Abstract
Purpose
Intraosseous (IO) catheters continue to be recommended in trauma resuscitation. Their utility has recently been debated due to concerns regarding inadequate flow rates during blood transfusion, and the potential for haemolysis. The objective of this review was to examine the evidence for intraosseous catheters in trauma resuscitation, and to highlight areas for future research.
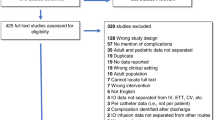
Methods
A PubMed and Embase search for articles published from January 1990 to August 2018 using the terms (“intra-osseous access” or “intraosseous access” or “IO access”) AND trauma was performed. Original articles describing the use of an IO catheter in the resuscitation of one or more trauma patients were eligible. Animal, cadaveric studies and those involving healthy volunteers were excluded.
Results
Nine studies, comprising of 1218 trauma patients and 1432 device insertions, were included. The insertion success rate was 95% and the incidence of complications 0.9%. Flow-rate data and evidence of haemolysis were poorly reported.
Conclusion
Intraosseous catheters have high insertion success rates and a low incidence of complications in trauma patients. Existing evidence suggests that IO transfusion is not associated with haemolysis, however, further studies in humans are needed. There is a paucity of flow rate data for blood transfusion via IO catheters in this population, although much anecdotal evidence advocating their use exists.


Similar content being viewed by others
References
Cannon J, Khan M, Raja A, Cohen M, Como J, Cotton B, et al. Damage control resuscitation in patients with severe traumatic hemorrhage: a practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2017;82:605–17.
Holcomb J, Wade C, Michalek J, Chisholm G, Zarzabal L, Schreiber M, et al. Increased plasma and platelet to red blood cell ratios improves outcome in 466 massively transfused civilian trauma patients. Ann Surg. 2008;248:447–58.
Holcomb J, Zarzabal L, Michalek J, Kozar R, Spinella P, Perkins J, et al. Increased platelet: RBC ratios are associated with improved survival after massive transfusion. J Trauma Acute Care Surg. 2011;71:318–28.
Pidcoke H, Aden J, Alejandra M, Borgman M, Spinella P, Dubick M, et al. Ten-year analysis of transfusion in Operation Iraqi Freedom and Operation Enduring Freedom: increased plasma and platelet use correlates with improved survival. J Trauma Acute Care Surg. 2012;73:445–52.
Holcomb J, del Junco D, Fox E, Wade C, Cohen M, Schreiber M, et al. The Prospective, Observational, Multicenter, Major Trauma Transfusion (PROMMTT) study: comparative effectiveness of a time-varying treatment with competing risks. JAMA Surg. 2013;148:127–36.
Spahn D, Bouillon B, Cerny V, Duranteau J, Filipescu D, Hunt B, et al. The European guideline on management of major bleeding and coagulopathy following trauma: fifth edition. Crit Care. 2019;23:98.
National Institute for Health and Care Excellence (NICE). Major Trauma: NICE guideline NG39. London: NICE; 2016.
American College of Surgeons. Advanced trauma life support (ATLS). 10th ed. Chicago: American College of Surgeons; 2018.
Advanced Life Support Group. Advanced paediatric life support: a practical approach to emergencies (APLS). 6th ed. London: BMJ Publishing Group; 2016.
Paterson-Brown S, Howell C. The MOET course manual. Managing obstetric emergencies and trauma. 3rd ed. Cambridge: Cambridge University Press; 2016.
Paxton J. Intraosseous vascular access: a review. Trauma. 2012;14:195–232.
Anson J. Vascular access in resuscitation: Is there a role for the intraosseous route? Anesthesiology. 2014;120:1015–31.
Petitpas F, Guenezan J, Vendeuvre T, Scepi M, Oriot D, Mimoz O. Use of intra-osseous access in adults: a systematic review. Crit Care. 2016;20:102.
Bjerkvig C, Fosse T, Apelseth T, Sivertsen J, Braathen H, Eliassen H, et al. Emergency sternal intraosseous access for warm fresh whole blood transfusion in Damage Control Resuscitation: 'Sternal intraosseous access in DCR'. J Trauma Acute Care Surg. 2018;84:S120–S124124.
Szarpak L, Ladny J, Dabrowski M, Ladny M, Smereka J, Ahuja S, et al. Comparison of 4 pediatric intraosseous access devices: a randomized simulation study. Pediatr Emerg Care. 2018. https://doi.org/10.1097/PEC.0000000000001587[Epub ahead of print].
Harris M, Balog R, Devries G. What is the evidence of utility for intraosseous blood transfusion in damage-control resuscitation? J Trauma Acute Care Surg. 2013;75:904–6.
Plewa M, King R, Fenn-Buderer N, Gretzinger K, Renuart D, Cruz R. Hematologic safety of intraosseous blood transfusion in a swine model of pediatric hemorrhagic hypovolemia. Acad Emerg Med. 1995;2:799–809.
Burgert J, Mozer J, Williams T, Gostnell J, Gegel B, Johnson S, et al. Effects of intraosseous transfusion of whole blood on hemolysis and transfusion time in a swine model of hemorrhagic shock: a pilot study. AANA J. 2014;82:198–202.
Bell M, Olshaker J, Brown C, McNamee G Jr, Fauver G. Intraosseous transfusion in an anesthetized swine model using 51Cr labeled autologous red blood cells. J Trauma Acute Care Surg. 1991;31:1487–9.
Lewis P, Wright C. Saving the critically injured trauma patient: a retrospective analysis of 1000 uses of intraosseous access. Emerg Med J. 2015;32:463–7.
Engels P, Erdogan M, Widder S, Butler M, Kureshi N, Martin K, et al. Use of intraosseous devices in trauma: a survey of trauma practitioners in Canada, Australia and New Zealand. Can J Surg. 2016;59:374–82.
Sherren P, Burns B. Prehospital blood transfusion: 5-year experience of an Australian helicopter emergency medical service. Crit Care. 2013;17:295.
Lyon R, Sausmarez E, McWhirter E, Wareham G, Nelson M, Matthies A, et al. Pre-hospital transfusion of packed red blood cells in 147 patients from a UK helicopter emergency medical service. Scand J Trauma Resusc Emerg Med. 2017;25:12.
Smith I, Crombie N, Bishop J, McLaughlin A, Naumann D, Herbert M, et al. RePHILL: protocol for a randomised controlled trial of pre-hospital blood product resuscitation for trauma. Transfus Med. 2018;28:346–56.
World Health Organization. Injuries and violence: the facts 2014. Geneva: World Health Organization; 2014.
Morley P, Atkins D, Billi J, Bossaert L, Callaway C, de Caen AR, et al. Part 3: evidence evaluation process: 2010 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation. 2010;81:S32–40.
Fenton P, Bali N, Sergeant I, Jeffrey S. A complication of the use of an intra-osseous needle. J R Army Med Corps. 2009;155:110–1.
Sarkar D, Philbeck T. The use of multiple intraosseous catheters in combat casualty resuscitation. Mil Med. 2009;174:106–8.
Nadler R, Gendler S, Chen J, Lending G, Abramovitch A, Glassberg E. The Israeli Defence Force experience with intraosseous access. Mil Med. 2014;179:1254–7.
Vassallo J, Horne S, Smith J. Intraosseous access in the military operational setting. J R Nav Med Serv. 2014;100:34–7.
Helm M, Haunstein B, Schlechtriemen T, Ruppert M, Lampl L, Gäβler M. EZ–IO(®) intraosseous device implementation in German helicopter emergency medical service. Resuscitation. 2015;88:43–7.
Savell S, Mora A, Perez C, Bebarta V, Maddry M. En route intraosseous access performed in the combat setting. Am J Disaster Med. 2016;11:225–31.
Malhotra R, Chua W, O’Neil G. Calf compartment syndrome associated with the use of an intra-osseous line in an adult patient: a case report. Malays Orthop J. 2016;10:49–51.
Chreiman K, Dumas R, Seamon M, Kim P, Reilly P, Kaplan L, et al. The intraosseous have it: a prospective observational study of vascular access success rates in patients in extremis using video review. J Trauma Acute Care Surg. 2018;84:558–6566.
Weiser G, Hoffmann Y, Galbraith R, Shavit I. Current advances in intraosseous infusion—a systematic review. Resuscitation. 2012;83:20–2.
Santos D, Carron P, Yersin B, Pasquier M. EZ–IO intraosseous device implementation in a pre-hospital emergency service: a prospective study and review of the literature. Resuscitation. 2013;84:440–5.
Hartholt K, van Lieshout E, Thies W, Patka P, Schipper I. Intraosseous devices: a randomized controlled trial comparing three intraosseous devices. Prehosp Emerg Care. 2010;14:6–13.
Frascone R, Jensen J, Kaye K, Salzman J. Consecutive field trials using two different intraosseous devices. Prehosp Emerg Care. 2007;11:164–71.
Leidel B, Kirchhoff C, Braunstein V, Bogner V, Biberthaler P, Kanz K. Comparison of two intraosseous access devices in adult patients under resuscitation in the emergency department: a prospective, randomized study. Resuscitation. 2010;81:994–9.
Sunde G, Heradstveit B, Vikenes B, Heltne J. Emergency intraosseous access in a helicopter emergency medical service: a retrospective study. Scand J Trauma Resusc Emerg Med. 2010;18:52.
Shavit I, Hoffmann Y, Galbraith R, Waisman Y. Comparison of two mechanical intraosseous infusion devices: a pilot, randomized crossover trial. Resuscitation. 2009;80:1029–33.
Luck R, Haines C, Mull C. Intraosseous access. J Emerg Med. 2010;34:468–75.
Hodgetts J, Johnston A, Kendrew J. Long-term follow-up of two patients with retained intraosseous sternal needles. J R Army Med Corps. 2017;163:221–2.
Dubick M, Holcomb J. A review of intraosseous vascular access: current status and military application. Mil Med. 2000;165:552.
Harris M. Re: saving the critically injured trauma patient. Emerg Med J. 2015;32:903.
Lallemand M, Moe D, McClellan J, Loughren M, Marko S, Eckert M, et al. No intravenous access, no problem: Intraosseous administration of tranexamic acid is as effective as intravenous in a porcine hemorrhage model. J Trauma Acute Care Surg. 2018;84:379–85.
Boysen S, Pang J, Mikler J, Knight C, Semple H, Caulkett N. Comparison of tranexamic acid plasma concentrations when administered via intraosseous and intravenous routes. Am J Emerg Med. 2017;35:227–33.
Bourne C, Cabelguenne D, David J, Rioufol C, Piriou V. Massive transfusion: analysis of practices according to available medical devices. Ann Fr Anesth Reanim. 2012;31:537–42.
Yentis S, Hirsch N. Anaesthesia and intensive care A–Z: an encyclopaedia of principles and practice. 4th ed. London: Churchill Livingston; 2009.
de Vogel J, Heydanus R, Mulders A, Smalbraak D, Papatsonis D, Gerritse B. Lifesaving intraosseous access in a patient with a massive obstetric hemorrhage. AJP Rep. 2011;1:119–22.
Chansa E, Hansen K, Gustafsson B. An intraosseous blood transfusion in a critically ill child. Afr J Emerg Med. 2014;4:83–5.
Burgert J. Intraosseous infusion of blood products and epinephrine in an adult patient in hemorrhagic shock. AANA J. 2009;77:359–63.
Weiser G, Poppa E, Katz Y, Bahouth H, Shavit I. Intraosseous blood transfusion in infants with traumatic hemorrhagic shock. Am J Emerg Med. 2013;31(640):e3–4.
Pasley J, Miller C, DuBose J, Shackelford S, Fang R, Boswell K, et al. Intraosseous infusion rates under high pressure: a cadaveric comparison of anatomic sites. J Trauma Acute Care Surg. 2015;78:295–9.
Hodge D, Fleisher G. Pediatric catheter flow rates. Am J Emerg Med. 1985;3:403–7.
Leidel B, Kirchhoff C, Bogner V, Braunstein V, Biberthaler P, Kanz K. Comparison of intraosseous versus central venous vascular access in adults under resuscitation in the emergency department with inaccessible peripheral veins. Resuscitation. 2012;83:40–5.
Joint United Kingdom (UK) Blood transfusion and tissue transplantation services professional advisory committee. Transfusion Handbook, https://www.transfusionguidelines.org/transfusion-handbook/7-effective-transfusion-in-surgery-and-critical-care/7-3-transfusion-management-of-major-haemorrhage. [Accessed 3 Sep 2018].
Sheils M, Ross M, Eatough N, Caputo N. Intraosseous access in trauma by air medical retrieval teams. Air Med J. 2014;33:161–4.
Tinmouth A, Fergusson D, Yee I, Hebert P. Clinical consequences of red cell storage in the critically ill. Transfusion. 2006;46:2014–27.
Author information
Authors and Affiliations
Contributions
JAT and HDD conceived the idea for the article. The literature was reviewed and analysed by JAT. The manuscript was drafted by JT and critically revised for intellectual content by ZP and HDD. JAT takes responsibility for the integrity of the data and the accuracy of its analysis.
Corresponding author
Ethics declarations
Conflict of interest
JAT, ZP and HDD declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Tyler, J.A., Perkins, Z. & De’Ath, H.D. Intraosseous access in the resuscitation of trauma patients: a literature review. Eur J Trauma Emerg Surg 47, 47–55 (2021). https://doi.org/10.1007/s00068-020-01327-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-020-01327-y