Abstract
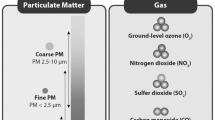
The evidence from a large number of studies indicates that exposures to current outdoor air pollution increase respiratory morbidity in children. Children with asthma, and those with asthma-like symptoms but without a diagnosis of asthma, are considered to be at highest risk of experiencing shortterm and/or longer-term adverse health effects. Many outdoor air pollutants readily penetrate indoors. Indoor air quality can deteriorate quickly when persistent and uncontrolled emissions occur and the ventilation/air exchange rate is reduced. It has been estimated that children spend 90% of their time indoors, including in school buildings, vehicles and public indoor environments. Environmental tobacco smoke is a well-recognized persistent indoor air contaminant with adverse health effects in children of all ages. Uncontrolled moisture in the indoor environment is increasingly recognized to significantly increase the risk of respiratory morbidity in children. The evidence that air pollutants singly and in combination with other environmental factors elicit adverse health responses in asthmatic and non-asthmatic children and adolescents, appears irrefutable.
Abrégé
Selon les observations de nombreuses études, l’exposition à la pollution actuelle de l’air extérieur ferait augmenter la morbidité respiratoire chez les enfants. Les enfants asthmatiques, et ceux qui présentent des symptômes d’asthme sans que la maladie ait été diagnostiquée, sont jugés les plus susceptibles de souffrir d’effets nocifs immédiats ou à long terme sur leur santé. Bon nombre de polluants de l’air extérieur pénètrent facilement à l’intérieur. La qualité de l’air intérieur peut se détériorer rapidement en présence d’émissions persistantes et incontrôlées, et si l’on réduit le rapport ventilation-échange d’air. On estime que les enfants passent 90 % de leur temps à l’intérieur, notamment dans les bâtiments scolaires, les véhicules et les lieux publics couverts. La fumée de tabac ambiante, un contaminant que l’on sait persister dans l’air intérieur, a des effets néfastes sur la santé des enfants de tout âge. On reconnaît de plus en plus que l’humidité non contrôlée du milieu intérieur accroît de façon considérable le risque de morbidité respiratoire chez les enfants. Les preuves que les polluants atmosphériques, seuls ou combinés à d’autres facteurs de l’environnement, provoquent des effets nocifs chez les enfants et adolescents asthmatiques et non asthmatiques semblent irréfutables.
Similar content being viewed by others
Bibliographie
Koren H, Utell MJ. Asthma and the environment. Environ Health Perspect 1997;105(5):534–37.
Bates, DV. Particulate air pollution. Thorax 1996;51:S3–S8.
Vincent R. Personal Communications.
Tattersfield, AE. Air pollution: Brown skies research. Thorax 1996;51:13–22.
Environment Canada. Urban Air Quality Environmental Indicator Bulletin State of the Environment Reporting, Ottawa, 1994.
Hilborn J, Still M. Canadian Perspectives on Air Pollution. Environment Canada, 1990.
Guidelines for the Index of the Quality of the Air. Report EPS 1/AP/3. Environment Canada, 1992.
Health Canada, Health and Environment, 1998.
Leech J, Wilby K, McMullen E, Laporte K, The Canadian Human Activity Pattern Study: Report of methods and population surveyed. Chron Dis Can 1996;17(3/4):118–23.
Samet JM, Spengler, JD. Indoor Air Pollution — A Health Perspective. Baltimore: The Johns Hopkins University Press, 1991.
Wallace L. Indoor particles: A review. J Air Waste Management 1996;46:98–126.
Trayer GW, Apte MG, Carruthers AR, et al. Indoor air pollution from wood-burning stoves. Environ Science Technol 1987;21:691–97.
Ott WR, Roberts, JW. Everyday exposure to toxic pollutants. Scientific American 1998;Feb 1998:86–91.
Dales RE, Kerr P, Schweitzer I, et al. Asthma management preceding an emergency department visit. Arch Intern Med 1992;152:2041–44.
American Thoracic Society. Guidelines as to what constitutes an adverse respiratory health effect, with special reference to epidemiologic studies on air pollution. Am Rev Respir Dis 1985;131:666–68.
Chang A, Phelan PD, Robertson, CF. Cough receptor sensitivity in children with acute and non-acute asthma. Thorax 1997;52:770–74.
Pope CA, Bates DV, Raizenne, ME. Health effects of particulate air pollution: Time for reassessment? Environ Health Perspect 1995;103(5):472–80.
Farlander-Braun JC, Vuille FH, Sennhauser U, et al. Respiratory health and long term exposure to air pollutants in Swiss school children. Am J Respir Crit Care Med 1997;155:1042–49.
Peters A, Dockery DW, Heinrich J, Wichmann EH. Medication use modifies the health effects of particulate sulfate and air pollution in children with asthma. Environ Health Perspect 1997;105:430–35.
Avol EL, Linn WS, Shamoo DA, et al. Shortterm respiratory effects of photochemical oxidant exposure in exercising children. JAPCA 1987;37:158–62.
Koenig JQ, Covert DS, Marshall SG, et al. The effects of ozone and nitrogen dioxide on pulmonary function in healthy and asthmatic adolescents. Am Rev Respir Dis 1987;136:1152–57.
McDonnell WF, Chapman RS, Leigh MW, et al. Respiratory responses of vigorously exercising children to 0.12 ppm ozone exposure. Am Rev Respir Dis 1985;132:875–79.
Raizenne ME, Burnett RT, Stern B, et al. Acute lung function responses to ambient acid aerosol exposures in children. Environ Health Perspect 1989;79:179–85.
Lippmann M. Health effects of the ozone: A critical review. J Air Pollut 1989;39:672–95.
Scarlett JF, Abbott KJ, Peacock JL, et al. Acute effects of summer air pollution on respiratory function in primary school children in southern England. Thorax 1996;51:1109–14.
Kinney PL, Thurston GD, Raizenne, ME. The effects of ambient ozone on lung function in children: A reanalysis of six summer camp studies. Environ Health Perspect 1996;104:170–74.
Burnett RT, Dales RE, Raizenne ME, et al. Effects of low ambient levels of ozone and sulfates on the frequency of respiratory admissions to Ontario hospitals. Environ Res 1994;65:172–94.
Manfreda J, Mao Y, Litven W. Morbidity and mortality for chronic obstructive lung disease. Am Rev Respir Dis 1989;140:S19–26.
Statistics Canada. Health Status of Canadians: Report of the 1991 General Social Survey. Ottawa: Minister of Industry, Science and Technology, Catalogue No. 11-612E, 1994.
Statistics Canada. National Population Health Survey Overview 1994–1995. Public Use Micro Data Files Catalogue No. 82F001XCB, 1995.
Dales RE, Raizenne M, El-Saadany S, et al. Prevalence of childhood asthma across Canada. Int J Epidemiol 1994;23:775–81.
King G, Pare, PD. Breathing easier. Can Med Assoc J 1997;157:1677–79.
Dockery DW, Cunningham J, Damokosh AI, et al. Health effects of acid aerosols on North American children: Respiratory symptoms. Environ Health Perspect 1996;104(5):500–5.
Health Canada, Student Lung Health Survey Final Descriptive Results 1995–96, Draft #1 Sentinel Health Unit Surveillance System — Asthma Component, Laboratory Centre for Disease Control, Respiratory Division, Bureau of Cardio-Respiratory Diseases and Diabetes, Ottawa, 1997.
American Thoracic Society. Health effects of outdoor air pollution. Am J Respir Crit Care Med 1996;153(1):3–50.
American Thoracic Society. Health effects of outdoor air pollution. Am J Respir Crit Care Med 1996;153(2):477–98.
Strachan DP, Cook, DG. Health effects of passive smoking: Parental smoking and lower respiratory illness in infancy and early childhood. Thorax 1997;52:905–14.
Rosentreich DL, Eggleson P, Kattan M, et al. The role of cockroach allergy and exposure to cockroach allergen in causing morbidity among inner-city children with asthma. N Engl J Med 1997;336:1356–63.
Hodges GR, Fink JN, Shlueter, DP. Hypersensitivity pneumonitis caused by a contaminated cool-mist vaporizer. Ann Intern Med 1974;80:501–4.
Michel O, Kips J, Duchateau J, et al. Severity of asthma is related to endotoxin in house dust. Am J Respir Crit Care Med 1996;154:1641–46.
Guidelines for indoor air quality in public buildings focusing on mycology. 1995. A federal government document.
Lemanske RF, Dick EC, Swenson CA, et al. Rhinovirus upper respiratory infection increases airway hyperactivity and late asthmatic reactions. J Clin Invest 1989;83:1–10.
Molfino NA, Wright SC, Katz I, et al. Effect of low concentrations of ozone on inhaled allergen responses in asthmatic subjects. Lancet 1991;338:199–203.
Air Quality Criteria Document for Ozone and Related Photochemical Oxidants, Volume III, July 1996, EPA/600/P-93/004cF.
Pope CA, Dockery DW, Spengler JD, Raizenne ME. Respiratory health and PM10 pollution: A daily time series analysis. Am Rev Respir Dis 1991;144:668–74.
Stern BR, Raizenne ME, Burnett RT, et al. Air pollution and childhood respiratory health: Exposure to sulfate and ozone in 10 Canadian rural communities. Environ Res 1994;66:125–42.
Ware JH, Ferris BG, Dockery DW, et al. Effects of ambient sulfur oxides and suspended particulates on respiratory health of preadolescent children. Am Rev Respir Dis 1986;133:834–42.
Raizenne M, Neas LM, Damokosh AI, et al. Health effects of acid aerosols on North American children: Pulmonary function. Environ Health Perspect 1996;104(5):506–51.
Koenig JQ, Covert DS, Hanley QS, et al. Prior exposure to ozone potentiates subsequent response to sulfur dioxide in adolescent asthmatic subjects. Am Rev Respir Dis 1990;141:377–80.
Delfino RJ, Murphy-Moulton AM, Burnett RT, et al. Effects of ozone and particulate air pollution on emergency room visits for respiratory illnesses in Montreal. Am J Respir Crit Care Med 1997;155:568–76.
Woodruff TJ, Grillo J, Schoendorf, KC. The relationship between selected causes of postneonatal infant mortality and particulate air pollution in the United States. Environ Health Perspect 1997;105(6):608–12.
Samet JM, Lambert WE, Skipper BJ, et al. A study of respiratory illness in infants and nitrogen dioxide exposure. Arch Environ Health 1992;47:57–63.
Dockery DW, Spengler JD, Speizer F, et al. Associations of health status with indicators of indoor air pollution from an epidemiologic study in six U. S. cities. Indoor Air 1987;2:203–7.
Dekker C, Dales R, Bartlett S, et al. Childhood asthma and the indoor environment. Chest 1991;100(4):922–26.
Spengler J, Neas L, Nakai S, et al. Respiratory symptoms and housing characteristics. Indoor Air 1994;4:72–82.
Maier WC, Arrighi MH, Morray B, et al. Indoor risk factors for asthma and wheezing among Seattle school children. Environ Health Perspect 1997;105:208–14.
Corne JM, Holgate, ST. Mechanisms of virus induced exacerbations of asthma. Thorax 1997;52:380–89.
Author information
Authors and Affiliations
Corresponding author
French language version/Version en Français
Rights and permissions
About this article
Cite this article
Raizenne, M., Dales, R. & Burnett, R. Air Pollution Exposures and Children–s Health. Can J Public Health 89 (Suppl 1), S47–S53 (1998). https://doi.org/10.1007/BF03405095
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03405095