Abstract
Background
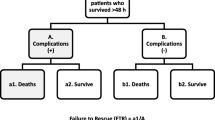
Trauma centers require reliable metrics to better compare the quality of care delivered. We compared mortality after a reported complication, termed failure to rescue (FTR), and FTR in the elderly (age >65 years) (FTRE) to determine which is a superior metric to assess quality of care delivered by trauma centers.
Methods
This was a retrospective review of the National Trauma Databank (NTDB) research data sets 2010 and 2011. Patients ≥16 years admitted to centers reporting ≥80% of AIS and/or ≥ 20% of comorbidities with > 200 subjects in the NTDB were selected. Centers were classified based on the rate of FTR and FTRE (<5 vs. 5–14 vs. ≥15%). The primary outcome was adjusted mortality for each group of trauma centers based on FTR and FTRE classifications.
Results
The overall mean ± SD FTR rate was 7.2 ± 5.2% and FTRE was 10.4 ± 7.9%. The adjusted odds ratio (AOR) for mortality was not different when centers with FTR <5% were compared to those with FTR of 5–14 or ≥15%. In contrast, a stepwise increase in FTRE predicted a significantly higher mortality when centers with FTRE 5% were compared to those with 5–14% (AOR: 1.05, p = 0.031) and ≥15% (AOR: 1.13, p < 0.001). Similarly, stepwise increase in FTRE predicted higher adjusted mortality for severely and critically injured patients, whereas FTR did not.
Conclusions and relevance
Higher FTRE predicts increased adjusted mortality better than FTR after trauma and should, therefore, be considered an important metric when comparing quality care delivered by trauma centers.

Similar content being viewed by others
References
American College of Surgeons. Resources for optimal care of the injured patient. Am Coll Surg. 2006;98.
Champion HR, Copes WS, Sacco WJ, et al. The major trauma outcome study: establishing national norms for trauma care. J Trauma. 1990;30(11):1356–65. http://www.ncbi.nlm.nih.gov/pubmed/2231804. Accessed 2 June 2014.
Hemmila MR, Nathens AB, Shafi S, et al. The trauma quality improvement program: pilot study and initial demonstration of feasibility. J Trauma. 2010;68(2):253–62.
Hashmi ZG, Schneider EB, Castillo R, et al. Benchmarking trauma centers on mortality alone does not reflect quality of care: implications for pay-for-performance. J Trauma Acute Care Surg. 2014;76(5):1184–91.
Demetriades D, Karaiskakis M, Velmahos G, et al. Effect on outcome of early intensive management of geriatric trauma patients. Br J Surg. 2002;89(10):1319–22.
Goodmanson NW, Rosengart MR, Barnato AE, Sperry JL, Peitzman AB, Marshall GT. Defining geriatric trauma: when does age make a difference? Surgery. 2012;152(4):668–74. (discussion 674–5).
Barmparas G, Martin M, Wiegmann DA, et al. Increased age predicts failure to rescue. Am Surg. 2016;82(11):1073–9. (7).
VanLare JM, Conway PH. Value-based purchasing–national programs to move from volume to value. N Engl J Med. 2012;367(4):292–5.
U.S. Census Bureau DIS. 2012 National Population Projections. http://www.census.gov/population/projections/data/national/2012.html. Accessed 20 Mar 2014.
Rhee P, Joseph B, Pandit V, et al. Increasing trauma deaths in the United States. Ann Surg. 2014;260(1):13–21.
WISQARS (Web-based Injury Statistics Query and Reporting System)|Injury Center|CDC. http://www.cdc.gov/injury/wisqars/. Accessed 15 June 2014.
Corso P, Finkelstein E, Miller T, Fiebelkorn I, Zaloshnja E. Incidence and lifetime costs of injuries in the United States. Inj Prev. 2006;12(4):212–8.
Velopulos CG, Enwerem NY, Obirieze A, et al. National cost of trauma care by payer status. J Surg Res. 2013;184(1):444–9.
Nathens AB, Cryer HG, Fildes J. The American college of surgeons trauma quality improvement program. Surg Clin North Am. 2012;92(2):441–54. x–xi.
Sharma S, de Mestral C, Hsiao M, et al. Benchmarking trauma center performance in traumatic brain injury: the limitations of mortality outcomes. J Trauma Acute Care Surg. 2013;74(3):890–4.
Hashmi ZG, Dimick JB, Efron DT, et al. Reliability adjustment: a necessity for trauma center ranking and benchmarking. J Trauma Acute Care Surg. 2013;75(1):166–72. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3989535&tool=pmcentrez&rendertype=abstract. Accessed 21 Dec 2014.
Shafi S, Rayan N, Barnes S, Fleming N, Gentilello LM, Ballard D. Moving from “optimal resources” to “optimal care” at trauma centers. J Trauma Acute Care Surg. 2012;72(4):870–7.
Silber JH, Rosenbaum PR. A spurious correlation between hospital mortality and complication rates: the importance of severity adjustment. Med Care. 1997;35(10 Suppl):OS77–OS92. http://www.ncbi.nlm.nih.gov/pubmed/9339779. Accessed 21 Mar 2014.
Ghaferi AA, Birkmeyer JD, Dimick JB. Variation in hospital mortality associated with inpatient surgery. N Engl J Med. 2009;361(14):1368–75.
Ghaferi AA, Birkmeyer JD, Dimick JB. Complications, failure to rescue, and mortality with major inpatient surgery in medicare patients. Ann Surg. 2009;250(6):1029–34. http://www.ncbi.nlm.nih.gov/pubmed/19953723. Accessed 21 Mar 2014.
Ghaferi AA, Osborne NH, Birkmeyer JD, Dimick JB. Hospital characteristics associated with failure to rescue from complications after pancreatectomy. J Am Coll Surg. 2010;211(3):325–30.
Ahmed EO, Butler R, Novick RJ. Failure-to-rescue rate as a measure of quality of care in a cardiac surgery recovery unit: a five-year study. Ann Thorac Surg. 2014;97(1):147–52.
Pasquali SK, He X, Jacobs JP, Jacobs ML, O’Brien SM, Gaynor JW. Evaluation of failure to rescue as a quality metric in pediatric heart surgery: an analysis of the STS Congenital Heart Surgery Database. Ann Thorac Surg. 2012;94(2):573–9 (discussion 579–80).
Glance LG, Dick AW, Meredith JW, Mukamel DB. Variation in hospital complication rates and failure-to-rescue for trauma patients. Ann Surg. 2011;253(4):811–6.
Taylor MD, Tracy JK, Meyer W, Pasquale M, Napolitano LM. Trauma in the elderly: intensive care unit resource use and outcome. J Trauma. 2002;53(3):407–14.
McKevitt EC, Calvert E, Ng A, et al. Geriatric trauma: resource use and patient outcomes. Can J Surg. 2003;46(3):211–5. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3211738&tool=pmcentrez&rendertype=abstract. Accessed 21 Dec 2014.
Haas B, Gomez D, Hemmila MR, Nathens AB. Prevention of complications and successful rescue of patients with serious complications: characteristics of high-performing trauma centers. J Trauma. 2011;70(3):575–82.
Asplund K, Gustafson Y, Jacobsson C, et al. Geriatric-based versus general wards for older acute medical patients: a randomized comparison of outcomes and use of resources. J Am Geriatr Soc. 2000;48(11):1381–8. http://www.ncbi.nlm.nih.gov/pubmed/11083312. Accessed 22 Dec 2014.
Landefeld CS, Palmer RM, Kresevic DM, Fortinsky RH, Kowal J. A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients. N Engl J Med. 1995;332(20):1338–44.
Lenartowicz M, Parkovnick M, McFarlan A, et al. An evaluation of a proactive geriatric trauma consultation service. Ann Surg. 2012;256(6):1098–101.
Bradburn E, Rogers FB, Krasne M, et al. High-risk geriatric protocol: improving mortality in the elderly. J Trauma Acute Care Surg. 2012;73(2):435–40.
Matsushima K, Schaefer EW, Won EJ, Armen SB, Indeck MC, Soybel DI. Positive and negative volume-outcome relationships in the geriatric trauma population. JAMA Surg. 2014;149(4):319–26.
Author contributions
Study conception and design: GB, MD; MM, MD; BLG, MD; and EJL, MD. Acquisition of data: GB, MD; AK, MD; MH, BS; and EJL, MD. Analysis and interpretation of data: GB, MD; MM, MD; and EJL, MD. Literature review: GB, MD; MM, MD; and EJL, MD. Drafting of manuscript: GB, MD; MM, MD; BLG, MD; and EJL, MD. Critical revision: DAW, PhD; KRC, PhD; BLG, MD; and EJL, MD.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to report and have received no financial support in relation to this manuscript.
Rights and permissions
About this article
Cite this article
Barmparas, G., Ley, E.J., Martin, M.J. et al. Failure to rescue the elderly: a superior quality metric for trauma centers. Eur J Trauma Emerg Surg 44, 377–384 (2018). https://doi.org/10.1007/s00068-017-0782-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-017-0782-x