Abstract
Objective
The aim of the study was to investigate the effects of acute hypervolemic hemodilution (HHD) on the pharmacokinetics of propofol in patients undergoing total hip replacement.
Methods
A total of 16 patients undergoing elective surgery for total hip replacement under general anesthesia in combination with epidural analgesia were randomly assigned to 2 groups: the control group (n = 8) or the HHD group (n = 8). All patients in both groups received lactated Ringer’s solution before induction of general anesthesia. In the control group the conventional fluid replacement protocol was used. In the HHD group 4% succinylated gelatin was infused at the rate of 20 ml•kg−1BW•h−1 with a targeted hematocrit of 30. Anesthesia was induced with midazolam 0.04 mg•kg−1, fentanyl 4 µg•kg−1 and propofol 1.5 mg•kg−1. Tracheal intubation was facilitated by infusion of succinylcholine 2 mg•kg−1. Anesthesia was maintained with isoflurane, fentanyl, vecuronium and epidural analgesia. Electrocardiogram (ECG), blood pressure (BP), blood oxygen saturation (SpO2), partial pressure of end-tidal carbon dioxide (PETCO2) and central venous pressure (CVP) were monitored continuously. Blood samples were taken at 1, 2, 4, 6, 10, 15, 30, 45, 60, 75, 90, 120, 150, 180, 240, 300 and 360 min after propofol administration to determine plasma concentrations of propofol by high performance liquid chromatography (HPLC).
Results
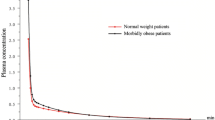
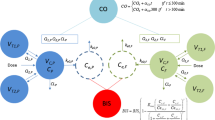
Plasma propofol concentrations were significantly lower in the HHD group than in the control group at 1, 2, 4, 6 and 10 min after propofol administration (p < 0.01) while there were no significant differences in plasma propofol levels 15–360 min after administration of propofol (p > 0.05). In the HHD group the volume of distribution of the central compartment (VC) increased significantly, elimination half-life (T1/2 γ) was significantly prolonged, the elimination rate constant (K10) and the whole-body clearance (CL) were significantly decreased compared with the control group (p < 0.01 or 0.05). There were no significant differences of the half-life of the fast distribution phase (T1/2 α), half-life of the slower distribution phase (T1/2 β), K12, K21, K13, K31 and the area under the curve (AUC) (p > 0.05). The pharmacokinetic profile of propofol is best described by a three-compartment model in both groups using minimal Akaike information criteria (AIC).
Conclusion
Acute HHD increases VC, prolongs the T1/2 γ, and decreases K10 and CL, which suggests that care must be taken when propofol is used in patients undergoing HHD. The induction dose should be increased, but the maintenance dose should be decreased. The time to emergency from anesthesia will likely be prolonged, especially in patients receiving prolonged continuous infusions.
Zusammenfassung
Ziel
Bei Patienten, die sich einer Hüfttotalendoprotheseoperation unterziehen sollte der Einfluss der akuten hypervolämischen Hämodilution (HHD) auf die Pharmakokinetik von Propofol untersucht werden.
Methoden
Es wurden 16 Patienten, die sich der elektiven Implantation einer Hüfttotalendoprothese unterzogen, randomisiert in eine Kontrollgruppe (n = 8) oder eine HHD-Gruppe (n = 8) aufgeteilt. Alle Patienten in beiden Gruppen erhielten vor Beginn der Allgemeinanästhesie Ringer-Laktat-Lösung. Während in der Kontrollgruppe ein konventionelles Flüssigkeitsmanagement betrieben wurde, wurde in der HHD-Gruppe 4%ige Gelatine mit einer Infusionsrate von 20 ml/kgKG/h verabreicht. Eine, 2, 4, 6, 10, 15, 30, 45, 60, 75, 90, 120, 150, 180, 240, 300 und 360 min nach der i.v.-Gabe von Propofol wurden Blutproben abgenommen, um die Propofolplasmakonzentration mithilfe der Hochleistungsflüssigkeitschromatographie zu bestimmen.
Ergebnisse
Plasmapropofolspiegel waren in der HHD-Gruppe 1, 2, 4, 6, 10 min nach Propofolinjektion signifikant niedriger als in der Kontrollgruppe (p < 0,01). Die Plasmapropofolkonzentrationen 15–360 min nach Gabe von Propofol waren hingegen in beiden Gruppen gleich (p > 0,05). In der HHD-Gruppe stieg das Verteilungsvolumen des zentralen Kompartiments (VC) signifikant, die Eliminationshalbwertszeit (T1/2γ) war signifikant verlängert, und die „Clearance“-Rate auf den ganzen Körper bezogen (CL) fiel im Vergleich zur Kontrollgruppe signifikant ab (p < 0,01 oder 0,05). Es gab keinen signifikanten Unterschied in der Halbwertszeit der schnellen Verteilungsphase (T1/2α), der Halbwertszeit der langsamen Verteilungsphase (T1/2β), K12, K21, K13, K31, und der „area under the curve“ (AUC, p > 0,05).
Schlussfolgerung
Die akute HHD erhöht VC, verlängert T1/2γ, erniedrigt K10 und CL. Dies bedeutet klinisch, dass die Induktionsdosis erhöht und die Erhaltungsdosis erniedrigt werden sollte.

Similar content being viewed by others
References
Mielke LL, Entholzner EK, Kling M et al (1997) Preoperative acute hypervolemic haemodilution with hydroxyethylstarch: an alternative to acute normovolemic haemodilution? Anesth Analg 84:26–30
Johnson KB, Egan TD, Kern SE (2003) The Influence of hemorrhagic shock on propofol. a pharmacokinetic and pharmacodynamic analysis. Anesthesiology 99:409–420
Leal N, Calvo R, Agrad FZ et al (2005) Altered dose-to-effect of propofol due to pharmacokinetics in rats with experimental diabetes mellitus. J Pharm Pharmacol 57:317–325
Dong Q, Wen X, Ouyang B (2001) Hemodynamic and hemorheological effects of hypovolemic hemodilution with hydroxyethyl starch. Chin J Anesthesiol 5:265–268
Kumar R, Chakraborty I, Sehgal R (2002) A prospective randomized study comparing two techniques of perioperative blood conservation: isovolemic hemodilution and hypervolemic hemodilution. Anesth Analg 95:1154–1161
Kataria BK, Ved SA, Nicodemus HF et al (1994) The pharmacokinetics of propofol in children using three different data analysis approaches. Anesthesiology 80:104–122
Li YH, Rui JZ, Zhou YG et al (2003) Population pharmacokinetics of propofol in Chinese patients. Acta Pharmacol Sin 24:581–588
Wu J, Wang SJ, Hang YN (2002) Comparison between pharmacokinetics of propofol in the elderly and young patients during induction. Chin J Anesthesiol 22:645–649
Bhattacharya AA, Curry S, Franks NP (2000) Binding of the general anesthetics propofol and halothane to human serum albumin. J Biol Chem 275:38731–38738
Leslie K, Sessler DI, Bjorksten AR et al (1995) Mild hypothermia alters propofol pharmacokinetics and increases the duration of action of atracurium. Anesth Analg 80:1007–1014
Wouters PF, Van de Velde MA, Marcus MA et al (1995) Hemodynamic changes during induction of anesthesia with eltanolone and propofol in dogs. Anesth Analg 81:125–131
Nollert G, Sperling J, Sakamoto T et al (2001) Higher hematocrit improves liver blood flow and metabolism during cardiopulmonary bypass in piglets. Thorac Cardiovasc Surg 49:226–230
Acknowledgements
The study was sponsored by a grant from Board of Health, Shanghai City Science Foundation (034057).
The authors thank the medical and nursing staff of the Department of Anesthesia and clinical pharmacists at the Fifth People’s Hospital of Shanghai for their participation in the study.
Conflict of interest
The corresponding author states that there are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tang, J., Wu, G. & Peng, L. Pharmacokinetics of propofol in patients undergoing total hip replacement. Anaesthesist 60, 835–840 (2011). https://doi.org/10.1007/s00101-011-1907-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00101-011-1907-y