Abstract
Purpose
Only a few reports compare the mid- and long-term outcome of the minimally invasive deltoid split (MIDS) with the classic anterior deltopectoral (DP) approach for osteosynthesis in proximal humeral fractures. This study compared the mid-term functional and the radiological results in patients with proximal humeral fractures undergoing osteosynthesis with the proximal humeral internal locking system (PHILOS™).
Methods
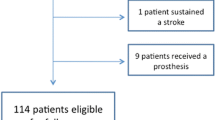
All patients undergoing osteosynthesis between 2008 and 2015 were clinically and radiologically examined with a minimal follow-up period of 1 year. Functional outcomes were analyzed using the DASH- and Constant Shoulder Scores (CSS). Radiological results were analyzed using a newly developed score.
Results
Thirty-nine patients underwent PHILOS™ osteosynthesis with the MIDS and twenty-three with the DP approach. Follow-up time was 41 months in the MIDS group and 62 months in the DP group, respectively. The median CSS was similar with 79 points in the MIDS group and 82 points in the DP group (p = 0.17). The MIDS group showed a significant lower power measurement in the CSS. In four-part fractures, a substantially lower CSS in absolute numbers in the MIDS group was detected. The median DASH score was 26.7 points in the MIDS group and 25.8 points in the DP group (p = 0.48). There was no difference in the radiological score. More patients with partial avascular necrosis (AVN) were found in the MIDS group, most with three- and four-part fractures. However, this was not statistically significant. Morbidity was similar between groups.
Conclusion
The results of the two surgical approaches are statistically comparable. Some differences such as a lower power measurement in the MIDS group, a higher partial AVN frequency and more plate removals are observed. In four-part fractures, the CSS was lower in the MIDS compared to the DP cohort. The MIDS technique might not be a solution for all fracture types, and the surgeon should be careful to analyze the morphology of the fracture before deciding upon the approach. Four-part fractures might be better treated with a DP approach.


Similar content being viewed by others
References
Lippuner K, Popp AW, Schwab P, Gitlin M, Schaufler T, Senn C, et al. Fracture hospitalizations between years 2000 and 2007 in Switzerland: a trend analysis. Osteoporos Int. 2011;22(9):2487–97.
Baron JA, Karagas M, Barrett J, Kniffin W, Malenka D, Mayor M, et al. Basic epidemiology of fractures of the upper and lower limb among Americans over 65 years of age. Epidemiology. 1996;7(6):612–8.
Kannus P, Palvanen M, Niemi S, Parkkari J, Jarvinen M, Vuori I. Osteoporotic fractures of the proximal humerus in elderly Finnish persons: sharp increase in 1970–1998 and alarming projections for the new millennium. Acta Orthopaed Scand. 2000;71(5):465–70.
Neer CS. Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am Vol. 1970;52(6):1077–89.
Neer CS. Displaced proximal humeral fractures. II. Treatment of three-part and four-part displacement. J Bone Joint Surg Am Vol. 1970;52(6):1090–103.
Habermeyer P. Die Humeruskopffraktur. Der Unfallchirurg. 1997;100:820–37.
Moonot P, Ashwood N, Hamlet M. Early results for treatment of three- and four-part fractures of the proximal humerus using the PHILOS plate system. J Bone Joint Surg Am Vol. 2007;89(9):1206–9.
Acklin YP, Jenni R, Walliser M, Sommer C. Minimal, Invasive. PHILOS((R))-plate osteosynthesis in proximal humeral fractures. Eur J Trauma Emerg Surg. 2009;35(1):35–9.
Lin T, Xiao B, Ma X, Fu D, Yang S. Minimally invasive plate osteosynthesis with a locking compression plate is superior to open reduction and internal fixation in the management of the proximal humerus fractures. BMC Musculoskelet Disord. 2014;15:206.
Liu K, Liu PC, Liu R, Wu X. Advantage of minimally invasive lateral approach relative to conventional deltopectoral approach for treatment of proximal humerus fractures. Med Sci Monit. 2015;21:496–504.
Hepp P, Theopold J, Voigt C, Engel T, Josten C, Lill H. The surgical approach for locking plate osteosynthesis of displaced proximal humeral fractures influences the functional outcome. J Shoulder Elbow Surg. 2008;17(1):21–8.
Wu CH, Ma CH, Yeh JJ, Yen CY, Yu SW, Tu YK. Locked plating for proximal humeral fractures: differences between the deltopectoral and deltoid-splitting approaches. J Trauma. 2011;71(5):1364–70.
Vijayvargiya M, Pathak A, Gaur S. Outcome analysis of locking plate fixation in proximal humerus fracture. J Clin Diagn Res. 2016;10(8):RC01–5.
Buecking B, Mohr J, Bockmann B, Zettl R, Ruchholtz S. Deltoid-split or deltopectoral approaches for the treatment of displaced proximal humeral fractures? Clin Orthop Relat Res. 2014;472(5):1576–85.
Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987(214):160–4.
Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med. 1996;29(6):602–8.
Ficat RP. Idiopathic bone necrosis of the femoral head. Early diagnosis and treatment. J Bone Joint Surg Br Vol. 1985;67(1):3–9.
Gardner MJ, Boraiah S, Helfet DL, Lorich DG. The anterolateral acromial approach for fractures of the proximal humerus. J Orthop Trauma. 2008;22(2):132–7.
Visser CP, Coene LN, Brand R, Tavy DL. Nerve lesions in proximal humeral fractures. J Shoulder Elbow Surg Am Shoulder Elbow Surg. 2001;10(5):421–7.
Visser CP, Tavy DL, Coene LN, Brand R. Electromyographic findings in shoulder dislocations and fractures of the proximal humerus: comparison with clinical neurological examination. Clin Neurol Neurosurg. 1999;101(2):86–91.
Roderer G, Erhardt J, Kuster M, Vegt P, Bahrs C, Kinzl L, et al. Second generation locked plating of proximal humerus fractures—a prospective multicentre observational study. Int Orthop. 2011;35(3):425–32.
Hertel R, Hempfing A, Stiehler M, Leunig M. Predictors of humeral head ischemia after intracapsular fracture of the proximal humerus. J Shoulder Elbow Surg Am Shoulder Elbow Surg. 2004;13(4):427–33.
Kruithof RN, Formijne Jonkers HA, van der Ven DJC, van Olden GDJ, Timmers TK. Functional and quality of life outcome after non-operatively managed proximal humeral fractues. J Orthop Traumatol. 2017;18(4):423–30.
Koljonen PA, Fang C, Lau TW, Leung F, Cheung NW. Minimally invasive plate osteosynthesis for proximal humeral fractures. J Orthop Surg. 2015;23(2):160–3.
Acknowledgements
The authors thank Ms. T. Glass for performing the statistical analyses, Ms. P. Heeb, Scientific Assistant, for her support in recruiting the patients and organizing the follow-up appointments, and Ms. C. Vines, MD, for the English language revision.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Joëlle Borer, Arby Babians, Jochen Schwarz, Silke Potthast, Marcel Jakob, Philipp Lenzlinger, and Urs Zingg declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Borer, J., Schwarz, J., Potthast, S. et al. Mid-term results of minimally invasive deltoid-split versus standard open deltopectoral approach for PHILOS™ (proximal humeral internal locking system) osteosynthesis in proximal humeral fractures. Eur J Trauma Emerg Surg 46, 825–834 (2020). https://doi.org/10.1007/s00068-019-01076-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-019-01076-7