Abstract
Background
An increasing number of studies have shown that low tidal volume (TV) with positive end-expiratory pressure (PEEP) offers lung protection during one-lung ventilation (OLV). Considering the unique physiological characteristics of infants, we aimed to determine the feasibility and effect of low TV with PEEP in infants undergoing OLV during thoracoscopy.
Patients and methods
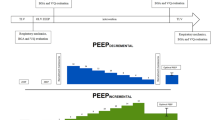
We randomized 60 infants to a conventional group (group I: TV, 8–10 ml/kg; RR, 23–45 bpm; PEEP, 0 cmH2O) or a low TV with PEEP group (group II: TV, 5–7 ml/kg; RR, 23–45 bpm; PEEP, 4–6 cmH2O). Arterial blood gas analyses were performed at four time points: 5 min of two-lung ventilation (TLV, T0), and 20 min, 40 min, and 60 min of OLV (T1, T2, T3); hemodynamic parameters (heart rate, mean blood pressure), temperature, as well as gas exchange (SpO2 and PETCO2) and ventilation parameters (FiO2, PEEP, Pmax) were recorded simultaneously. Lung compliance and shunt were also calculated.
Result
No significant difference was found between both groups at T0. Compared with T0, PETCO2, Pmax, PaCO2, lactic acid, and intrapulmonary shunt volume (Qs/Qt) were increased while PaO2 and respiratory system compliance (Cdyx) were decreased noticeably in both groups at T1, T2, and T3. At T1, T2, and T3, Pmax and Qs/Qt were much lower while PETCO2, PaCO2, and Cdyx were higher in group II than in group I. There was no significant difference in lactic acid and PaO2 measurements between the two groups at T1, T2, and T3.
Conclusion
Low TV with PEEP could be an effective intraoperative ventilation strategy for infants undergoing OLV during video-assisted thoracoscopic surgery and may reduce the risk of lung injury. However, this strategy, as well as the influence of intraoperative hypercapnia on infants, needs further investigation.
Zusammenfassung
Hintergrund
In immer mehr Studien zeigt sich, dass ein niedriges Atemzugvolumen (AZV) bei positivem endexpiratorischem Druck („positive end-expiratory pressure“, PEEP) die Lunge unter Ein-Lungen-Ventilation („one-lung ventilation“, OLV) schont. Unter Berücksichtigung der physiologischen Besonderheiten von Säuglingen war es Ziel der Autoren, die Praktikabilität und Wirkung eines niedrigen AZV bei PEEP für Säuglinge während einer Thorakoskopie unter OLV zu untersuchen.
Patienten und Methoden
Es wurden 60 Säuglinge auf die konventionelle Gruppe (Gruppe I; AZV: 8–10 ml/kg; Atemfrequenz, AF: 23–45/min; PEEP: 0 cmH2O) oder auf die Gruppe mit niedrigem AZV bei PEEP randomisiert (Gruppe II; AZV: 5–7 ml/kg; AF: 23–45/min; PEEP: 4–6 cmH2O). Arterielle Blutgasanalysen erfolgten zu 4 Zeitpunkten: 5 min 2‑Lungen-Ventilation („two-lung ventilation“, TLV, T0) sowie 20 min, 40 min und 60 min OLV (T1, T2, T3); hämodynamische Parameter (Herzfrequenz, mittlerer Blutdruck), Temperatur sowie Gasaustausch- (pulsoxymetrisch gemessene Sauerstoffsättigung, SpO2, und endtidaler Kohlendioxidpartialdruck, PETCO2) und Beatmungsparameter (inspiratorische Sauerstoffkonzentration, FiO2; PEEP; maximaler Atemwegsdruck, Pmax) wurden gleichzeitig erfasst. Lungencompliance und -shunt wurden ebenfalls ermittelt.
Ergebnisse
Es wurde kein signifikanter Unterschied zwischen beiden Gruppen an T0 festgestellt. Dagegen waren in beiden Gruppen PETCO2, Pmax, PaCO2 (arterieller CO2-Partialdruck), Milchsäure und intrapulmonales Shuntvolumen (Qs/Qt) erhöht, während PaO2 (arterieller O2-Partialdruck) und die Compliance des respiratorischen Systems (Cdyx) an T1, T2 und T3 deutlich erniedrigt waren. An T1, T2 und T3 waren Pmax und Qs/Qt viel niedriger, während PETCO2, PaCO2 und Cdyx in Gruppe II höher als Gruppe I waren. Zwischen den beiden Gruppen bestand kein signifikanter Unterschied bei Milchsäure und PaO2 an T1, T2 und T3.
Schlussfolgerung
Ein niedriges AZV bei PEEP könnte eine wirksame intraoperative Beatmungsform für Säuglinge unter OLV während videoassistierter thorakoskopischer Operationen (VATS) darstellen und das Risiko einer Lungenschädigung vermindern. Jedoch sind weitere Studien dieses Vorgehens sowie des Einflusses der intraoperativen Hyperkapnie auf Säuglinge erforderlich.
Similar content being viewed by others
References
Hare GM, Kavanagh BP, Mazer CD et al (2003) Hypercapnia increases cerebral tissue oxygen tension in anesthetized rats. Can J Anaesth 50(10):1061–1068
Dimitriou G, Greenough A, Pink L, McGhee A, Hickey A, Rafferty GF (2002) Effect of posture on oxygenation and respiratory muscle strength in convalescent infants. Arch Dis Child Fetal Neonatal Ed 86(3):F147–F150
Hammer GB (2004) Single-lung ventilation in infants and children. Paediatr Anaesth 14(1):98–102
Heaf DP, Helms P, Gordon I, Turner HM (1983) Postural effects on gas exchange in infants. N Engl J Med 308(25):1505–1508
Katz JA, Laverne RG, Fairley HB, Thomas AN (1982) Pulmonary oxygen exchange during endobronchial anesthesia: effect of tidal volume and PEEP. Anesthesiology 56(3):164–171
Baudouin SV (2003) Lung injury after thoracotomy. Br J Anaesth 91(1):132–142
Fernandez-Perez ER, Keegan MT, Brown DR, Hubmayr RD, Gajic O (2006) Intraoperative tidal volume as a risk factor for respiratory failure after pneumonectomy. Anesthesiology 105(1):14–18
Hemmes SN, Serpa NA, Schultz MJ (2013) Intraoperative ventilatory strategies to prevent postoperative pulmonary complications: a meta-analysis. Curr Opin Anaesthesiol 26(2):126–133
The Acute Respiratory Distress Syndrome Network (2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 342(18):1301–1308
Severgnini P, Selmo G, Lanza C et al (2013) Protective mechanical ventilation during general anesthesia for open abdominal surgery improves postoperative pulmonary function. Anesthesiology 118(6):1307–1321
Frost EA, Arancibia CU, Shulman K (1979) Pulmonary shunt as a prognostic indicator in head injury. J Neurosurg 50(6):768–772
Kozian A, Schilling T, Rocken C, Breitling C, Hachenberg T, Hedenstierna G (2010) Increased alveolar damage after mechanical ventilation in a porcine model of thoracic surgery. J Cardiothorac Vasc Anesth 24(4):617–623
Licker M, Diaper J, Villiger Y et al (2009) Impact of intraoperative lung-protective interventions in patients undergoing lung cancer surgery. Crit Care 13(2):R41
Senturk M (2006) New concepts of the management of one-lung ventilation. Curr Opin Anaesthesiol 19(1):1–4
Perilli V, Sollazzi L, Modesti C et al (2003) Comparison of positive end-expiratory pressure with reverse Trendelenburg position in morbidly obese patients undergoing bariatric surgery: effects on hemodynamics and pulmonary gas exchange. Obes Surg 13(4):605–609
von Ungern-Sternberg B, Regli A, Frei F, Hammer J, Jordi Ritz E, Erb T (2007) Decrease in functional residual capacity and ventilation homogeneity after neuromuscular blockade in anesthetized preschool children in the lateral position. Paediatr Anaesth 17(9):841–845
Satoh D, Kurosawa S, Kirino W et al (2012) Impact of changes of positive end-expiratory pressure on functional residual capacity at low tidal volume ventilation during general anesthesia. J Anesth 26(5):664–669
Cinnella G, Grasso S, Spadaro S et al (2013) Effects of recruitment maneuver and positive end-expiratory pressure on respiratory mechanics and transpulmonary pressure during laparoscopic surgery. Anesthesiology 118(1):114–122
Marangoni E, Alvisi V, Ragazzi R et al (2012) Respiratory mechanics at different PEEP level during general anesthesia in the elderly: a pilot study. Minerva Anestesiol 78(11):1205–1214
Michelet P, D’Journo XB, Roch A et al (2006) Protective ventilation influences systemic inflammation after esophagectomy: a randomized controlled study. Anesthesiology 105(5):911–919
Roze H, Lafargue M, Perez P et al (2012) Reducing tidal volume and increasing positive end-expiratory pressure with constant plateau pressure during one-lung ventilation: effect on oxygenation. Br J Anaesth 108(6):1022–1027
Tusman G, Böhm S, Tempra A et al (2003) Effects of recruitment maneuver on atelectasis in anesthetized children. Anesthesiology 98(1):14–22
Hickling KG, Henderson SJ, Jackson R (1990) Low mortality associated with low volume pressure limited ventilation with permissive hypercapnia in severe adult respiratory distress syndrome. Intensive Care Med 16(6):372–377
Curley G, Contreras MM, Nichol AD, Higgins BD, Laffey JG (2010) Hypercapnia and acidosis in sepsis: a double-edged sword? Anesthesiology 112(2):462–472
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J. Liu, X. Liao, Y. Li, H. Luo, W. Huang, L. Peng, Q. Fang, and Z. Hu declare that they have no competing interests.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Jing Liu and Xinfang Liao contributed equally to this study and share first authorship.
Rights and permissions
About this article
Cite this article
Liu, J., Liao, X., Li, Y. et al. Effect of low tidal volume with PEEP on respiratory function in infants undergoing one-lung ventilation . Anaesthesist 66, 667–671 (2017). https://doi.org/10.1007/s00101-017-0330-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00101-017-0330-4