Abstract
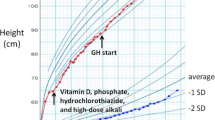
We report a child with Noonan syndrome, referred with severe short stature (height −5.4 SD) and biochemical features of GH resistance. The Noonan syndrome phenotype was confirmed by a clinical geneticist, however analysis of the protein tyrosine phosphatase nonreceptor type 11 (PTPN11) gene showed no mutation. Baseline serum IGF-I, IGF-binding protein 3 (IGFBP-3) and acid-labile subunit (ALS) were low, and in an IGF-I generation test, IGF-I did not increase into the normal range and IGFBP-3 and ALS did not change. These results are consistent with GH resistance. Treatment with human GH (hGH) was given in a dose of 0.05 mg/kg/day and height velocity increased from 5.6 to 10.7 cm/yr during the first year, and 8.9 cm/yr during the second year of therapy. Height standard deviation score has increased by 1.85 after 2 and a half yr of therapy. Serum IGF-I, IGFBP-3 and ALS values increased well into the normal range. This case shows that the potential value of GH therapy must be evaluated in each patient individually and that an excellent response may occur in a child with a PTPN11-negative genotype.
Similar content being viewed by others
References
Zenker M, Buheitel G, Rauch R, et al. Genotype-phenotype correlations in Noonan syndrome. J Pediatr 2004, 144: 368–74.
Tartaglia M, Mehler EL, Goldberg R, et al. Mutations in PTPN11, encoding the protein tyrosine phosphatase SHP-2, cause Noonan syndrome. Nat Genet 2001, 29: 465–8.
Nora JJ, Nora AH, Sinha AK, Spangler RD, Lubs HA. The Ullrich-Noonan syndrome (Turner phenotype). Am J Dis Child 1974, 127: 48–55.
Ahmed ML, Foot AB, Edge JA, Lamkin VA, Savage MO, Dunger DB. Noonan’s syndrome: Abnormalities of the growth hormone/IGF-I axis and the response to treatment with human biosynthetic growth hormone. Acta Paediatr Scand 1991; 80: 446–50.
Cotterill A, McKenna WJ, Brady AF, et al. The short-term effects of growth hormone therapy on height velocity and cardiac ventricular wall thickness in children with Noonan’s Syndrome. J Clin Endocrinol Metab 1996, 81: 2291–7.
Binder G, Neuer K, Ranke MB, Wittekindt NE. PTPN11 mutations are associated with mild growth hormone resistance in individuals with Noonan syndrome. J Clin Endocrinol Metab 2005, 90: 5377–81
Ferreira LV, Souza SA, Arnhold IJ, Mendoca BB, Jorge AA. PTPN11 (protein tyrosine phosphatase, nonreceptor type 11) mutations and response to growth hormone therapy in children with Noonan syndrome. J Clin Endocrinol Metab 2005, 90: 5156–60
Limal JM, Parfait B, Cabrol S, et al. Noonan syndrome: relationships between genotype, growth, and growth factors. J Clin Endocrinol Metab 2006, 91: 300–6.
MacFarlane CE, Brown DC, Johnston LB, et al. Growth hormone therapy and growth in children with Noonan’s syndrome: results of 3 years’ follow up. J Clin Endocrinol Metab 2001, 86: 1953–6.
Kirk JM, Betts PR, Butler GE, et al. Short stature in Noonan syndrome: response to growth hormone therapy. Arch Dis Child 2001, 84: 440–3.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Walton-Betancourth, S., Martinelli, C.E., Thalange, N.K.S. et al. Excellent growth response to growth hormone therapy in a child with PTPN11-negative Noonan syndrome and features of growth hormone resistance. J Endocrinol Invest 30, 439–441 (2007). https://doi.org/10.1007/BF03346324
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03346324