Abstract
Sodium ipodate (IPO) has been shown to bind nuclear T3 receptors (NT3R) in vitro, but previous studies have conflicted in regard to demonstration of this interaction in vivo. We sought evidence for IPO-NT3R binding in vivo by giving large doses of IPO to thyroidectomized (TDX) rats replaced with low doses of T3. We predicted that IPO-NT3R binding would inhibit T3 induced increases in mitochondrial alpha glycerophosphate dehydrogenase activity (alpha-GPDH) in kidney, heart and liver. Three groups of ten euthyroid rats each received 13 daily injections of vehicle, or 6 or 12 mg/100 g body weight of IPO, respectively. Both doses of IPO resulted in decreases in serum T3 and increases in serum TSH. Liver and kidney alpha-GPDH, however, were decreased only in the group receiving 6 mg IPO. In addition, three groups of 30 TDX rats were implanted with osmotic minipumps that contained T3 in the following concentrations: 33, 69 and 96 ng/ul. Ten rats in each group received 13 daily injections of vehicle, or IPO (vide supra). The alpha-GPDH responses were complex in that there was significant interaction between T3 and IPO effects in the kidney (A×B F ratio 5.13, p<0.001) and liver (A×B F ratio 2.85, p<0.05). The major finding, however, was that alpha-GPDH was not significantly reduced by IPO in any T3 replaced group. Rather, in all three organs, alpha GPDH was significantly increased above that produced by T3 alone by at least one combination of IPO and T3. Changes in serum TSH also suggested that IPO could enhance T3 effects. We conclude that IPO-NT3R binding is not a prominent mechanism via which the drug attenuates T3 effects in vivo. The data suggest that IPO may enhance T3 effects at the cellular level and that this enhancement may not be reflected by routinely monitored serum TSH. The latter observation may have clinical importance.
Similar content being viewed by others
References
Eil C., Chestnut R.Y. The effects of radiographic contrast agents and other compounds on the nuclear binding of L-[125|] triiodothyronine in dispersed human fibroblasts. J. Clin. Endocrinol. Metab. 60: 548, 1985.
DeGroot L.J., Rue P.A. Roentgenographic contrast agents inhibit triiodothyronine binding to nuclear receptors in vitro. J. Clin. Endocrinol. Metab. 49: 538, 1979.
Burman K.D., Lukes Y.G., Latham K.R., Wartofsky L. Ipodate and 8-anilino-1-naphthalene sulfonic acid block receptor binding of T-3 in rat liver. Horm. Metab. Res. 12: 685, 1980.
Kaplan M.M., Utiger R.D. lodothyronine metabolism in rat liver homogenates. J.Clin. Invest. 61: 459, 1978.
Chopra I.J., Huang T-S., Hurd R.E., Solomon D.H. A study of cardiac effects of thyroid hormones: evidence for amelioration of the effects of thyroxine by sodium ipodate. Endocrinology 114: 2039, 1984.
Melmed S., Melson M., Kaplowitz N., Yamada T., Hershman J.M. Glutathione dependent thyroxine 5′-monodeiodination modulates growth hormone production by cultured nonthyrotropic rat pituitary cells. Endocrinology 108: 970, 1981.
DeVito W.J., Connors J.M., Hedge G.A. The pituitary TSH response to TRH is inversely related to the plasma TSH concentration and directly related to the pituitary TSH content during hypothyroidism in the rat. Acta Endocrinol. (Copenh.) 114: 27, 1987.
Lee Y-P., Lardy H.A. Influence of thyroid hormones of L-alpha-glycerophosphate dehydrogenase and other dehydrogenases in various organs of the rat. J. Biol. Chem. 240: 1427, 1965.
Smallridge R.C., Rogers J., Verma P.S. Serum angiotensin converting enzyme: alterations in hyperthyroidism, hypothyroidism and subacute thyroiditis. JAMA 250: 2489, 1983.
Rohrbach M.S. [Glycine-1-14C] Hippuryl-L-histidyl-1 leucine: a substrate for the radiochemical assay of angiotensin converting enzyme. Anal. Biochem. 84: 272, 1978.
Lowry O.H., Rosebrough N.J., Farr A.L., Randall R.J. Protein measurement with the Folin phenol reagent. J. Biol. Chem. 193: 265, 1951.
Smallridge R.C., Verma P.S. Angiotensin-converting enzyme activity is altered in the hypothyroid rat. 7th International Congress of Endocrinology, Excerpta Medica: International Congress Series 652, 1984, p. 1489 (abstract).
Wu S-Y., Chopra I.J., Solomon D.H., Johnson D.E. The effect of repeated administration of ipodate (Oragrafin) in hyperthyroidism. J. Clin. Endocrinol. Metab. 47: 1358, 1978.
Lim V.S., Zavala D.C., Flanigan M.J., Freeman R.M. Blunted peripheral tissue responsiveness to thyroid hormone in uremic patients. Kidney Int. 31: 808, 1987.
Sogol P.B., Hershman J.M., Reed A.W., Dillmann W.H. The effects of amiodarone on serum thyroid hormones and hepatic thyroxine 5′-monodeiodination in rats. Endocrinology 113: 1464, 1983.
Felicetta J.V., Bagchi N., Brown T.R., Czanko R. Amiodarone and ipodate reduce hepatic levels of thyroid-sensitive enzymes. Clin. Res. 34: 908A, 1986.
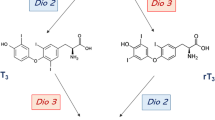
Chopra I.J., Solomon D.H., Chopra U., Wu S.Y., Fisher D.A., Nakamura Y. Pathways of metabolism of thyroid hormones. Recent. Prog. Horm. Res. 34: 521, 1978.
Obregon M.J., Pascual A., Mallol J., Morreale de Escobar G., Escobar del Rey F. Evidence against a major role of L-thyroxine at the pituitary level: Studies in rats treated with iopanoic acid (Telepaque). Endocrinology 106: 1827, 1980.
Pascual A., Montiel F., Aranda A. Effects of iopanoic acid on thyroid hormone receptor, growth hormone production, and triiodothyronine generation from thyroxine in pituitary GH1 cells. Endocrinology 120: 1089, 1987.
Felicetta J.V., Czanko R., Huber-Smith M.J., McCann D.S. Cholecystographic agents and sulfobromophthalein inhibit the binding of L-thyroxine to plasma membranes of rat hepatocytes. Endocrinology 118: 2500, 1986.
Silva J.E., Larsen P.R. Contributions of plasma triiodothyronine and local thyroxine monodeiodination to triiodothyronine to nuclear triiodothyronine receptor saturation in pituitary, liver and kidney of hypothyroid rats. J. Clin. Invest. 61: 1247, 1978.
Van Doorn J., Roelfsema F., Van Der Heide D. Concentrations of thyroxine and 3, 5, 3′ — triiodothyronine at 34 different sites in euthyroid rats as determined by isotopic equilibrium technique. Endocrinology 117: 1201, 1985.
Caldwell G., Errington M., Toft A.D. Resistant hyperthyroidism induced by sodium ipodate used as treatment for Graves’ disease. Acta Endocrinol. (Copenh.) 120: 215, 1989.
Author information
Authors and Affiliations
Additional information
The opinions or assertations contained herein are the private views of the authors and are not to be construed as official or reflecting the views of the Department of the Army or the Department of Defense.
Rights and permissions
About this article
Cite this article
Hays, J.H., Eil, C. & Smallridge, R.C. Sodium ipodate increases triiodothyronine action in vivo . J Endocrinol Invest 15, 507–512 (1992). https://doi.org/10.1007/BF03348793
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03348793