Abstract
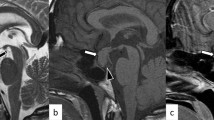
Growth hormone overproduction is characterized by increased size of visceral organs as well as growth of bone and soft tissues. We describe a case of a 23-year-old female acromegalic patient, who had been previously unsuccessfully operated upon by transsphenoidal pituitary surgery and then irradiated. In November 1987 a routine X-ray chest examination revealed a mediastinal mass, subsequently confirmed by CT scan. The patient underwent surgical removal of the mass: macroscopical aspect, histological sections and immunocytochemistry showed typical thymic structures without any evidence of neurosecretory activity. No GH-positive cells were found and only small amounts of immunoreactive GHRH like material (9.2 ng/g wet wg) were detected in the tumor extract. Before surgery plasma GHRH levels were not elevated (26 pg/ml); serum GH and IGF-I levels were 27.4 ± 4.9 μg/l and 191 nmol/l, respectively, and remained unchanged after surgery. These data ruled out a GHRH and/or GH ectopic production, confirming the primitive pituitary origin of acromegaly in this patient. It is likely that thymic hyperplasia may be explained by longstanding overproduction of GH and the young age of the patient.
Similar content being viewed by others
References
Nabarro J.D.N. Acromegaly. Clin. Endocrinol. (Oxf.) 26: 481, 1987.
Rosai J., Levine G.D. Tumors of the thymus. Atlas of tumor pathology. American Forces Institute of Pathology, Washington, 1976, p. 26.
Soudjian J.V., Moinar G.D., Silverstein M.N., Titus J.L Morphological studies of the thymus in acromegaly, diabetes mellitus, and Cushing’s syndrome. Metabolism 19: 40, 1970.
Sano T., Asa S.L, Kovacs K. Growth hormone-releasing hormone-producing tumors: clinical, biochemical and morphological manifestations. Endocr. Rev. 9: 357, 1988.
Arosio M., Moriondo P., Travaglini P., Ambrosi B., Beck Peccoz P., Conti Puglisi F., Secchi F., Faglia G. Modifications in serum growth hormone concentration induced by sulpiride in acromegalic patients pretreated with dopamine, bromocriptine and meter-goline. J. Clin. Endocrinol. Metab. 51: 454, 1980.
De Toni G., Aicardi G., Bulgarelli R., Dalla Volta A., De Toni E., Gobessi I. Trattato di pediatria e puericultura. Edizioni Minerva Medica, Saluzzo, 1968, Vol. II, p. 358.
Arliss J., Scholes J., Dickson P.R., Messina J.J. Massive thymic hyperplasia in an adolescent. Ann. Thorac. Surg. 45: 220, 1988.
Losa M., Wolfram G., Mojto G., Schopohl J., Spiess Y., Huber R., Müller O.A., Von Werder K. Presence of growth hormone-releasing hormone like-immunoreactivity in human tumors: characterization of immunological and biological properties. J. Clin. Endocrinol. Metab. 70: 62, 1990.
Sternberger I.A. Immunocytochemistry. Prentice-Hall Inc., Englewood Cliffs, New York, 1974.
Levenston S.A., McKeel D.W., Buckley P.J., Deuschryver K., Greider M.H., Jaffe B.M., Daughaday W.H. Acromegaly and Cushing’s syndrome associated with a foregut carcinoid tumor. J. Clin. Endocrinol. Metab. 53: 682, 1981.
Schulte H.M., Benker G., Windeck R., Olbricht T., Reinwein D. Failure to respond to growth hormone releasing hormone (GHRH) in acromegaly due to a GHRH secreting pancreatic tumor: dynamics of multiple endocrine testing. J. Clin. Endocrinol. Metab. 61: 585, 1985.
Hofman W.J., Moller P., Otto H.F. Thymic hyperplasia. II. Lymphofollicular hyperplasia of the thymus. An immunohistologic study. Klin. Wochenschr. 65: 53, 1987.
Iudd R. L. Massive thymic hyperplasia with myoid cell differentiation. Hum. Pathol. 78: 1180, 1987.
Rosati A., Pisascane A., Palmieri B., Ruco L.P., Baroni C.D. True thymic hyperplasia: presence of vimentin+/desmin+ cells. Proceedings of XVII International Congress of the International Academy of Pathology and the 8th World Congress of Academic and Environmental Pathology. Dublin, September 4–9, 1988, p. 111. (Abstract)
Talwar G.P., Hanjan S.N.S., Kidwai Z., Gupta P.D., Mehrotra N.N., Saxena R., Bhattarai Q. Growth hormone action on thymus and lymphoid cells. In: Pecile A., Muller E.E. (Eds.), Growth hormone and related peptides. Elsevier Science Publisher B.V., New York, 1976, p. 104.
Lesniak M.A., Roth J., Gordon P., Gavin J.R. III. Human growth hormone radioreceptor assay using cultured human lymphocytes. Nature 241: 20, 1973.
Kelley K.W., Brief S., Westly H.J., Novakovsky J., Bechtel P.J., Simon J., Walker E.B. GH3 pituitary adenoma cells can reverse thymic aging in rats. Proc. Natl. Acad. Sci. USA 83: 5663, 1986.
Arrenbrecht S. Specific binding of growth hormone to thymocytes. Nature 252: 255, 1974.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Bazzoni, N., Ambrosi, B., Arosio, M. et al. Acromegaly and thymic hyperplasia: a case report. J Endocrinol Invest 13, 931–935 (1990). https://doi.org/10.1007/BF03349660
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03349660