Abstract
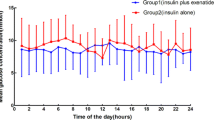
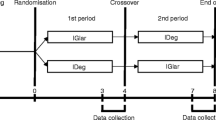
The effect of octreotide on morning hyperglycemia and GH levels was evaluated in eight insulin-dependent diabetic patients. Octreotide (50 mcg) was administered through subcutaneous injections at different hours (20: 00, 22: 00 and 24: 00h) or through continuous subcutaneous night infusion from midnight to 08: 00 at increasing rate between 03: 00 and 08: 00h. After octreotide injection at midnight we noticed a sharp decrease of both glycemia (p<0.005) and GH (p<0.05) at 04: 00h, but not at 08: 00h. Only the night continuous infusion at increasing rate was able to reduce glycemia and GH at 04: 00 and at 08: 00h (p<0.001 and p<0.01 respectively). The injections of octreotide at 20: 00 and 22: 00h lowered GH values at 24: 00h (p<0.01 and p<0.05 vs insulin alone) but did not show any signicant effect on blood glucose levels and GH at 04: 00 and 08: 00h. In conclusion, only the continuous subcutaneous night infusion of octreotide at increasing rate during the last hours of the night was able to reduce simultaneously morning hyperglycemia and GH levels in insulin-dependent diabetic patients, whereas evening subcutaneous injections at different times did not show any appreciable effect.
Similar content being viewed by others
References
Campbell P.J., Bolli G.B., Cryer P.E., Gerich J.E. Sequence of event during development of the dawn phenomenon in insulin-dependent diabetes mellitus. Metabolism 34: 1100, 1985.
Davidson M.B., Harris M.D., Ziel F.H., Rosenberg C.S. Suppression of sleep-induced growth hormone secretion by anticholinergic agents abolishes dawn phenomenon. Diabetes 37: 166, 1988.
Perriello G., De Feo G., Bolli P. The dawn phenomenon: nocturnal blood glucose homeostasis in insulin dependent diabetes mellitus. Diabet. Med. 5: 13, 1988.
Atiea J.A., Creagh F., Page M., Owens D.R., Scanlon M.F., Peter J.R. Eearly morning hyperglycaemia in insulin dependent diabetes: acute and sustained effects of cholinergic blockade. J. Clin. Endocrinol. Metab. 69: 390, 199.
Edge J.A., Dunger D.B., Matthews D.R., Gilbert J.P., Smith CP. Increased overnight growth hormone concentration in diabetic compared with normal adolescents. J. Clin. Endocrinol. Metab. 71: 1356, 1990.
Horner J.M., Kempt S.F., Hintz R.L. Growth hormone and somatomedin in insulin-dependent diabetes mellitus. J. Clin. Endocrinol. Metab. 53: 1148, 1981.
Lunetta M., Di Mauro M., Le Moli R., Nicoletti F. Effect of octreotide on blood glucose and counter-regulatory hormones in insulin-dependent diabetic patients: the role of dose and route of administration. Eur. J. Clin. Pharmacol. 51: 139, 1996.
Navascues I., Gil J., Pascau C., Senen D., Del Pozo E., Serrano Rios M. Effect of a long acting somatostatin derivative SMS 201–995 (Sandostatin) on glucose homeostasis in type 1 diabetes mellitus. Horm. Res. 29: 92, 1988.
Serrano-Rios M., Navascues J., Saban J., Ordonez A., Sevilla F., Del Pozo E. Sandostatin analog SMS 21–995 and insulin needs in insulin-dependent diabetic patients studied by means of an artificial pancreas. J. Clin. Endocrinol. Metab. 63: 1071, 1986.
Nosari I., Lepore G., Querci F., Maglio M.L., Sileo F., Pagani G. Effects of a somatostatin derivative (SMS 2 995) on postprandial hyperglycemia in insulin-dependent diabetics studied by means of a closed-loop device. J. Endocrinol. Invest. 12: 413, 1989.
Plewe G., Niken G., Krause U., Del Pozo E., Beyer J. Somatostatin analogue SMS 201–995 in type 1 diabetes mellitus. Initial experience after repeated administration. Scand. J. Gastroenterol. 21(Suppl. 119): 166, 1986.
Grossman L.D., Shumak S.L., George S.R., Singer W., Zinnan B. The effects of SMS 201–995 (Sandostatin) on metabolic profiles in insulin-dependent diabetes mellitus. J. Clin. Endocrinol Metab. 68: 63, 1989.
Hyer S.L., Sharp P.S., Brooks R.A., Burrin J.M., Kohner E.M. Continuous subcutaneous octreotide infusion markedly suppresses IGF-I levels whilst only partially suppressing GH secretion in diabetics with retinopathy. Acta Endocrinol. (Copenh.) 120: 187, 1989.
Osei K., O D’Dorisio T.M., Malarkey W.B., Cataland S. Continuous subcutaneous octreotide infusion: dose-response relationships between metabolic effects and octreotide clearance in patients with insulin-dependent (type 1) diabetes. J. Lab. Clin. Med. 118: 56, 1991.
Christensen S.E., Weelke J., Orskov N., Moller N., Flyvbjerg A., Harris A.G., Lud E., Jorgensen J. Continuous subcutaneous pump infusion of somatostatin analogue SMS 201–995 vs subcutaneous injection schedule in acromegalic patients. Clin. Endocrinol. (Oxf.) 24: 297, 1987.
Aarsen R.S.R., Bruining G.J., Grose W.F.A., Van Strik R., Lamberts S.W.J., Harris A. Long-acting somatostatin analogue (Sandostatin) reduces late night insulinopenic ketogenesis in diabetic teenagers. Acta Endocrinol. 116(Suppl. 28): 645, 1987.
Willms B., Harris A., Mehmke B. Effect if a single nocturnal administration of a long acting somatostatin analog, SMS 201–995 on blood glucose profile during the night, human growth hormone and Cortisol secretion in type 1 (insulin-dependent) diabetic patients. Diabetologia 30: 597 A, 1987.
Osei K., O’Dorisio M., Malarkey W.B., Craig E.L., Cataland S. Metabolic efficts of long-acting somatostatin analogue (Sandostatin) in type 1 diabetic patients on conventional therapy. Diabetes 38: 704, 1989.
Wurzburger M.I., Prelevic G.M., Sonksen P.H., Balint-Peri LA. The effect of the somatostatin analogue octreotide on growth hormone secretion in insulin-dependent without residual insulin secretion. Horm. Metab. Res. 24: 329, 1992.
Bolli G., Perriello G., Fanelli C., De Feo P. Nocturnal blood glucose control in type I diabetes mellitus. Diabetes Care 16(Suppl. 3): 71, 1993.
Borissova A.M., Kozlowski P., Popova J., Kirilov G. Morning peripheral insulin effectiveness and night changes in growth hormone, blood glucose and basal insulin needs in patients with type 1 diabetes mellitus. Diabetes Metab. 18: 463, 1992.
Perriello G., De Feo P., Torlone E., Fanelli C., Santeusanio F., Brunetti P., Bolli G.B. Nocturnal spikes of growth hormone secretion cause the dawn phenomenon in type 1 diabetes mellitus by decreasing hepatic (extraepatic) sensitivity to insulin in absence of insulin waning. Diabetologia 33: 52, 1190.
Bauer W., Brinr V., Doepner W., Hall R., Hueguenin R., Marbach P., Petcher T.J., Pless J. SMS 201–995 a very potent and selective octapeptide analogue of somatostatin with prolonged action. Life Sci. 31: 1133, 1982.
Del Pozo E., Kutz K. Pharmacological properties and effect on glucose homeostasis of a somatostatin derivative (SMS 201–995): studies in humans. In: Ludecke, Tolis, (Eds.), Growth factors and acromegaly. Reaven Press, New York, 1987, p. 207.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Lunetta, M., Di Mauro, M. & Le Moli, R. Different effects of octreotide by continuous night infusion at increasing rate or by evening injections at different times on morning hyperglycemia and growth hormone levels in insulin-dependent diabetic patients. J Endocrinol Invest 21, 454–458 (1998). https://doi.org/10.1007/BF03347326
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03347326