Abstract
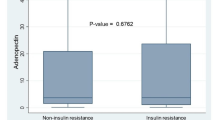
Several studies have demonstrated that low levels of serum adiponectin are present in obesity, insulin resistance, hypertension and hyperlipidemias. The aim of our study was to determine whether serum adiponectin level is different between patients with polycystic ovarian syndrome (PCOS) and control subjects. We also investigated relationships between various cardiovascular risk factors, levels of serum adiponectin and other hormones, such as androstendione, testosterone, estradiol, DHEAS, sex hormone binding globulin (SHBG), and leptin. We also analysed the correlation between serum adiponectin and free androgen index. Ninety-one women with clinical diagnosed PCOS and 53 healthy control subjects, carefully matched by body mass index (BMI) and age, were enrolled in the study. The fasting blood samples were obtained and all participants underwent an oral 75 g glucose tolerance test. The prevalences of impaired glucose tolerance (IGT), hypertension and hypertriglyceridemia were higher in the PCOS group. PCOS women had increased androgen concentrations and higher free androgen index and decreased level of serum SHBG. Lower serum adiponectin concentrations were observed among cases than in controls (median 13.7 μg/ml vs 17.8 μg/ml, p<0.001) despite being matched by BMI. In the PCOS group adiponectin levels correlated significantly with: BMI (r=−0.32, p=0.002), waist circumference (r=−0.32, p=0.003), waist-to-hip ratio (WHR, r=−0.38, p=0.001), triglycerides (r=−0.31, p=0.007), SHBG (r=0.30, p=0.003) and free androgen index (r=−0.29, p=0.02). In contrast, the adiponectin level does not appear to be related to total testosterone, DHEAS and leptin levels. The adiponectin and SHBG levels were found to be decreased in PCOS women with IGT compared to PCOS women with normal glucose tolerance, but after adjustment by BMI or WHR, the differences were no longer statistically significant. To exclude a possible confounding effect due to a higher prevalence of IGT in the PCOS group, this comparison was repeated for the subgroup of 58 PCOS women and 48 control women after excluding those with IGT. Neither adiponectin nor SHBG were significantly different between those subgroups. Multiple regression analysis revealed that serum adiponectin concentrations were best predicted by WHR, free androgen index and presence of IGT when all patients were considered. In PCOS subjects, the only independent predictor of adiponectin concentrations was glucose tolerance status. Conclusions: Lower adiponectin levels were observed in PCOS group than in control women, and these differences were probably due to higher prevalence of IGT in these cases.
Similar content being viewed by others
References
Carmina E, Lobo RA. Polycystic ovary syndrome (PCOS): arguably the most common endocrinopathy is associated with significant morbidity in women. J Clin Endocrinol Metab 1999, 84: 1897–9.
Vrbikova J, Cifkova R, Jirkovska A, et al. Cardiovascular risk factors in young Czech females with polycystic ovary syndrome. Hum Reprod 2003, 18: 980–4.
Legro RS, Kunselman AR, Dodson WC, Dunaif A. Prevalence and predictors of risk for type 2 diabetes mellitus and impaired glucose tolerance in polycystic ovary syndrome: a prospective, controlled study in 254 affected women. J Clin Endocrinol Metab 1999, 84: 165–169.
Pasquali R, Casimirri F. The impact of obesity on hyperandrogenism and polycystic ovary syndrome in premenopausal women. Clin Endocrinol (Oxf) 1993, 39: 1–16.
Wild S, Pierpoint T, McKeigue P, Jacobs H. Cardiovascular disease in women with polycystic ovary syndrome at longterm follow-up. A retrospective cohort study. Clin Endocrinol (Oxf) 2000, 52: 595–600.
Cibula D, Cifkova R, Fanta M, Poledne R, Zivny J, Skibova J. Increased risk of non-insulin dependent diabetes mellitus, arterial hypertension and coronary artery disease in perimenopausal women with a history of the polycystic ovary syndrome. Hum Reprod 2000, 15: 785–9.
Dahlgren E, Johansson S, Lapidus L, Oden A, Janson PO. Polycystic ovary syndrome and risk for myocardial infarction — evaluation from a risk factor model based on a porpective population study of women. Acta Obstet Gynecol Scand 1992, 71: 599–604.
Weyer C, Funahashi T, Tanaka S, et al. Hypoadiponectinemia in obesity and type 2 diabetes: close association with insulin resistance and hyperinsulinemia. J Clin Endocrinol Metab 2001, 86: 1930–5.
Adamczak M, Wiecek A, Funahashi T, Chudek J, Kokot F, Matsuzawa Y. Decreased plasma adiponectin concentration in patients with essential hypertension. Am J Hypertens 2003, 16: 72–5.
Ouchi N, Kihara S, Arita Y, et al. Novel modulator for endothelial adhesion molecules: adipocyte-derived plasma protein, adiponectin. Circulation 1999, 100: 2473–6.
Combs TP, Berg AH, Obici S, Scherer PE, Rossetti L. Endogenous glucose production is inhibited by the adipose-derived protein Acrp30. J Clin Invest 2001, 108: 1875–81.
Fruebis J, Tsao T-S, Javorschi S, et al. Proteolytic cleavage product of 30-kDa adipocyte complement-related protein increases fatty acid oxidation in muscle and causes weight loss in mice. Proc Natl Acad Sci 2001, 98: 2005–10.
Kubota N, Terauchi Y, Yamauchi T, et al. Disruption of adiponectin causes insulin resistance and neointimal formation. J Biol Chem 2002, 277: 25863–6.
Yamauchi T, Kamon J, Waki H, et al. The fat-derived hormone adiponectin reverses insulin resistance associated with both lipoatrophy and obesity. Nat Med 2001, 7: 941–6.
Tschritter O, Fritsche A, Thamer C, et al. Plasma adiponectin concentrations predict insulin sensitivity of both glucose and lipid metabolism. Diabetes 2003, 52: 239–43.
Spranger J, Kroke A, Mohlig M, et al. Adiponectin and protection against type 2 diabetes mellitus. Lancet 2003, 361: 226–8.
Abbasi F, Reaven GM. Evaluation of the quantitative insulin sensitivity check index as an estimate of insulin sensitivity in humans. Metabolism 2002, 51: 235–7.
Cibula D, Skrha J, Hill M, et al. Prediction of insulin sensitivity in nonobese women with polycystic ovary syndrome. J Clin Endocrinol Metab 2002, 87: 5821–5.
Jayagopal V, Kilpatrick ES, Jennings PE, Hepburn DA, Atkin SL. The biological variation of testosterone and sex hormonebinding globulin (SHBG) in polycystic ovarian syndrome: implications for SHBG as a surrogate marker of insulin resistance. J Clin Endocrinol Metab 2003, 88: 1528–33.
Nestler JE, Powers LP, Matt DW, et al. A direct effect of hyperinsulinemia on serum sex hormone-binding globulin levels in obese women with the polycystic ovary syndrome. J Clin Endocrinol Metab 1991, 72: 83–9.
Yu JG, Javorschi S, Hevener A, et al. The effect of thiazolidinediones on plasma adiponectin levels in normal, obese, and type 2 diabetic subjects. Diabetes 2002, 51: 2968–74.
Rexrode KM, Manson JE, Lee IM, et al. Sex hormone levels and risk of cardiovascular events in postmenopausal women. Circulation 2003, 108: 1688–93.
Orio FJ, Palomba S, Cascella T, et al. Adiponectin levels in women with polycystic ovary syndrome. J Clin Endocrinol Metab 2003, 88: 2619–23.
Sarrel PM. Cardiovascular aspects of androgens in women. Semin Reprod Endocrinol 1998, 16: 121–8.
Phillips GB, Jing TY, Laragh JH. Serum sex hormone levels in postmenopausal women with hypertension. J Hum Hypertens 1997, 11: 523–6.
Elbers JM, Giltay EJ, Teerlink T, et al. Effects of sex steroids on components of the insulin resistance syndrome in transsexual subjects. Clin Endocrinol (Oxf) 2003, 58: 562–71.
Nishizawa H, Shimomura I, Kishida K, et al. Androgens decrease plasma adiponectin, an insulin-sensitizing adipocytederived protein. Diabetes 2002, 51: 2734–41.
Dieudonne MN, Pecquery R, Boumedienne A, Leneveu MC, Giudicelli Y. Androgen receptors in human preadipocytes and adipocytes: regional specificities and regulation by sex steroids. Am J Physiol Cell Physiol 1998, 274: C1645–52.
Matsubara M, Maruoka S, Katayose S. Inverse relationship between plasma adiponectin and leptin concentrations in normal-weight and obese women. Eur J Endocrinol 2002, 147: 173–80.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sieminska, L., Marek, B., Kos-Kudla, B. et al. Serum adiponectin in women with polycystic ovarian syndrome and its relation to clinical, metabolic and endocrine parameters. J Endocrinol Invest 27, 528–534 (2004). https://doi.org/10.1007/BF03347474
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03347474