Abstract
Objective
We aimed to investigate the regulation and contribution of vascular endothelial growth factor (VEGF) and sFlt-1(1–3) to human monocytic THP-1 migration.
Materials and methods
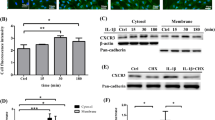
Ad-sFlt-1/FLAG, a recombinant adenovirus carrying the human sFlt-1(1–3) (the first three extracellular domains of FLT-1, the hVEGF receptor-1) gene, was constructed. L929 cells were infected with Ad-sFlt-1/FLAG and the expression of sFlt-1 was detected by immunofluorescent assay and ELISA. Corning® Transwell® Filter Inserts containing polyethylene terephthalate (PET) membranes with pore sizes of 3 μm were used as an experimental model to simulate THP-1 migration. Five VEGF concentrations (0, 0.1, 1, 10 and 100 ng/ml), four concentrations of sFlt-1(1–3)/FLAG expression supernatants (0.1, 1, 10 and 100 ng/ml), and monocyte chemoattractant protein-1 (MCP-1, 10 ng/ml) were used to test the ability of THP-1 cells to migrate through PET membranes.
Results
The sFlt-1(1–3) gene was successfully recombined into Ad-sFlt-1/FLAG. sFlt-1(1–3) was expressed in L929 cells transfected with Ad-sFlt-1/FLAG. THP-1 cell migration increased with increasing concentrations of VEGF, while cell migration decreased with increasing concentrations of sFlt1(1–3)/FLAG. sFlt1(1–3)/FLAG had no effect on MCP-1-induced cell migration.
Conclusions
This study demonstrated that VEGF is able to elicit a migratory response in THP-1 cells, and that sFlt-1(1–3) is an effective inhibitor of THP-1 migration towards VEGF.



Similar content being viewed by others
References
Noseworthy JH, Lucchinetti C, Rodriguez M, Weinshenker BG. Multiple sclerosis. N Engl J Med. 2000;343:938–52.
Brück W. The pathology of multiple sclerosis is the result of focal inflammatory demyelination with axonal damage. J Neurol. 2005;252(Suppl 5):v3–9.
Frohman EM, Racke MK, Raine CS. Multiple sclerosis—the plaque and its pathogenesis. N Engl J Med. 2006;354:942–55.
Imitola J, Chitnis T, Khoury SJ. Insights into the molecular pathogenesis of progression in multiple sclerosis: potential implications for future therapies. Arch Neurol. 2006;63:25–33.
Huitinga I, van Rooijen N, de Groot CJ, Uitdehaag BM, Dijkstra CD. Suppression of experimental allergic encephalomyelitis in Lewis rats after elimination of macrophages. J Exp Med. 1990;172:1025–33.
Huitinga I, Damoiseaux JG, Döpp EA, Dijkstra CD. Treatment with anti-CR3 antibodies ED7 and ED8 suppresses experimental allergic encephalomyelitis in Lewis rats. Eur J Immunol. 1993;23:709–15.
Proescholdt MA, Jacobson S, Tresser N, Oldfield EH, Merrill MJ. Vascular endothelial growth factor is expressed in multiple sclerosis plaques and can induce inflammatory lesions in experimental allergic encephalomyelitis rats. J Neuropathol Exp Neurol. 2002;61:914–25.
Graumann U, Reynolds R, Steck AJ, Schaeren-Wiemers N. Molecular changes in normal appearing white matter in multiple sclerosis are characteristic of neuroprotective mechanisms against hypoxic insult. Brain Pathol. 2003;13:554–73.
Kirk SL, Karlik SJ. VEGF and vascular changes in chronic neuroinflammation. J Autoimmun. 2003;21:353–63.
Su JJ, Osoegawa M, Matsuoka T, Minohara M, Tanaka M, Ishizu T, et al. Upregulation of vascular growth factors in multiple sclerosis: correlation with MRI findings. J Neurol Sci. 2006;243:21–30.
Marumo T, Schini-Kerth VB, Busse R. Vascular endothelial growth factor activates nuclear factor-kappaB and induces monocyte chemoattractant protein-1 in bovine retinal endothelial cells. Diabetes. 1999;48:1131–7.
Barleon B, Sozzani S, Zhou D, Weich HA, Mantovani A, Marmé D. Migration of human monocytes in response to vascular endothelial growth factor (VEGF) is mediated via the VEGF receptor flt-1. Blood. 1996;87:3336–43.
Kim I, Moon SO, Kim SH, Kim HJ, Koh YS, Koh GY. Vascular endothelial growth factor expression of intercellular adhesion molecule 1 (ICAM-1), vascular cell adhesion molecule 1 (VCAM-1), and E-selectin through nuclear factor-kappa B activation in endothelial cells. J Biol Chem. 2001;276:7614–20.
Shibuya M, Yamaguchi S, Yamane A, Ikeda T, Tojo A, Matsushime H, et al. Nucleotide sequence and expression of a novel human receptor-type tyrosine kinase gene (flt) closely related to the fms family. Oncogene. 1990;5:519–24.
Kondo K, Hiratsuka S, Subbalakshmi E, Matsushime H, Shibuya M. Genomic organization of the flt-1 gene encoding for vascular endothelial growth factor (VEGF) receptor-1 suggests an intimate evolutionary relationship between the 7-Ig and the 5-Ig tyrosine kinase receptors. Gene. 1998;208:297–305.
Kendall RL, Wang G, Thomas KA. Identification of a natural soluble form of the vascular endothelial growth factor receptor, FLT-1, and its heterodimerization with KDR. Biochem Biophys Res Commun. 1996;226:324–8.
Barleon B, Totzke F, Herzog C, Blanke S, Kremmer E, Siemeister G, et al. Mapping of the sites for ligand binding and receptor dimerization at the extracellular domain of the vascular endothelial growth factor receptor FLT-1. J Biol Chem. 1997;272:10382–8.
Ye C, Feng C, Wang S, Wang KZ, Huang N, Liu X, et al. sFlt-1 gene therapy of follicular thyroid carcinoma. Endocrinology. 2004;145:817–22.
Proescholdt MA, Heiss JD, Walbridge S, Mühlhauser J, Capogrossi MC, Oldfield EH, et al. Vascular endothelial growth factor (VEGF) modulates vascular permeability and inflammation in rat brain. J Neuropathol Exp Neurol. 1999;58:613–27.
Clauss M, Gerlach M, Gerlach H, Brett J, Wang F, Familletti PC, et al. Vascular permeability factor: a tumor-derived polypeptide that induces endothelial cell and monocyte procoagulant activity, and promotes monocyte migration. J Exp Med. 1990;172:1535–45.
Heil M, Clauss M, Suzuki K, Buschmann IR, Willuweit A, Fischer S, et al. Vascular endothelial growth factor (VEGF) stimulates monocyte migration through endothelial monolayers via increased integrin expression. Eur J Cell Biol. 2000;79:850–7.
Reinders ME, Sho M, Izawa A, Wang P, Mukhopadhyay D, Koss KE, et al. Proinflammatory functions of vascular endothelial growth factor in alloimmunity. J Clin Invest. 2003;112:1655–65.
Brück W, Sommermeier N, Bergmann M, Zettl U, Goebel HH, Kretzschmar HA, et al. Macrophages in multiple sclerosis. Immunobiology. 1996;195:588–600.
Shen H, Clauss M, Ryan J, Schmidt AM, Tijburg P, Borden L, et al. Characterization of vascular permeability factor/vascular endothelial growth factor receptors on mononuclear phagocytes. Blood. 1993;81:2767–73.
Ohtani K, Egashira K, Hiasa K, Zhao Q, Kitamoto S, Ishibashi M, et al. Blockade of vascular endothelial growth factor suppresses experimental restenosis after intraluminal injury by inhibiting recruitment of monocyte lineage cells. Circulation. 2004;110:2444–52.
Author information
Authors and Affiliations
Corresponding author
Additional information
Responsible editor: Graham Wallace.
Rights and permissions
About this article
Cite this article
Zhu, C., Xiong, Z., Chen, X. et al. Soluble vascular endothelial growth factor (VEGF) receptor-1 inhibits migration of human monocytic THP-1 cells in response to VEGF. Inflamm. Res. 60, 769–774 (2011). https://doi.org/10.1007/s00011-011-0332-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00011-011-0332-7