Abstract
Purpose
The treatment mode in acute vertebrobasilar occlusion (VBO) remains uncertain. We analyzed efficacy and safety of intravenous glycoprotein IIb/IIIa inhibitor (IV GPI) plus subsequent intra-arterial thrombolysis with or without additional endovascular mechanical therapy (percutaneous transluminal angioplasty/stenting or thrombus aspiration) and sought treatment factors that predict good clinical outcome.
Methods
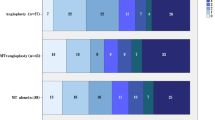
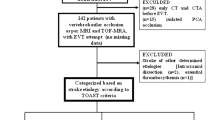
We retrospectively analyzed 120 cases of patients with angiographically proven acute VBO. Multivariate logistic regression was used to identify independent predictors for clinical outcome and included level of consciousness, age, sex, time to angiography, GPI agent, admission mode, occlusion type, recanalization success, and endovascular treatment mode. Clinical follow-up was dichotomized in no to moderate disability (modified Rankin scale (mRS) 0–3) vs. severe disability or death (mRS 4–6).
Results
Median National Institutes of Health stroke scale (NIHSS) score on admission was 32, and mean NIHSS score was 24. A total of 49 patients (41 %) developed no to moderate disability (mRS 0–3), and 39 patients (33 %) died. Thrombolysis in myocardial infarction 2/3 recanalization success was achieved in 97 patients (80.8 %). Symptomatic intracerebral hemorrhages occurred in 11 patients (9 %). Mild impairment of consciousness (p < 0.001) and embolic occlusion type (p = 0.01) were significant predictors of favorable outcome. Clinical outcome in recanalized patients was better, but not statistically significant (p = 0.055).
Conclusions
Our results indicate that combined therapy with IV GPI and subsequent endovascular therapy may be a valid treatment strategy in acute VBO. With this treatment approach, a preserved vigilance before treatment and an embolic occlusion type are associated with no to moderate disability.

Similar content being viewed by others
Abbreviations
- VBO:
-
Vertebrobasilar occlusion
- IV GPI:
-
Intravenous glycoprotein IIb/IIIa inhibitor
- TIMI:
-
Thrombolysis in myocardial infarction
- PTA:
-
Percutaneous transluminal angioplasty
References
Hacke W, Zeumer H, Ferbert A, Bruckmann H, del Zoppo GJ. Intra-arterial thrombolytic therapy improves outcome in patients with acute vertebrobasilar occlusive disease. Stroke. 1988;19(10):1216–22.
Becker R. Dynamics of coronary thrombolysis and reocclusion. Clin Cardiol. 1997;11(Suppl. 3):III2–5.
Nagel S, Schellinger PD, Hartmann M, Juettler E, Huttner HB, Ringleb P, Schwab S, Köhrmann M. Therapy of acute basilar artery occlusion: intraarterial thrombolysis alone vs bridging therapy. Stroke. 2009;40(1):140–6. doi:10.1161/STROKEAHA.108.526566.
Eckert B, Koch C, Thomalla G, Kucinski T, Grzyska U, Roether J, Alfke K, Jansen O, Zeumer H. Aggressive therapy with intravenous abciximab and intra-arterial rtPA and additional PTA/stenting improves clinical outcome in acute vertebrobasilar occlusion: combined local fibrinolysis and intravenous abciximab in acute vertebrobasilar stroke treatment (FAST): results of a multicenter study. Stroke. 2005;36(6):1160–5. doi:10.1161/01.STR.0000165918.80812.1e.
Barlinn K, Becker U, Puetz V, Dzialowski I, Kunz A, Kepplinger J, von Kummer R, Gahn G. Combined treatment with intravenous abciximab and intraarterial tPA yields high recanalization rate in patients with acute basilar artery occlusion. J Neuroimaging. 2012;22(2):167–71. doi:10.1111/j.1552-6569.2011.00584.x.
Penumbra Pivotal Stroke Trial I. The penumbra pivotal stroke trial: safety and effectiveness of a new generation of mechanical devices for clot removal in intracranial large vessel occlusive disease. Stroke. 2009;40(8):2761–8. doi:10.1161/STROKEAHA.108.544957.
Schonewille WJ, Wijman CA, Michel P, Rueckert CM, Weimar C, Mattle HP, Engelter ST, Tanne D, Muir KW, Molina CA, Thijs V, Audebert H, Pfefferkorn T, Szabo K, Lindsberg PJ, de Freitas G, Kappelle LJ, Algra A; BASICS study group. Treatment and outcomes of acute basilar artery occlusion in the Basilar Artery International Cooperation Study (BASICS): a prospective registry study. Lancet. 2009;8(8):724–30. doi:10.1016/S1474-4422(09)70173-5.
Jauch EC, Saver JL, Adams HP, Jr., Bruno A, Connors JJ, Demaerschalk BM, Khatri P, McMullan PW Jr, Qureshi AI, Rosenfield K, Scott PA, Summers DR, Wang DZ, Wintermark M, Yonas H; American Heart Association Stroke Council; Council on Cardiovascular Nursing; Council on Peripheral Vascular Disease; Council on Clinical Cardiology. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(3):870–947. doi:10.1161/STR.0b013e318284056a.
Adams HP, Jr., Effron MB, Torner J, Davalos A, Frayne J, Teal P, Leclerc J, Oemar B, Padgett L, Barnathan ES, Hacke W; AbESTT-II Investigators. Emergency administration of abciximab for treatment of patients with acute ischemic stroke: results of an international phase III trial: Abciximab in Emergency Treatment of Stroke Trial (AbESTT-II). Stroke. 2008;39(1):87–99. doi:10.1161/STROKEAHA.106.476648.
Siebler M, Hennerici MG, Schneider D, von Reutern GM, Seitz RJ, Röther J, Witte OW, Hamann G, Junghans U, Villringer A, Fiebach JB. Safety of Tirofiban in acute Ischemic Stroke: the SaTIS trial. Stroke. 2011;42(9):2388–92. doi:10.1161/STROKEAHA.110.599662.
Pancioli AM, Adeoye O, Schmit PA, Khoury J, Levine SR, Tomsick TA, Sucharew H, Brooks CE, Crocco TJ, Gutmann L, Hemmen TM, Kasner SE, Kleindorfer D, Knight WA, Martini S, McKinney JS, Meurer WJ, Meyer BC, Schneider A, Scott PA, Starkman S, Warach S, Broderick JP; CLEAR-ER Investigators. Combined approach to lysis utilizing eptifibatide and recombinant tissue plasminogen activator in acute ischemic stroke-enhanced regimen stroke trial. Stroke. 2013;44(9):2381–7. doi:10.1161/STROKEAHA.113.001059.
Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med. 1995;333(24):1581–7. doi:10.1056/NEJM199512143332401.
Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, Larrue V, Lees KR, Medeghri Z, Machnig T, Schneider D, von Kummer R, Wahlgren N, Toni D; ECASS Investigators. Thrombolysis with alteplase 3–4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359(13):1317–29. doi:10.1056/NEJMoa0804656.
Pfefferkorn T, Holtmannspotter M, Schmidt C, Bender A, Pfister HW, Straube A, Mayer TE, Brückmann H, Dichgans M, Fesl G. Drip, ship, and retrieve: cooperative recanalization therapy in acute basilar artery occlusion. Stroke. 2010;41(4):722–6. doi:10.1161/STROKEAHA.109.567552.
Vergouwen MD, Algra A, Pfefferkorn T, Weimar C, Rueckert CM, Thijs V, Kappelle LJ, Schonewille WJ; Basilar Artery International Cooperation Study (BASICS) Study Group. Time is brain(stem) in basilar artery occlusion. Stroke. 2012;43(11):3003–6. doi:10.1161/STROKEAHA.112.666867.
Arnold M, Nedeltchev K, Schroth G, Baumgartner RW, Remonda L, Loher TJ, Stepper F, Sturzenegger M, Schuknecht B, Mattle HP. Clinical and radiological predictors of recanalisation and outcome of 40 patients with acute basilar artery occlusion treated with intra-arterial thrombolysis. J Neurol Neurosurg Psychiatry. 2004;75(6):857–62.
Lindsberg PJ, Mattle HP. Therapy of basilar artery occlusion: a systematic analysis comparing intra-arterial and intravenous thrombolysis. Stroke. 2006;37(3):922–8. doi:10.1161/01.STR.0000202582.29510.6b.
Fesl G, Holtmannspoetter M, Patzig M, Mayer TE, Pfefferkorn T, Brueckmann H, Schulte-Altedorneburg G. Mechanical thrombectomy in basilar artery thrombosis: technical advances and safety in a 10-year experience. Cardiovasc Intervent Radiol. 2014;37:355–61. doi:10.1007/s00270-013-0827-4.
Espinosa de Rueda M, Parrilla G, Zamarro J, Garcia-Villalba B, Hernandez F, Moreno A. Treatment of acute vertebrobasilar occlusion using thrombectomy with stent retrievers: initial experience with 18 patients. AJNR Am J Neuroradiol. 2013;34(5):1044–8. doi:10.3174/ajnr.A3329.
Acknowledgments
We acknowledge the efforts of Dr. Jan-Hendrik Buhk in kindly reviewing the manuscript and providing some very valuable suggestions enabling us to improve on the quality of the manuscript.
Sources of Funding
None.
Disclosures
J. Fiehler consults for Company Microvention, Stryker, Codman and is a speaker for Covidien.
Conflict of Interest
The authors declare that there are no actual or potential conflicts of interest in relation to this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ernst, M., Butscheid, F., Fiehler, J. et al. Glycoprotein IIb/IIIa Inhibitor Bridging and Subsequent Endovascular Therapy in Vertebrobasilar Occlusion in 120 Patients. Clin Neuroradiol 26, 169–175 (2016). https://doi.org/10.1007/s00062-014-0341-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00062-014-0341-3