Abstract
Aims/hypothesis
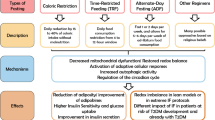
Pioglitazone (PIO) is a peroxisome proliferator-activated receptor (PPAR)γ agonist insulin-sensitiser with anti-inflammatory and anti-atherosclerotic effects. Our objective was to evaluate the effect of low-dose PIO (15 mg/day) on glucose metabolism and inflammatory state in obese individuals with type 2 diabetes.
Methods
A randomised, double-blind, placebo-controlled, mechanistic trial was conducted on 29 patients with type 2 diabetes treated with metformin and/or sulfonylurea. They were randomised to receive PIO or placebo (PLC) for 6 months, in a 1:1 ratio. Participants were allocated to interventions by central office. All study participants, investigators and personnel performing measurements were blinded to group assignment. At baseline and after 6 months patients underwent: (1) OGTT; (2) muscle biopsy to evaluate expression of TNF-α, tissue inhibitor of metalloproteases 3 (TIMP-3) levels, TNF-α converting enzyme (TACE) expression and enzymatic activity; (3) euglycaemic–hyperinsulinaemic clamp; (4) measurement of plasma high-sensitivity C-reactive protein (hsCRP), plasminogen activator inhibitor type-1 (PAI-1), TNF-α, IL-6, monocyte chemotactic protein-1 (MCP-1), adiponectin and fractalkine (FRK). The interventions were PIO 15 mg/day vs placebo and the main outcomes measured were absolute changes in whole-body insulin sensitivity, insulin secretion and inflammatory state.
Results
Fifteen participants were randomized to receive PIO and 14 participants were randomized to receive PLC. Eleven participants completed the study in the PIO group and nine participants completed the study in the PLC group and were analysed. Fasting plasma glucose and HbA1c decreased modestly (p < 0.05) after PIO and did not change after PLC. M/I (insulin-stimulated whole-body glucose disposal), adipose tissue insulin resistance (IR) index, insulin secretion/IR (disposition) index and insulinogenic index improved significantly after PIO, but not after PLC. Circulating MCP-1, IL-6, FRK, hsCRP and PAI-1 levels decreased in PIO- as compared with PLC-treated patients, while TNF-α did not change. TNF-α protein expression and TACE enzymatic activity in muscle were significantly reduced by PIO but not PLC. Adiponectin levels increased significantly after PIO as compared with PLC treatment. Given that the mean TACE enzymatic activity level at baseline in the PIO group was 0.29 ± 0.07 (fluorescence units [FU]), and at end of study decreased to 0.05 vs 0.14 in the PLC group, the power to reject the null hypothesis that the population means of the PIO and PLC groups are equal after 6 months is greater than 0.80. Given that M/I was 2.41 ± 0.35 μmol kg−1 min−1 (pmol/l)−1 at baseline and increased by 0.55 in the PIO and 0.17 in the PLC groups, the power to reject the null hypothesis that the population means of the PIO and PLC groups are equal after 6 months is greater than 0.85. The type I error probability associated with this test of this null hypothesis is 0.05. No serious adverse events occurred in either group.
Conclusions/interpretation
Low-dose PIO (15 mg/day) improves glycaemic control, beta cell function and inflammatory state in obese patients with type 2 diabetes.
Trial registration
Clinical.Trial.gov NCT01223196
Funding
This study was funded by TAKEDA.
Similar content being viewed by others
Introduction
Insulin resistance (IR) is a characteristic feature of the pathogenesis of type 2 diabetes mellitus and is present long before its diagnosis [1, 2]. IR and type 2 diabetes mellitus are associated with a higher cardiovascular disease risk factor profile and accelerated atherogenesis [3]. The mechanistic link between IR, diabetes and cardiovascular disease is not fully elucidated, although obesity (particularly visceral obesity) is associated with increased cardiovascular morbidity and mortality [4, 5]. Adipose tissue is an important endocrine organ, secreting a variety of hormones and cytokines. Circulating adipokines, including TNF-α and IL-6, may in part be responsible for the metabolic, haemodynamic and haemostatic abnormalities associated with IR in the context of obesity [6–8]. Fractalkine (FRK) is a novel membrane-bound chemokine expressed in macrophages, endothelial cells and adipose tissue, as well as in smooth muscle cells, monocytes, natural killer cells and T cells. FRK plays a role in cell migration, adhesion and proliferation and thus it has been postulated to contribute to atherogenesis [9]. In type 2 diabetes, thiazolidinediones (TZDs) improve insulin sensitivity in muscle and liver and prevent diabetes in patients with impaired glucose tolerance [10, 11]. TZDs have potent anti-inflammatory, anti-atherosclerotic and cardioprotective effects and improve circulating levels of inflammatory biomarkers such as C-reactive protein, adiponectin, monocyte chemo-attractant protein-1 (MCP-1), matrix metalloproteinase-9 (MMP-9), a marker of plaque instability and plasminogen activator inhibitor type-1 (PAI-1) [12–15]. Pioglitazone (PIO) is usually employed to treat individuals with type 2 diabetes at doses ranging from 30 to 45 mg/day, which are associated with a dose-dependent increase in body weight, mainly due to an increase in adipose tissue [16, 17]. Fluid retention may also occur in up to 5–10% of diabetic patients treated with PIO, possibly accelerating the onset of congestive heart failure (CHF) [18, 19]. The risk of CHF and the increase in body weight remain major drawbacks for the use of PIO in clinical practice [18–20]. Since these side effects are dose dependent, we hypothesised that a lower dose (15 mg/day) of PIO would still produce glyco-metabolic, as well as anti-inflammatory, beneficial effects, with minimal weight gain and fluid retention in type 2 diabetes mellitus.
Methods
Trial design
Sixty obese individuals with type 2 diabetes (age 18–70 years, BMI 30–40 kg/m2, HbA1c < 10% [86 mmol/mol]) treated with diet alone or diet plus metformin and/or sulfonylurea were screened. Patients who had been previously treated with insulin or TZDs were excluded. Only diabetic patients who were free of other major organ disease, whose body weight was stable for at least 3 months and who did not participate in strenuous exercise were enrolled. Thirty-one individuals did not fulfil the enrolment (inclusion/exclusion) criteria and 29 individuals were randomised, 15 to receive treatment with PIO and 14 to receive placebo (PLC). In the PLC group, three patients were lost to follow-up because they left the area and two patients withdrew consent because they were unwilling to repeat the muscle biopsy; nine patients in the PLC group completed the study. In the PIO group, three patients were lost to follow-up because they left the area and one patient withdrew consent because he/she was unwilling to repeat the muscle biopsy; 11 patients in the PIO group completed the study (Fig. 1). Twenty obese patients with type 2 diabetes treated with sulfonylureas and/or metformin completed the 6 months double-blind, placebo-controlled, randomised trial evaluating the effects of the addition of low-dose PIO (15 mg/day) or PLC on gluco-metabolic control, insulin sensitivity, insulin secretion and sub-inflammatory state. Before the initiation of therapy, all participants received dietary counselling and were asked to consume a standard ADA, weight-maintaining diet throughout the study. At baseline, eligible patients underwent:(1) OGTT; (2) vastus lateralis muscle biopsy; (3) euglycaemic–hyperinsulinaemic clamp; (4) dual-energy x-ray absorptiometry (DEXA scan); (5) measurement of plasma adipocytokines and inflammatory markers. Patients were evaluated in follow-up visits at 1, 3 and 5 months and on each of these visits, blood pressure, pulse rate and weight were determined. The presence of oedema was also determined. At 1–3 and 5 months a blood sample was obtained for measurement of adipocytokines and inflammatory markers. At 6 months, all baseline measurements were repeated.
Ethics
The study protocol was approved by the Institutional Review Board of the University of Texas Health Science Center and of the South Texas Veterans Healthcare System, Audie Murphy Hospital at San Antonio. The study protocol was conducted in accordance with the guidelines of the Declaration of Helsinki. Written and oral informed consent was obtained from all participants enrolled in this study. The study was registered at Clinical-Trials.gov (registration no. NCT01223196).
Study procedures
All tests were carried out at The Bartter Clinical Research Unit of the South Texas Veterans Healthcare System, in the morning after a 10–12 h overnight fast.
OGTT
-
1.
A catheter was placed in an antecubital vein and blood samples were collected at −30, −15, 0, 30, 60, 90 and 120 min for determination of plasma glucose (PG), NEFA, C-peptide and insulin concentrations. Insulin secretory rate (ISR) was calculated by plasma C-peptide, as previously described [21].
-
2.
Insulin secretion/IR index (also called disposition index) was calculated as: [ΔISR 0–120 (AUC)/ΔG 0–120 (AUC)] × [glucose infusion rate (M)/steady-state plasma insulin concentration (I)]. M/I is derived from the euglycaemic–hyperinsulinaemic clamp. Under steady-state conditions of euglycaemia, M divided by I provides a direct measure of whole-body insulin sensitivity (M/I value; μmol kg−1 min−1 (pmol/l)−1).
-
3.
The first phase of insulin secretion (acute insulin response or insulinogenic index) was calculated in the initial 30 min of the OGTT (ΔI 0–30/ΔG 0–30). ΔI (0–30) and ΔG (0–30) are the differences between baseline and 30 min during the OGTT in insulin (I) and glucose (G), respectively.
-
4.
Adipose tissue IR index was calculated as fasting insulin concentration × fasting NEFA concentration.
Skeletal muscle biopsies and western blot
Thirty minutes before the beginning of the OGTT, a vastus lateralis muscle biopsy was performed, as previously described [22]. All muscle biopsy samples were immediately frozen and stored in liquid nitrogen until processed. Western blot experiments were performed as described previously [23]. Protein samples (30 μg) were separated using 7.5–10–12.5% SDS gel electrophoresis (Bio-Rad, Hercules, CA, USA) and electrotransferred to nitrocellulose membranes (Amersham Pharmacia Biotech, Piscataway, NJ, USA). The membranes were probed with antibodies (1:500; Abcam, Cambridge, MA, USA) against TNF-α, TNF-α converting enzyme (TACE) and tissue inhibitor of metalloproteases 3 (TIMP-3). Equal protein loading was confirmed by reblotting the membranes with polyclonal antibody to glyceraldehyde-3-phosphate dehydrogenase (GAPDH) (1:1,000; Cell Signaling Technology, Danvers, MA, USA). Images were analysed and quantified with Quantity One (Bio-Rad). The SensoLyte 520 TACE Activity Assay Kit (AnaSpec EGT Group, Fremont, CA, USA) was used to determine TACE enzymatic activity. Skeletal muscle lysates (50 μg) were probed with a QXL 520/5-FAM FRET substrate containing the cleavage site of TACE. Active TACE cleaves FRET substrate in two separate fragments resulting in an increase of 5-FAM fluorescence, which was monitored at an excitation/emission wavelength of 490/520 nm [23, 24].
Euglycaemic–hyperinsulinaemic clamp
After an overnight fast, catheters were inserted into an antecubital vein for insulin and glucose infusion and the second catheter was inserted retrogradely into a vein on the dorsum of the hand, which was placed into a thermoregulated heated box (55°C). Following collection of three baseline samples, participants received a 4 h euglycaemic insulin clamp (80 mU m−2 min) [25]. The PG concentration was allowed to drop to 5.6 mmol/l, at which it was maintained. Under steady-state conditions of euglycaemia, the glucose infusion rate (M) divided by the steady-state plasma insulin concentration (I) provides a direct measure of whole-body insulin sensitivity (M/I value; μmol kg−1 min−1 (pmol/l)−1).
DEXA DEXA was performed to determine fat and lean body mass and bone mineral density (Hologic, Waltham, MA, USA).
Biochemical analyses
Concentrations of plasma cytokines (TNF-α, IL-6, MCP-1 and FRK) were measured using the human specific Milliplex map kit according to the manufacturer’s instructions (Millipore, St Charles, MO, USA). Total adiponectin, high-sensitivity C-reactive protein (hsCRP) and PAI-1 were measured by ELISA (R&D Systems, Minneapolis, MN, USA). PG levels were measured using the glucose oxidase method (GM9; Analox Instruments, London, UK). Plasma insulin and C-peptide were measured by radioimmunoassay. Plasma NEFA were measured using a colorimetric method (WAKO, Richmond, VA, USA).
Statistical analysis
The AUC of glucose, insulin, C-peptide and adipocytokines during the OGTT and clamp were calculated by the trapezoid rule. Values were measured as mean ± SEM or as median (interquartile range) for variables with a skewed distribution; categorical data were expressed as percentages. Variables that were not normally distributed were log-transformed before analysis. A p value of <0.05 (two-tailed analysis) was considered to be statistically significant. The Mann–Whitney test was used to test differences in anthropometric and metabolic differences between groups. Treatment-induced changes were examined by Wilcoxon’s signed rank test. Multivariate analysis was performed to evaluate the relation between TACE activity changes and metabolic variables. Data were analysed using SPSS 20 (Statistical Package for Social Sciences, Chicago, IL, USA).
Results
Clinical characteristics of the study population
At baseline, participants in the PLC and PIO groups were well matched for clinical, anthropometric and metabolic variables, with no statistically significant differences between the two groups (Table 1).
Changes in body weight and body composition
In the PIO group, there was a small but significant increase in body weight and BMI after 6 months of treatment (from 93.7 ± 4.9 to 95.5 ± 4.9 kg, p = 0.02, and from 33.6 ± 1.9 to 34.2 ± 1.9 kg/m2, p = 0.01, respectively). In the PLC group, weight and BMI did not change significantly. Waist circumference decreased significantly in the PLC group and increased slightly (p = NS) in the PIO group. The percentage body fat was also increased with PIO treatment (from 36.4 ± 2.6 to 38.5 ± 2.6%, p = 0.003) and did not change significantly in the PLC group. In both groups there were no significant changes in bone density, systolic and diastolic blood pressure or HDL-cholesterol. Plasma triacylglycerol levels, total cholesterol and LDL-cholesterol declined significantly in the PIO group. Total cholesterol and LDL-cholesterol decreased significantly also in the PLC group (Table 1).
Glucose metabolism, insulin secretion and beta cell function
Fasting plasma glucose (FPG) and 2 h PG in the OGTT, as well as HbA1c, decreased significantly after 6 months of treatment in the PIO group (p < 0.05) and did not change significantly in the PLC group (Table 1). The M/I value during the euglycaemic–hyperglycaemic insulin clamp improved significantly in the PIO group (from 2.41 ± 0.35 to 2.96 ± 0.45 μmol kg−1 min−1 (pmol/l)−1, p = 0.04) and did not change significantly in the PLC group (from 2.66 ± 0.32 to 2.83 ± 0.45 μmol kg−1 min−1 (pmol/l)−1 p = 0.46) (Fig. 2a). The Δ change in M/I was significantly higher in the PIO than in the PLC group (+23% vs +6.3%, p = 0.005) (Fig. 2b). Beta cell function, evaluated by the disposition index, improved in PIO-treated participants (increased from 9.8 ± 0.3 to 12.7 ± 0.3, p = 0.04) and did not change in the PLC group (from 6.5 ± 0.2 to 6.2 ± 0.2, p = 0.35) (Fig. 2c). The Δ change in disposition index was significantly higher in the PIO than in the PLC group (+29.8% vs −4.6%, p = 0.002) (Fig. 2d). The insulinogenic index did not change in the PLC group (0.13 ± 0.06 vs 0.14 ± 0.07, p = 0.42) and improved in the PIO group (0.3 ± 0.01 vs 0.4 ± 0.02, p = 0.04) (Fig. 2e). The Δ change in insulinogenic index was significantly higher in the PIO than in the PLC group (+33% vs +8%, p = 0.006) (Fig. 2f). The adipose tissue IR index was significantly reduced after PIO treatment (from 5.4 ± 0.9 to 2.9 ± 0.8, p = 0.043) and was slightly increased in the PLC group (from 3.1 ± 0.8 to 4.2 ± 0.9, p = 0.12) (Fig. 2g). The Δ change was reduced in the PIO group, while it was increased in the PLC group (−46% vs +34%, p = 0.015, respectively) (Fig. 2h). After 24 weeks the PG concentration during the OGTT did not change in the PLC group and decreased in the PIO group, although not significantly (electronic supplementary material [ESM] Fig. 1a, b). ISR during the OGTT was similar in the PLC and PIO groups as well as plasma C-peptide and insulin concentrations (data not shown). After 6 months ISR decreased slightly in the PIO group (mean AUC: 6,726 ± 827 vs 6,129 ± 868 pmol/min × m2, p = NS) and modestly increased, although not significantly, in the PLC group (mean AUC: 5,091 ± 551 vs 5,298 ± 1,132 pmol/min × m2, p = NS) (ESM. Fig. 1c, d). The plasma C-peptide and insulin concentrations decreased slightly (p = NS) in the PIO group and did not change in the PLC group (data not shown).
Insulin sensitivity and insulin secretion at baseline (BAS) and after 6 months of treatment (EOS) in the PLC and PIO groups. (a) M/I value. (b) Δ Change in M/I value. (c) Insulin secretion/IR (disposition) index. (d) Δ Change in disposition index. (e) Insulinogenic index. (f) Δ Change in insulinogenic index. (g) Adipose tissue IR index. (h) Δ Change in adipose tissue IR index. *p < 0.05, **p < 0.01
Plasma NEFA concentration
NEFA during the OGTT declined slightly in the PIO group and increased slightly in the PLC group after 6 months of treatment, although not significantly (ESM Fig. 1e, f). During the insulin clamp, plasma NEFA concentration did not change in the PLC group after 6 months and decreased slightly in the PIO group, although this reduction was not statistically significant (data not shown).
Inflammatory status assessment
TNF-α expression in skeletal muscle
TACE is the enzyme that produces TNF-α and IL-6 from their precursor proteins, and it is physiologically inhibited by TIMP-3. At baseline, TNF-α protein levels in skeletal muscle were similar in the PIO and PLC group (PIO = 0.26 ± 0.05 relative units [RU] vs PLC = 0.18 ± 0.06 RU, p = NS) (Fig. 3a, b). Following PIO treatment for 6 months, muscle TNF-α decreased by ∼30%, from 0.26 ± 0.05 RU to 0.18 ± 0.05 RU (p = 0.02). In the PLC group, TNF-α levels decreased slightly but not significantly at the end of treatment (0.18 ± 0.06 RU vs 0.14 ± 0.04 RU, p = NS) (Fig. 3b). After correction for age, sex, duration of type 2 diabetes and BMI change, the decrease in TNF-α was significantly higher in the PIO vs PLC group (PIO = 0.078 ± 0.029 RU vs PLC = 0.035 ± 0.026 RU, p = 0.02) (Fig. 3c). We also observed a negative correlation between TNF-α expression at baseline and improvement in HbA1c levels after 6 months (r = −0.5, p = 0.029 after correction for age and sex) (data not shown). At baseline, TACE and TIMP-3 protein levels were similar in the PLC and PIO groups, and did not change significantly in either group after treatment (Fig. 3a, d, e). To further investigate the mechanisms underlying the changes in skeletal muscle TNF-α protein, we evaluated the TACE enzymatic activity in muscle extracts by an in vitro fluorometric assay, as previously described [23, 24]. At baseline, TACE enzymatic activity levels in skeletal muscle were not significantly different between the PLC and PIO group (0.22 ± 0.1 fluorescence units [FU] vs 0.29 ± 0.07 FU, p = 0.34) (Fig. 3f). After 6 months of treatment with PIO, TACE activity levels were decreased by >80% as compared with baseline (0.29 ± 0.07 FU vs 0.05 ± 0.01 FU, p = 0.005) whereas in the PLC group, TACE activity levels were reduced by ∼36% in comparison with baseline (0.22 ± 0.1 FU vs 0.14 ± 0.07 FU, p = 0.065) (Fig. 3f). The reduction in TACE activity in the PIO group was significantly higher than in the PLC group (0.24 ± 0.06 FU vs 0.08 ± 0.03 FU, p = 0.047) (Fig. 2g). TACE activity changes observed at the end of treatment in comparison with baseline were significantly correlated with changes in HbA1c (r = 0.59, p = 0.019) and FPG (r = 0.70, p = 0.004) in the whole study population after correction for age, sex and BMI (Table 2). In PIO-treated patients the changes in TACE activity correlated with HbA1c (r = 0.87, p = 0.01) and FPG (r = 0.88, p = 0.01). In the PLC group, TACE activity correlated with HbA1c (r = 0.87, p = 0.051). To further evaluate the independent association of the changes in HbA1c and FPG with changes in TACE activity in the whole study population, we performed a multivariate regression analysis in a model including age, sex and BMI. We found that TACE activity was significantly correlated with HbA1c (β = 0.65, r = 0.6, p = 0.02) and FPG (β = 0.77, r = 0.7, p = 0.004).
Skeletal muscle protein expression and enzymatic activity, at baseline (BF, BAS) and after 6 months of treatment (AF, EOS), of TIMP-3, TACE and their product TNF-α (PLC n = 9 and PIO n = 11 individuals, respectively). (a) Western blot of TNF-α, TACE, TIMP-3 and GAPDH. (b) TNF-α protein levels in skeletal muscle, in RU vs GAPDH. (c) ΔTNF-α protein expression. (d) TIMP-3 protein levels in PLC and PIO groups. (e) TACE protein levels in PLC and PIO groups. (f) TACE enzymatic activity in PLC and PIO groups. (g) Δ TACE enzymatic activity. *p < 0.05, **p < 0.01
Circulating cytokines and inflammation marker levels
Baseline plasma TNF-α, MCP-1, IL-6 and FRK concentrations were significantly increased in the PLC group and they declined progressively at 5 and 6 months, generally reaching the levels observed in the PIO group, at the end of the study (Fig. 4a–d). In the PIO group, plasma IL-6, FRK and MCP-1 remained quite constant during the 6 months’ treatment period. Overall IL-6, FRK, MCP-1 and, to a lesser extent, TNF-α levels were lower in the PIO group than in the PLC group. Furthermore, the levels of cytokines were also reduced in both OGTT and the euglycaemic–hyperinsulinaemic clamp after 6 months of treatment with PIO, but not after PLC (data not shown). To further evaluate the anti-inflammatory/anti-atherogenic effects of PIO, we measured total adiponectin, hsCRP and PAI-1. Interestingly, after 6 months of treatment, adiponectin levels were increased in the PIO group (from 40.9 ± 3.5 to 70.8 ± 9.6 ng/ml, p = 0.006) but not in the PLC group (34.5 ± 4.6 vs 41.1 ± 5.8 ng/ml, p = 0.59) (Fig. 5a). The Δ change in adiponectin levels was significantly higher in the PIO group than in the PLC group (+78% vs +14%, p = 0.03) (Fig. 5b). hsCRP concentrations were also significantly decreased in the PIO group after 6 months of treatment (from 6.3 ± 1.3 to 4.1 ± 0.8 ìg/ml, p = 0.03) as compared with the PLC group (5.7 ± 2.2 vs 4.8 ± 1.0 ìg/ml, p = 0.48) (Fig. 5c). The Δ change in hsCRP was significantly reduced in the PIO group but not in the PLC group (−33% vs −17%, p = 0.02, respectively) (Fig. 5d). PAI-1 levels were strongly reduced after PIO treatment (from 3.7 ± 0.8 to 1.4 ± 0.4 ng/ml, p < 0.001) and did not change in the PLC group (8.7 ± 2.6 vs 8.3 ± 2.5 ng/ml, p = 0.41) (Fig. 5e). The Δ change in PAI-1 level was significantly reduced in the PIO group as compared with the PLC group (−60% vs −5%, p < 0.001, respectively) (Fig. 5f).
Discussion
The present study demonstrates that low-dose PIO (15 mg/day) ameliorates glyco-metabolic control, beta cell function and inflammatory state in type 2 diabetes. This was a 6 month, randomised double-blind, placebo-controlled, single-centre study, which included euglycaemic–hyperinsulinaemic clamp, OGTT, serial cytokine measurements and skeletal muscle biopsies with evaluation of TNF-α protein, TACE enzymatic activity and levels of key insulin-signalling proteins. The data on the effect of TZD treatment on insulin secretion in patients with type 2 diabetes mellitus are controversial, with some studies showing an improvement in beta cell function and others failing to observe any significant change [26, 27]. In the present study, low-dose PIO caused a significant reduction in HbA1c (0.5%), which was associated with an improvement in whole-body insulin sensitivity (M/I value) and improvement in beta cell function, as demonstrated by increases in the insulin secretion/IR (disposition) and insulinogenic indexes. Moreover, adipose tissue sensitivity was also improved by PIO treatment. In contrast, whole-body insulin sensitivity, adipose tissue sensitivity and beta cell function did not improve in PLC-treated patients.
Higher doses of PIO (30–45 mg/day) or rosiglitazone (8 mg/day) typically are characterised by a substantial weight gain (4–5 kg) over 1–3 years of treatment, due to increased fat mass and fluid retention [11, 12, 14–19]. In type 2 diabetes mellitus, obesity causes worsening of IR and deterioration of glycaemic control despite aggressive therapy. In the present study, no patient treated with low-dose PIO developed oedema and weight gain was relatively modest (≅2 kg) over 6 months of treatment. It is possible that the lower increase in body weight that we observed could be related to the shorter duration of treatment, in combination with the lower PIO dose. Moreover, the weight gain was significantly and directly correlated with decreases in HbA1c (r = −0.46, p < 0.05), FPG (r = −0.30, p < 0.05) and mean PG concentration during OGTT (r = −0.45, p < 0.05) in the PIO group as previously described [11, 16, 28].
To our knowledge, only two previous studies employing low-dose PIO have evaluated its effect on inflammation in patients with type 2 diabetes. Aso et al reported a decrease in HbA1c associated with increase of HOMA of insulin resistance (HOMA-IR) in a low-dose PIO (7.5 mg/day) study, with a concurrent increase in high-molecular-weight adiponectin after 12 weeks of treatment [29]. In the present study, we also confirmed that adiponectin levels increased significantly only in the PIO group.
Kato et al showed that significant decreases in HbA1c and HOMA-IR after 12 weeks of low-dose PIO (15 mg/day) were associated with a significant reduction in hsCRP [30]. In this study we confirmed a strong reduction in hsCRP levels in the PIO group as compared with the PLC group. Similarly, we demonstrated a significant reduction in PAI-1 levels in the PIO group during the 6 months of treatment, while there was no change in the PLC group, consistent with the possibility that PIO may also have anti-atherogenic effects.
PIO, acting on peroxisome proliferator-activated receptor γ (PPARγ) in adipose tissue and liver, modulates a numbers of metabolic and inflammatory processes that are potentially involved in cardiovascular risk, including endothelial dysfunction, release of adhesion molecules and mediators of cell survival and coagulation/fibrinolysis [31]. In the present study we demonstrated a PIO treatment resulted in a ≅ 30% decrease in TNF-α protein levels in muscle. Interestingly, we observed a negative correlation between TNF-α protein expression in muscle at baseline and improvement of HbA1c levels over 6 months. We have previously shown a dysregulation of the TIMP3–TACE dyad, which regulates, among other things, TNF-α release from the skeletal muscle into the circulation in individuals affected by obesity and type 2 diabetes [23]. In this study, we demonstrated for the first time that low-dose PIO reduced TNF-α expression and also TACE enzymatic activity in human skeletal muscle, and that these effects were associated with an improvement in HbA1c and FPG, emphasising the role of inflammation in the pathogenesis of IR in type 2 diabetes [32–35]. TNF-α has been shown to promote monocyte adhesion to the endothelium, inhibit endothelial nitric oxide synthase and directly impair insulin signalling by causing serine phosphorylation of insulin receptor and insulin receptor substrate-1 [6]. The present study also demonstrated that low-dose PIO therapy decreased plasma IL-6 levels compared with placebo over the 6 month treatment period, although there was no statistical difference between PIO and PLC in the last month. IL-6 is a pro-inflammatory cytokine that correlates with IR in humans and is associated with atherosclerotic coronary artery disease, possibly through its effect on plaque development and destabilisation [7, 36, 37]. We also demonstrated a reduction in plasma MCP-1 levels compared with PLC over the 6 month period. MCP-1 is involved in chemokine-directed trans-endothelial migration of monocytes, and possibly in plaque rupture and thrombogenesis. PIO, compared with PLC, also reduced the plasma levels of FRK. The soluble form of FRK is released from its membrane form by extracellular cleavage through ADAM metallopeptidase domain ADAM10 and TACE, and then acts as a chemo-attractant for leucocytes and for smooth muscle cells expressing the receptor (i.e. CX3CR1) [38]. Hyperglycaemia, as seen in type 2 diabetes, promotes FRK expression by smooth muscle and endothelial cells in vitro, leading to enhanced monocyte adhesion, which can promote atherogenesis [39]. It has been previously shown that abrogation of FRK signalling by FRK receptor deletion in mice results in reduced accumulation of tissue-specific macrophages such as foam cells at the level of atherogenic lesions and microglial cells at sites of retinal degeneration [40]. In vitro, rosiglitazone has been shown to suppress the membrane translocation of FRK receptors in macrophages and prevent the nuclear export of FRK in endothelial cells [41]. It is noteworthy that Yokoyama et al demonstrated that low-dose PIO (15 mg/day) reduced the incidence of in-stent restenosis without adversely affecting left ventricular remodelling after acute myocardial infarction in patients with type 2 diabetes or impaired glucose tolerance [42]. Interestingly, PIO treatment has been shown to be somewhat effective in the late phase of atherosclerosis and the clinical significance of the reduction in TACE activity, as well as plasma levels of IL-6 and FRK, in the prevention/retardation of atherogenesis with low-dose PIO (15 mg/day) remains to be determined [14, 28].
The present study has some limitations, such as the relatively short duration (6 months) of treatment and the limited number of participants studied, which might have reduced the ability to observe a more pronounced effect of PIO on inflammatory markers. On the other hand, it is important to emphasise that this study included the application of a euglycaemic–hyperinsulinaemic clamp to directly assess insulin sensitivity combined with skeletal muscle biopsies for the evaluation of in vivo inflammatory pathways such as the TIM–TACE dyad, which is involved in the generation of TNF-α and IL-6. It must be noted that these studies were performed in a very limited number of patients.
In this study we could not assess changes in the expression of insulin-signalling proteins or changes in their function because we did not perform skeletal muscle biopsies after insulin stimulation. Therefore, we could not evaluate the effect of low-dose PIO on the insulin-signalling mechanism in skeletal muscle. Whole-body glucose uptake was significantly improved after PIO treatment concomitant with the reduction of inflammatory signalling pathways, which are known to inhibit insulin’s action [6–8, 33]. Therefore it can only be hypothesised that insulin signalling was improved at the level of skeletal muscle by PIO; future studies will be necessary to directly assess these phenomena.
In conclusion, low-dose PIO improved glycaemic control, insulin sensitivity and beta cell function, with a very modest concomitant weight gain. Moreover, we demonstrated that low-dose PIO significantly reduced TNF-α protein and TACE enzymatic activity in skeletal muscle and circulating inflammatory cytokines in humans. Altogether, these findings suggest that low-dose PIO treatment, by improving glycaemic control while decreasing inflammation, could have a favourable impact on cardiovascular risk in patients with type 2 diabetes, who are particularly vulnerable to cardiovascular disease.
Abbreviations
- CHF:
-
Congestive heart failure
- DEXA:
-
Dual-energy x-ray absorptiometry
- FRK:
-
Fractalkine
- FPG:
-
Fasting plasma glucose
- FU:
-
Fluorescence units
- GAPDH:
-
Glyceraldehyde-3-phosphate dehydrogenase
- HOMA-IR:
-
HOMA of insulin resistance
- hsCRP:
-
High-sensitivity C-reactive protein
- IR:
-
Insulin resistance
- ISR:
-
Insulin secretory rate
- M/I:
-
Glucose infusion rate (M)/steady-state plasma insulin concentration (I)
- MCP-1:
-
Monocyte chemo-attractant protein-1
- MMP-9:
-
Matrix metalloproteinase-9
- PAI-1:
-
Plasminogen activator inhibitor type-1
- PG:
-
Plasma glucose
- PIO:
-
Pioglitazone
- PLC:
-
Placebo
- PPARγ:
-
Peroxisome proliferator-activated receptor γ
- RU:
-
Relative units
- TACE:
-
TNF-α converting enzyme
- TIMP-3:
-
Tissue inhibitor of metalloproteases 3
- TZD:
-
Thiazolidinedione
References
Del Prato S, Bonadonna RC, Bonora E et al (1993) Characterization of cellular defects of insulin action in type 2 (non-insulin-dependent) diabetes mellitus. J Clin Invest 91:484–494
Martin BC, Warram JH, Krolewski AS et al (1992) Role of glucose and insulin resistance in development of type 2 diabetes mellitus: results of a 25-year follow-up study. Lancet 340:925–929
Haffner SM, D’Agostino R Jr, Mykkänen L et al (1999) Insulin sensitivity in subjects with type 2 diabetes. Relationship to cardiovascular risk factors: the Insulin Resistance Atherosclerosis Study. Diabetes Care 22:562–568
Khashper A, Gaspar T, Azencot M et al (2011) Visceral abdominal adipose tissue and coronary atherosclerosis in asymptomatic diabetics. Int J Cardiol 162:184–188
Preis SR, Hwang SJ, Coady S et al (2009) Trends in all-cause and cardiovascular disease mortality among women and men with and without diabetes in the Framingham Heart Study, 1950–2005. Circulation 119:1728–1735
Hotamisligil GS, Peraldi P, Budavari A, Ellis R, White MF, Spiegelman BM (1996) IRS-1-mediated inhibition of insulin receptor tyrosine kinase activity in TNF-alpha- and obesity-induced insulin resistance. Science 271:665–668
Austin RL, Rune A, Bouzakri K, Zierath JR, Krook A (2008) SiRNA-mediated reduction of inhibitor of nuclear factor-kappaB kinase prevents tumor necrosis factor-alpha-induced insulin resistance in human skeletal muscle. Diabetes 57:2066–2073
Federici M, Hribal ML, Menghini R et al (2005) Timp3 deficiency in insulin receptor-haploinsufficient mice promotes diabetes and vascular inflammation via increased TNF-alpha. J Clin Invest 115:3494–3505
Cefalu WT (2011) Fractalkine: a cellular link between adipose tissue inflammation and vascular pathologies. Diabetes 60:1380–1382
Miyazaki Y, Glass L, Triplitt C et al (2001) Effect of rosiglitazone on glucose and non-esterified fatty acid metabolism in type II diabetic patients. Diabetologia 44:2210–2219
DeFronzo RA, Tripathy D, Schwenke DC et al (2011) Pioglitazone for diabetes prevention in impaired glucose tolerance. N Engl J Med 364:1104–1115
Hanefeld M, Marx N, Pfützner A et al (2007) Anti-inflammatory effects of pioglitazone and/or simvastatin in high cardiovascular risk patients with elevated high sensitivity C-reactive protein: the PIOSTAT Study. J Am Coll Cardiol 49:290–297
Joner M, Farb A, Cheng Q et al (2007) Pioglitazone inhibits in-stent restenosis in atherosclerotic rabbits by targeting transforming growth factor-beta and MCP-1. Arterioscler Thromb Vasc Biol 27:182–189
Dormandy JA, Charbonnel B, Eckland DJ et al (2005) Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive Study (PROspective pioglitAzone Clinical Trial In macroVascular Events): a randomised controlled trial. Lancet 366:1279–1289
Chiquette E, Ramirez G, Defronzo R (2004) A meta-analysis comparing the effect of thiazolidinediones on cardiovascular risk factors. Arch Intern Med 164:2097–2104
Charbonnel B, Schernthaner G, Brunetti P et al (2005) Long-term efficacy and tolerability of add-on pioglitazone therapy to failing monotherapy compared with addition of gliclazide or metformin in patients with type 2 diabetes. Diabetologia 48:1093–1104
Balas B, Belfort R, Harrison SA et al (2007) Pioglitazone treatment increases whole body fat but not total body water in patients with non-alcoholic steatohepatitis. J Hepatol 47:565–570
Delea TE, Edelsberg JS, Hagiwara M, Oster G, Phillips LS (2003) Use of thiazolidinediones and risk of heart failure in people with type 2 diabetes: a retrospective cohort study. Diabetes Care 26:2983–2989
Kaul S, Bolger AF, Herrington D, Giugliano RP, Eckel RH (2010) Thiazolidinedione drugs and cardiovascular risks: a science advisory from the American Heart Association and American College of Cardiology Foundation. Circulation 121:1868–1877
Karalliedde J, Buckingham R, Starkie M, Lorand D, Stewart M, Viberti G (2006) Effect of various diuretic treatments on rosiglitazone-induced fluid retention. J Am Soc Nephrol 17:3482–3490
Hovorka R, Soons PA, Young MA (1996) ISEC: a program to calculate insulin secretion. Comput Methods Programs Biomed 50:253–264
Cusi K, Maezono K, Osman A et al (2000) Insulin resistance differentially affects the PI 3-kinase- and MAP kinase-mediated signaling in human muscle. J Clin Invest 105:311–320
Monroy A, Kamath S, Chavez AO et al (2009) Impaired regulation of the TNF-alpha converting enzyme/tissue inhibitor of metalloproteinase 3 proteolytic system in skeletal muscle of obese type 2 diabetic patients: a new mechanism of insulin resistance in humans. Diabetologia 52:2169–2181
Jin G, Huang X, Black R et al (2002) A continuous fluorimetric assay for tumor necrosis factor-alpha converting enzyme. Anal Biochem 302:269–275
DeFronzo RA, Tobin JD, Andres R (1979) Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol 237:E214–E223
Gastaldelli A, Ferrannini E, Miyazaki Y, Matsuda M, Mari A, DeFronzo RA (2007) Thiazolidinediones improve beta-cell function in type 2 diabetic patients. Am J Physiol Endocrinol Metab 292:E871–E883
Inzucchi SE, Maggs DG, Spollett GR et al (1998) Efficacy and metabolic effects of metformin and troglitazone in type II diabetes mellitus. N Engl J Med 338:867–872
Doehner W, Erdmann E, Cairns R et al (2011) Inverse relation of body weight and weight change with mortality and morbidity in patients with type 2 diabetes and cardiovascular co-morbidity: an analysis of the PROactive study population. Int J Cardiol 29:1–7
Aso Y, Hara K, Ozeki N et al (2009) Low-dose pioglitazone increases serum high molecular weight adiponectin and improves glycemic control in Japanese patients with poorly controlled type 2 diabetes. Diabetes Res Clin Pract 85:147–152
Kato T, Sawai Y, Kanayama H et al (2009) Comparative study of low-dose pioglitazone or metformin treatment in Japanese diabetic patients with metabolic syndrome. Exp Clin Endocrinol Diabetes 117:593–599
Bays H, Mandarino L, DeFronzo RA (2004) Role of the adipocyte, free fatty acids, and ectopic fat in pathogenesis of type 2 diabetes mellitus: peroxisomal proliferator-activated receptor agonists provide a rational therapeutic approach. J Clin Endocrinol Metab 89:463–478
Pedersen BK, Febbraio MA (2012) Muscle, exercise and obesity: skeletal muscle as a secretory hormone. Nat Rev Endocrinol 8:457–465
Shoelson SE, Lee J, Goldfine AB (2006) Inflammation and insulin resistance. J Clin Invest 116:1793–1801
Goldfine AB, Fonseca V, Jablonski KA (2006) The effects of salsalate on glycemic control in patients with type 2 diabetes: a randomized trial. Ann Intern Med 152:346–357
Fernàndez-Real JM, Pérez del Pulgar S, Luche E et al (2011) CD14 modulates inflammation-driven insulin resistance. Diabetes 60:2179–2186
Anfossi G, Russo I, Doronzo G, Pomero A, Trovati M (2010) Adipocytokines in atherothrombosis: focus on platelets and vascular smooth muscle cells. Mediators Inflamm. doi:10.1155/2010/174341
Cardellini M, Perego L, D’Adamo M et al (2005) C-174G polymorphism in the promoter of the interleukin-6 gene is associated with insulin resistance. Diabetes Care 28:2007–2012
Bazan JF, Bacon KB, Hardiman G et al (1997) A new class of membrane-bound chemokine with a CX3C motif. Nature 385:640–644
Dragomir E, Manduteanu I, Calin M et al (2008) High glucose conditions induce upregulation of fractalkine and monocyte chemotactic protein-1 in human smooth muscle cells. Thromb Haemost 100:1155–1165
Saederup N, Chan L, Lira SA, Charo IF (2008) Fractalkine deficiency markedly reduces macrophage accumulation and atherosclerotic lesion formation in CCR2-/- mice: evidence for independent chemokine functions in atherogenesis. Circulation 117:1642–1648
Wan Y, Evans RM (2010) Rosiglitazone activation of PPARgamma suppresses fractalkine signaling. J Mol Endocrinol 44:135–142
Yokoyama J, Sutoh N, Higuma T, Horiuchi D, Katoh C, Yokota T (2007) Efficacy and safety of low-dose pioglitazone after primary coronary angioplasty with the use of bare metal stent in patients with acute myocardial infarction and with type 2 diabetes mellitus or impaired glucose tolerance. Heart Vessels 22:146–151
Acknowledgements
This work was presented in part in abstract form at the ADA meeting, 2012, in Philadelphia, PA, USA. Franco Folli thanks Leslie David Hillis, Department of Medicine, University of Texas Health Science Center at San Antonio, Texas, for continuous generous support.
Funding
This study was funded by TAKEDA. GD and TVF were supported in part by fellowships from Fo.Ri.SID, Italy.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Contribution statement
DT, GD and TVF researched and analysed the data, conceived the study and wrote the manuscript. ZPC, ACV, SK, FA and AG researched and analysed the data and critically revised the manuscript for important intellectual content. PF, CJ, MF and RAD analysed and interpreted the data and critically revised the manuscript for important intellectual content. FF conceived the study, researched, analysed and interpreted the data, wrote the manuscript, contributed to the discussion and reviewed the final version of the manuscript.
All authors gave final approval of the version of the manuscript to be published.
Author information
Authors and Affiliations
Corresponding author
Additional information
Devjit Tripathy, Giuseppe Daniele and Teresa V. Fiorentino contributed equally as first authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM Fig. 1
OGTT data at baseline and end of treatment A-B: Plasma glucose levels in PLC and PIO groups; C-D: Insulin secretion rate in PLC and PIO groups; E-F: NEFA levels during OGTT in PLC and PIO groups. Open circle: baseline; Full square: end of study. *p < 0.05. (PDF 34 kb)
Rights and permissions
About this article
Cite this article
Tripathy, D., Daniele, G., Fiorentino, T.V. et al. Pioglitazone improves glucose metabolism and modulates skeletal muscle TIMP-3–TACE dyad in type 2 diabetes mellitus: a randomised, double-blind, placebo-controlled, mechanistic study. Diabetologia 56, 2153–2163 (2013). https://doi.org/10.1007/s00125-013-2976-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-013-2976-z