Willemsen RH, Burling K, Barker P et al (2018) Frequent monitoring of C-peptide levels in newly diagnosed type 1 subjects using dried blood spots collected at home. J Clin Endocrinol Metab 103(9):3350–3358. https://doi.org/10.1210/jc.2018-00500
Ludvigsson J (1983) Methodological aspects on C-peptide measurements. Acta Medica Scand Suppl 671:53–59
Mirel RD, Ginsberg-Fellner F, Horwitz DL, Rayfield EJ (1980) C-peptide reserve in insulin-dependent diabetes. Comparative responses to glucose, glucagon and tolbutamide. Diabetologia 19(3):183–188. https://doi.org/10.1007/BF00275266
Greenbaum C, Seidel K, Pihoker C (2004) The case for intravenous arginine stimulation in lieu of mixed-meal tolerance tests as outcome measure for intervention studies in recent-onset type 1 diabetes. Diabetes Care 27(5):1202–1204. https://doi.org/10.2337/diacare.27.5.1202
Keymeulen B, Vandemeulebroucke E, Ziegler AG et al (2005) Insulin needs after CD3-antibody therapy in new-onset type 1 diabetes. N Engl J Med 352(25):2598–2608. https://doi.org/10.1056/NEJMoa043980
Berger B, Stenstrom G, Sundkvist G (2000) Random C-peptide in the classification of diabetes. Scand J Clin Lab Invest 60(8):687–693
Greenbaum CJ, Mandrup-Poulsen T, McGee PF et al (2008) Mixed-meal tolerance test versus glucagon stimulation test for the assessment of beta-cell function in therapeutic trials in type 1 diabetes. Diabetes Care 31(10):1966–1971. https://doi.org/10.2337/dc07-2451
Faber OK, Binder C (1977) C-peptide response to glucagon. A test for the residual beta-cell function in diabetes mellitus. Diabetes 26(7):605–610. https://doi.org/10.2337/diab.26.7.605
Panero F, Novelli G, Zucco C et al (2009) Fasting plasma C-peptide and micro- and macrovascular complications in a large clinic-based cohort of type 1 diabetic patients. Diabetes Care 32(2):301–305. https://doi.org/10.2337/dc08-1241
The DCCT Research Group (1998) Effect of intensive therapy on residual beta-cell function in patients with type 1 diabetes in the diabetes control and complications trial. A randomized, controlled trial. The Diabetes Control and Complications Trial Research Group. Ann Intern Med 128:517–523
Greenbaum CJ, Anderson AM, Dolan LM et al (2009) Preservation of beta-cell function in autoantibody-positive youth with diabetes. Diabetes Care 32(10):1839–1844. https://doi.org/10.2337/dc08-2326
Sorensen JS, Vaziri-Sani F, Maziarz M et al (2012) Islet autoantibodies and residual beta cell function in type 1 diabetes children followed for 3-6 years. Diabetes Res Clin Pract 96(2):204–210. https://doi.org/10.1016/j.diabres.2011.12.013
Davis AK, DuBose SN, Haller MJ et al (2015) Prevalence of detectable C-peptide according to age at diagnosis and duration of type 1 diabetes. Diabetes Care 38(3):476–481. https://doi.org/10.2337/dc14-1952
Xu P, Qian X, Schatz DA, Cuthbertson D, Krischer JP, Group DPTS (2014) Distribution of C-peptide and its determinants in North American children at risk for type 1 diabetes. Diabetes Care 37(7):1959–1965. https://doi.org/10.2337/dc13-2603
Mortensen HB, Hougaard P, Swift P et al (2009) New definition for the partial remission period in children and adolescents with type 1 diabetes. Diabetes Care 32(8):1384–1390. https://doi.org/10.2337/dc08-1987
Andersen ML, Rasmussen MA, Pörksen S et al (2013) Complex multi-block analysis identifies new immunologic and genetic disease progression patterns associated with the residual β-cell function 1 year after diagnosis of type 1 diabetes. PLoS One 8(6):e64632. https://doi.org/10.1371/journal.pone.0064632
Max Andersen ML, Hougaard P, Pörksen S et al (2014) Partial remission definition: validation based on the insulin dose-adjusted HbA1c (IDAA1C) in 129 Danish children with new-onset type 1 diabetes. Pediatr Diabetes 15(7):469–476. https://doi.org/10.1111/pedi.12208
Nagl K, Hermann JM, Plamper M et al (2017) Factors contributing to partial remission in type 1 diabetes: analysis based on the insulin dose-adjusted HbA1c in 3657 children and adolescents from Germany and Austria. Pediatr Diabetes 18(6):428–434. https://doi.org/10.1111/pedi.12413
Nielens N, Polle O, Robert A, Lysy PA (2018) Integration of routine parameters of glycemic variability in a simple screening method for partial remission in children with type 1 diabetes. J Diabetes Res 2018:5936360
Redondo MJ, Libman I, Cheng P et al (2018) Racial/ethnic minority youth with recent-onset type 1 diabetes have poor prognostic factors. Diabetes Care 41(5):1017–1024. https://doi.org/10.2337/dc17-2335
Lundberg RL, Marino KR, Jasrotia A et al (2017) Partial clinical remission in type 1 diabetes: a comparison of the accuracy of total daily dose of insulin of <0.3 units/kg/day to the gold standard insulin-dose adjusted hemoglobin A1c of ≤9 for the detection of partial clinical remission. J Pediatr Endocrinol Metab 30(8):823–830. https://doi.org/10.1515/jpem-2017-0019
Boyle KD, Keyes-Elstein L, Ehlers MR et al (2016) Two- and four-hour tests differ in capture of c-peptide responses to a mixed meal in type 1 diabetes. Diabetes Care 39(6):e76–e78. https://doi.org/10.2337/dc15-2077
Wentworth JM, Bediaga NG, Giles LC et al (2018) Beta cell function in type 1 diabetes determined from clinical and fasting biochemical variables. Diabetologia. https://doi.org/10.1007/s00125-018-4722-z
Barker A, Lauria A, Schloot N et al (2014) Age-dependent decline of beta-cell function in type 1 diabetes after diagnosis: a multi-centre longitudinal study. Diabetes Obes Metab 16(3):262–267. https://doi.org/10.1111/dom.12216
Ludvigsson J, Carlsson A, Deli A et al (2013) Decline of C-peptide during the first year after diagnosis of type 1 diabetes in children and adolescents. Diabetes Res Clin Pract 100(2):203–209. https://doi.org/10.1016/j.diabres.2013.03.003
Kuhtreiber WM, Washer SL, Hsu E et al (2015) Low levels of C-peptide have clinical significance for established type 1 diabetes. Diabet Med 32(10):1346–1353. https://doi.org/10.1111/dme.12850
Wang L, Lovejoy NF, Faustman DL (2012) Persistence of prolonged C-peptide production in type 1 diabetes as measured with an ultrasensitive C-peptide assay. Diabetes Care 35(3):465–470. https://doi.org/10.2337/dc11-1236
Funding
Funding for the author’s lab work on residual beta cell function is supported by the Novo Nordisk Foundation and the Innovative Medicines Initiative 2 Joint Undertaking under grant agreement No 115797 (INNODIA), which receives support from the European Union’s Horizon 2020 research and innovation programme and EFPIA, JDRF and The Leona M. and Harry B. Helmsley Charitable Trust.
Author information
Authors and Affiliations
Contributions
The author was the sole contributor to this paper.
Corresponding author
Ethics declarations
The author declares that there is no duality of interest associated with this manuscript.
Rights and permissions
About this article
Cite this article
Pociot, F. Capturing residual beta cell function in type 1 diabetes. Diabetologia 62, 28–32 (2019). https://doi.org/10.1007/s00125-018-4768-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-018-4768-y