Abstract
Epidemiological studies have shown that inflammation plays a critical role in the development and progression of various chronic diseases, including cancers, neurological diseases, hepatic fibrosis, diabetic retinopathy, and vascular diseases. Decursin and decursinol angelate (DA) are pyranocoumarin compounds obtained from the roots of Angelica gigas. Several studies have described the anti-inflammatory effects of decursin and DA. Decursin and DA have shown potential anti-inflammatory activity by modulating growth factors such as vascular endothelial growth factor, transcription factors such as signal transducer and activator of transcription 3 and nuclear factor kappa-light-chain-enhancer of activated B cells, cellular enzymes including matrix metalloproteinases cyclooxygenase, and protein kinases such as extracellular receptor kinase, phosphatidylinositol-3-kinase, and protein kinase C. These compounds have the ability to induce apoptosis by activating pro-apoptotic proteins and the caspase cascade, and reduced the expression of anti-apoptotic proteins such as B-cell lymphoma 2 and B-cell lymphoma-extra-large. Interaction with multiple molecular targets and cytotoxic effects, these two compounds are favorable candidates for treating various chronic inflammatory diseases such as cancers (prostate, breast, leukemia, cervical, and myeloma), rheumatoid arthritis, diabetic retinopathy, hepatic fibrosis, osteoclastogenesis, allergy, and Alzheimer’s disease. We have summarized the preliminary studies regarding the biological effects of decursin and DA. In this review, we will also highlight the functions of coumarin compounds that can be translated to a clinical practice for the treatment and prevention of various inflammatory ailments.


Similar content being viewed by others
References
Atanasov AG, Waltenberger B, Pferschy-Wenzig EM, et al. Discovery and resupply of pharmacologically active plant-derived natural products: a review. Biotechnol Adv. 2015;33:1582–614.
Choi KO, Lee I, Paik SY, Kim DE, Lim JD, Kang WS, Ko S. Ultrafine Angelica gigas powder normalizes ovarian hormone levels and has antiosteoporosis properties in ovariectomized rats: particle size effect. J Med Food. 2012;15:863–72.
Yim D, Singh RP, Agarwal C, Lee S, Chi H, Agarwal R. A novel anticancer agent, decursin, induces G1 arrest and apoptosis in human prostate carcinoma cells. Cancer Res. 2005;65:1035–44.
Kim WJ, Lee MY, Kim JH, Sukb K, Lee WH. Decursinol angelate blocks transmigration and inflammatory activation of cancer cells through inhibition of PI3K, ERK and NF-kB activation. Cancer Lett. 2010;296:35–42.
Jung SY, Choi JH, Kwon SM, Masuda H, Asahara T, Lee YM. Decursin inhibits vasculogenesis in early tumor progression by suppression of endothelial progenitor cell differentiation and function. J Cell Biochem. 2012;113:1478–87.
Jiang C, Guo J, Wang Z, Xiao B, Lee HJ, Lee EO, Lu J. Decursin and decursinol angelate inhibit estrogen-stimulated and estrogen-independent growth and survival of breast cancer cells. Breast Cancer Res. 2007;9:1.
Kim JH, Kim JH, Lee YM, Ahn EM, Kim KW, Yu YS. Decursin Inhibits VEGF-mediated inner blood—retinal barrier breakdown by suppression of VEGFR-2 activation. J Cereb Blood Flow Metab. 2009;29:1559–67.
Son SH, Kim MJ, Chung WY, Son JA, Kim YS, Kim YC, Park KK. Decursin and decursinol inhibit VEGF-induced angiogenesis by blocking the activation of extracellular signal-regulated kinase and c-Jun N-terminal kinase. Cancer Lett. 2009;280:86–92.
Lee B, Wu Z, Sung SH, Lee T, Song KS, Lee MY, Liu KH. Potential of decursin to inhibit the human cytochrome P450 2J2 isoform. Food Chem Toxicol. 2014;70:94–9.
Yim NH, Lee JH, Cho WK, Yang MC, Kwak DH, Ma JY. Decursin and decursinol angelate from Angelica gigas Nakai induce apoptosis via induction of TRAIL expression on cervical cancer cells. Eur J Integr Med. 2011;3:299–307.
Choi YJ, Kim DH, Kim SJ, Kim J, Jeong SI, Chung CH, Kim SY. Decursin attenuates hepatic fibrogenesis through interrupting TGF-beta-mediated NAD (P) H oxidase activation and Smad signaling in vivo and in vitro. Life Sci. 2014;108:94–103.
Zitvogel L, Pietrocola F, Kroemer G. Nutrition, inflammation and cancer. Nat Immunol. 2017;18:843–50.
Younis T, Haché KD, Rayson D, Dewar R, Gray S, Barnes PJ. Survivin and COX-2 expression in male breast carcinoma. Breast. 2009;18:228–32.
Arunasree KM, Roy KR, Anilkumar K, Aparna A, Reddy GV, Reddanna P. Imatinib-resistant K562 cells are more sensitive to celecoxib,A selective COX-2 inhibitor. Role of COX-2 and MDR-1. Leuk Res. 2008;32:855–64.
Ahn Q, Jeong SJ, Lee HJ, Kwon HY, Han I, Kim HS, Zhu S. Inhibition of cyclooxygenase-2-dependent survivin mediates decursin-induced apoptosis in human KBM-5 myeloid leukemia cells. Cancer Lett. 2010;298:212–21.
Shin S, Joo SS, Park D, Jeon JH, Kim TK, Kim JS, Park SK, Hwang BY, Kim YB. Ethanol extract of Angelica gigas inhibits croton oil-induced inflammation by suppressing the cyclooxygenase—prostaglandin pathway. J Vet Sci. 2010;11:43–50.
Yoo HH, Lee MW, Kim YC, Yun CH, Kim DH. Mechanism-based inactivation of cytochrome P450 2A6 by decursinol angelate isolated from Angelica gigas. Drug Metab Dispos. 2007;35:1759–65.
Satarug S, Ujjin P, Vanavanitkun Y, Nishijo M, Baker JR, Moore MR. Effects of cigarette smoking and exposure to cadmium and lead on phenotypic variability of hepatic CYP2A6 and renal function biomarkers in men. Toxicology. 2004; 204:161–73.
Enayetallah AE, French RA, Thibodeau MS, Grant DF. Distribution of soluble epoxide hydrolase and of cytochrome P450 2C8, 2C9, and 2J2 in human tissues. J Histochem Cytochem.2004; 52:447–54.
Wu S, Moomaw CR, Tomer KB, Falck JR, Zeldin DC. Molecular cloning and expression of CYP2J2, a human cytochrome P450 arachidonic acid epoxygenase highly expressed in heart. J Biol Chem. 1996;271:3460–68.
Chen C, Wei X, Rao X, Wu J, Yang S, Chen F, Wang DW. Cytochrome P450 2J2 is highly expressed in hematologic malignant diseases and promotes tumor cell growth. J Pharmacol Exp Ther. 2011;336:344–55.
Jiang JG, Chen CL, Card JW, Yang S, Chen JX, Fu XN, Ning YG, Xiao X, Zeldin DC, Wang DW. Cytochrome P450 2J2 promotes the neoplastic phenotype of carcinoma cells and is up-regulated in human tumors. Cancer Res. 2005;65:4707–15.
Lamalice L, Houle F, Jourdan G, Huot J. Phosphorylation of tyrosine 1214 on VEGFR2 is required for VEGF-induced activation of Cdc42 upstream of SAPK2/p38. Oncogene. 2004;23:434–45.
Jung MH, Lee SH, Ahn EM, Lee YM. Decursin and decursinol angelate inhibit VEGF-induced angiogenesis via suppression of the VEGFR-2-signaling pathway. Carcinogenesis. 2009;30:655–61.
Yao JS, Chen Y, Zhai W, Xu K, Young WL, Yang GY. Minocycline exerts multiple inhibitory effects on vascular endothelial growth factor-induced smooth muscle cell migration the role of ERK1/2, PI3K, and matrix metalloproteinases. Circ Res. 2004;95:364–71.
Chen CH, Chang LT, Tung WC, et al. “Levels and values of circulating endothelial progenitor cells, soluble angiogenic factors, and mononuclear cell apoptosis in liver cirrhosis patients. J Biomed Sci. 2012;19:66–77.
Bank S, Andersen PS, Burisch J, et al. polymorphisms in the toll-like receptor and the il-23/il-17 pathways were associated with susceptibility to inflammatory bowel disease in a danish cohort. Plos One. 2015;10:e0145302.
Pant S, Deshmukh A, Gurumurthy GS, Pothineni NV, Watts TE, Romeo F, Mehta JL. Inflammation and atherosclerosis–revisited. J Cardiovasc Pharmacol Ther. 2014;19:170–8.
Seki E, Schwabe RF. Hepatic inflammation and fibrosis: functional links and key pathways. Hepatology. 2015;61:1066–79.
Shehzad A, Islam SU, Ahn EM, Lee YM, Lee YS. Decursinol angelate inhibits PGE2-induced survival of the human leukemia HL-60 cell line via regulation of the EP2 receptor and NFκB pathway. Cancer Biol Ther. 2016;17:985–93.
Walter S, Letiembre M, Liu Y, Heine H, Penke B, Hao W, Bode B, Manietta N, Walter J, Schulz-Schuffer W, Fassbender K. Role of the toll-like receptor 4 in neuroinflammation in Alzheimer’s disease. Cell Physiol Biochem. 2007; 20:947–56.
Marchev AS, Dimitrova PA, Burns AJ, Kostov RV, Dinkova-Kostova AT, Georgiev MI. Oxidative stress and chronic inflammation in osteoarthritis: can NRF2 counteract these partners in crime? Ann N Y Acad Sci. 2017. https://doi.org/10.1111/nyas.13407.
Jiang C, Lee HJ, Li GX, Guo J, Malewicz B, Zhao Y, Kim SH. Potent antiandrogen and androgen receptor activities of an Angelica gigas-containing herbal formulation: identification of decursin as a novel and active compound with implications for prevention and treatment of prostate cancer. Cancer Res. 2006;66:453–63.
Kim JH, Jeong JH, Jeon ST, Kim H, Ock J, Suk K, Lee WH. Decursin inhibits induction of inflammatory mediators by blocking nuclear factor-κB activation in macrophages. Mol pharmacol. 2006;69:1783–90.
Siegel RL, Miller KD, Jemal A. Cancer Statistics. CA Cancer J Clin. 2017;67:7–30.
Kim JM, Noh EM, Kim MS, Hwang JK, Hwang HY, Ryu DG, Kim HJ, Yu HN, You YO, Kim JS, Youn HJ, Kwon KB, Jung SH, Lee YR. Decursin prevents TPA-induced invasion through suppression of PKCα/p38/NF-κB-dependent MMP-9 expression in MCF-7 human breast carcinoma cells. Int J Oncol. 2014;44:1607–13.
Choi SR, Lee JH, Kim JY, Park KW, Jeong IY, Shim KH, Seo KI. Decursin from Angelicagigas Nakai induces apoptosis in RC-58T/h/SA# 4 primary human prostate cancer cells via a mitochondria-related caspase pathway. Food Chem Toxicol. 2011;49:2517–23.
Zhang J, Wang L, Zhang Y, Li L, Tang S, et al. Chemopreventive effect of Korean Angelica root extract on TRAMP carcinogenesis and integrative “omic” profiling of affected neuroendocrine carcinomas. Mol Carcinog. 2015;54:1567–83.
Lee HJ, Lee EO, Lee JH, Lee KS, Kim KH, et al. In vivo anti-cancer activity of Korean Angelica gigas and its major pyranocoumarin decursin. Am J Chin Med. 2009;37:127–42.
Nilsson S, Gustafsson J-Å. Biological role of estrogen and estrogen receptors. Crit Rev Biochem Mol Biol. 2002;37:1–28.
de Azevedo CRAS, Thuler LCS, de Mello MJG, de Oliveira Lima JT, da Fonte ALF, Fontão DFS, Carneiro VCG, Chang TMC, Ferreira CG. Phase II trial of neoadjuvant chemotherapy followed by chemoradiation in locally advanced cervical cancer. Gynecol Oncol. 2017;8258:31023–5.
Hosseini A, Ghorbani A. Cancer therapy with phytochemicals.Evidence from clinical studies. Avicenna J Phytomed. 2015;5:84–97.
Maduro JH, Noordhuis MG, ten Hoor KA, Pras E, Arts HJ, Eijsink JJ, Hollema H, Mom CH, de Jong S, de Vries EG, de Bock GH, van der Zee AG. The prognostic value of TRAIL and its death receptors in cervical cancer. Int J Radiat Oncol Biol Phys. 2009;75:203–11.
Hideshima T, Mitsiades C, Tonon G, Richardson PG, Anderson KC. Understanding multiple myeloma pathogenesis in the bone marrow to identify new therapeutic targets. Nat Rev Cancer. 2007;7:585–98.
Ahn KS, Sethi G, Sung B, Goel A, Ralhan R, Aggarwal BB. Guggulsterone, a farnesoid X receptor antagonist, inhibits constitutive and inducible STAT3 activation through induction of a protein tyrosine phosphatase SHP-1. Cancer Res. 2008;68:4406–15.
Kim HJ, Kim SM, Park KR, Jang HJ, Na YS, Ahn KS, Ahn KS. Decursin chemosensitizes human multiple myeloma cells through inhibition of STAT3 signaling pathway. Cancer Lett. 2011;301:29–37.
Jang J, Jeong SJ, Kwon HY, Jung JH, Sohn EJ, Lee HJ, Kim JH, Kim SH, Kim JH, Kim SH. Decursin and doxorubicin are in synergy for the induction of apoptosis via stat3 and/or mtor pathways in human multiple myeloma cells. Evid Based Complement Alternat Med. 2013; 2013: 506324.
Kim HH, Bang SS, Choi JS, Han H, Kim IH. Involvement of PKC and ROS in the cytotoxic mechanism of anti-leukemic decursin and its derivatives and their structure–activity relationship in human K562 erythroleukemia and U937 myeloleukemia cells. Cancer Lett. 2005;223:191–201.
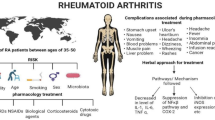
Chaudhari K, Rizvi S, Syed BA. Rheumatoid arthritis: current and future trends. Nat Rev Drug Discov. 2016;15:305–6.
Giannelli G, Erriquez R, Iannone F, Marinosci F, Lapadula G, Antonaci S. MMP-2, MMP-9, TIMP-1 and TIMP-2 levels in patients with rheumatoid arthritis and psoriatic arthritis. Clin Exp Rheumatol. 2004;22:335–8.
Manolagas SC. Birth and death of bone cells: basic regulatory mechanisms and implications for the pathogenesis and treatment of osteoporosis 1. Endocr Rev. 2000;21:115–37.
Takayanagi H, Kim S, Koga T, Nishina H, Isshiki M, Yoshida H, Wagner EF. Induction and activation of the transcription factor NFATc1 (NFAT2) integrate RANKL signaling in terminal differentiation of osteoclasts. Dev Cell. 2002;3:889–901.
Takayanagi H. Osteoimmunology, shared mechanisms and crosstalk between the immune and bone systems. Nat Rev Immunology. 2007;7:292–304.
Yagi M, Miyamoto T, Sawatani Y, Iwamoto K, Hosogane N, Fujita N, Oike Y. DC-STAMP is essential for cell–cell fusion in osteoclasts and foreign body giant cells. J Exp Med. 2005;202:345–51.
Yagi M, Miyamoto T, Toyama Y, Suda T. Role of DC-STAMP in cellular fusion of osteoclasts and macrophage giant cells. J Bone Miner Metab. 2006;24:355–58.
Mensah KA, Ritchlin CT, Schwarz EM. RANKL induces heterogeneous DC-STAMPlo and DC-STAMPhi osteoclast precursors of which the DC-STAMPlo precursors are the master fusogens. J Cell Physiol. 2010;223:76–83.
Hood JD, Cheresh DA. Role of integrins in cell invasion and migration. Nat Rev Cancer. 2002;2:91–100.
Kim KJ, Yeon JT, Choi SW, Moon SH, Ryu BJ, Yu R, Son YJ. Decursin inhibits osteoclastogenesis by downregulating NFATc1 and blocking fusion of pre-osteoclasts. Bone. 2015;81:208–16.
Wang X, Zheng T, Kang JH, Li H, Cho H, Jeon R, Ryu JH, Yim M. Decursin from Angelica gigas suppresses RANKL-induced osteoclast formation and bone loss. Eur J Pharmacol. 2016;774:34–42.
Gariano RF, Gardner TW. Retinal angiogenesis in development and disease. Nature. 2004;438:960–66.
Simó R, Hernández C. Intravitreous anti-VEGF for diabetic retinopathy. Hopes and fears for a new therapeutic strategy. Diabetologia. 2008;51:1574–80.
Qaum T, Xu Q, Joussen AM, Clemens MW, Qin W, Miyamoto K, Adamis AP. VEGF-initiated blood–retinal barrier breakdown in early diabetes. Inves ophthalmol vis sci. 2001;42:2408–13.
Yang Y, Yang K, Li Y, Li X, Sun Q, Meng H, Zhang Y. Decursin inhibited proliferation and angiogenesis of endothelial cells to suppress diabetic retinopathy via VEGFR2. Mol Cell Endocrinol. 2013;378:46–52.
Ui-Jin B, Mi-Ra O, Tae-Sung J, Soo-Wan C, Byung-Hyun P. Decursin and decursinol angelate-rich Angelica gigas Nakai extract suppresses de novo lipogenesis and alleviates nonalcoholic fatty liver disease and dyslipidemia in mice fed a high fat diet. J Funct Foods. 2017;31:208–16.
Friedman SL. Hepatic stellate cells, protean, multifunctional, and enigmatic cells of the liver. Physiol Rev. 2008;88:125–72.
Leask A, Abraham DJ. TGF-β signaling and the fibrotic response. FASEB J. 2004;18:816–27.
Crosas-Molist E, Fabregat I. Role of NADPH oxidases in the redox biology of liver fibrosis. Redox Biol. 2015;6:106–11.
Bedard K, Krause KH. The NOX family of ROS-generating NADPH oxidases: physiology and pathophysiology. Physiol Rev. 2007;87:245–313.
Cui W, Matsuno K, Iwata K, Ibi M, Matsumoto M, Zhang J, Yabe-Nishimura C. NOX1/nicotinamide adenine dinucleotide phosphate, reduced form (NADPH) oxidase promotes proliferation of stellate cells and aggravates liver fibrosis induced by bile duct ligation. Hepatology. 2011;54:949–58.
Jiang JX, Chen X, Serizawa N, Szyndralewiez C, Page P, Schröder K, Török NJ. Liver fibrosis and hepatocyte apoptosis are attenuated by GKT137831: a novel NOX4/NOX1 inhibitor in vivo. Free Radic Biol Med. 2012;53:289–96.
Feng XH, Derynck R. Specificity and versatility in TGF-β signaling through Smads. Annu Rev Cell Dev Biol. 2005;21:659–93.
Peiser M, Tralau T, Heidler J, et al. Allergic contact dermatitis: epidemiology, molecular mechanisms, in vitro methods and regulatory aspects. Cell Mol Life Sci. 2012;69:763–81.
Joo SS1, Park D, Shin S, Jeon JH, Kim TK, Choi YJ, Lee SH, Kim JS, Park SK, Hwang BY, Lee DI, Kim YB. Anti-allergic effects and mechanisms of action of the ethanolic extract of Angelica gigas in dinitrofluorobenzene-induced inflammation models. Environ Toxicol Pharmacol. 2010;30:127–33.
Shin S, Jeon JH, Park D, Jang JY, Joo SS, Hwang BY, Choe SY, Kim YB. Anti-inflammatory effects of an ethanol extract of Angelica gigas in a Carrageenan-air pouch inflammation model. Exp Anim. 2009;58:431–6.
Bonda DJ et al. Oxidative stress in Alzheimer disease: a possibility for prevention. Neuropharmacology. 2010;59:290–4.
Chauhan V, Chauhan A. Oxidative stress in Alzheimer’s disease. Pathophysiology. 2006;13:195–208.
Bhardwaj M, Deshmukh R, Kaundal M, Krishna Reddy BV. Pharmacological induction of hemeoxygenase-1 activity attenuates intracerebroventricular streptozotocin induced neurocognitive deficit and oxidative stress in rats. Eur J Pharmacol. 2016;772:43–50.
Kang SY, Kim YC. Decursinol and decursin protect primary cultured rat cortical cells from glutamate-induced neurotoxicity. J Pharm Pharmacol. 2007;59:863–70.
Li L, Du J, Zou L, Xia H, Wu T, Kim Y, Lee Y. The neuroprotective effects of decursin isolated from Angelica gigas nakai against amyloid β-protein-induced apoptosis in PC 12 cells via a mitochondria-related caspase pathway. Neurochem Res. 2015;40:1555–62.
Li L, Du JK, Zou LY, Wu T, Lee YW, Kim YH. Decursin isolated from Angelica gigas Nakai rescues PC12 cells from amyloid-protein-induced neurotoxicity through Nrf2-mediated upregulation of heme oxygenase-1: potential roles of MAPK. Evid Based Complement Alternat Med. 2013; 2013:467245.
Kim KM, Lee YJ, Hong YG, Kang JS. Oral acute and subacute toxicity studies of decursin and decursinol angelate of Angelica gigas Nakai. Mol Cell Toxicol. 2009;5:153–9.
Zhang J, Li L, Hale TW, Chee W, Xing C, Jiang C, Lü J. Single oral dose pharmacokinetics of decursin and decursinol angelate in healthy adult men and women. PloS One. 2015;10:e0114992.
Acknowledgements
This research was supported by the Basic Science Research Program of the NRF funded by the Ministry of Science, ICT, and Future Planning (NRF-2016R1A2B4012677).
Author information
Authors and Affiliations
Corresponding author
Additional information
Responsible Editor: John Di Battista.
Rights and permissions
About this article
Cite this article
Shehzad, A., Parveen, S., Qureshi, M. et al. Decursin and decursinol angelate: molecular mechanism and therapeutic potential in inflammatory diseases. Inflamm. Res. 67, 209–218 (2018). https://doi.org/10.1007/s00011-017-1114-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00011-017-1114-7