Abstract
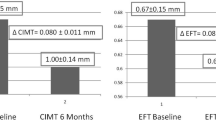
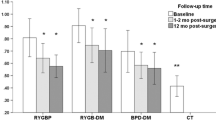
The aim of this study was to investigate the direct involvement of hyperinsulinaemia, DHEA and DHEA-S [DHEA(S)] in severe obesity in early carotid atherosclerosis, measured as intima-media thickness (IMT). Seventeen normotensive premenopausal women with very high BMI (43.5±1.6 kg/m2) were recruited for the study. Six women were also evaluated 12 months after laparoscopic adjustable silicone gastric banding (LASGB). Dietary intake, fasting plasma lipid profile, glycemic and insulinemic response to the OGTT, adrenal secretion, at baseline and after ACTH stimulation test, were measured. IMT, common carotid diameter (CD) and left ventricular mass index (LVMi) were measured by B-mode echotomography. All obese subjects showed higher fasting and stimulated insulin levels, but lower DHEA(S) levels than controls, showing a negative correlation between both fasting and stimulated insulin and DHEA(S), either at baseline or after ACTH testing. IMT was higher (p<0.05) than controls, with a positive correlation with stimulated insulin (p<0.05) and a strong negative correlation with DHEA(S) (p<0.001). In a multiple linear regression analysis, insulin response to OGTT maintained an association with DHEA(S) independent of fasting insulin, while DHEA maintained the association with IMT independent of stimulated insulin (p<0.0001). In the six patients evaluated 12 months after LASGB, fasting insulin levels decreased, while DHEA(S) levels increased (p<0.05). In conclusion, an early cardiovascular involvement was detected in this group of severe obese with hyperinsulinaemia and low DHEA(S), even in the absence of other well known CVD risk factors.
Similar content being viewed by others
References
Laakso M., Sarlund H., Salonen R., et al. Asymptomatic atherosclerosis and insulin resistance. Arterioscler. Thromb. 1991, 11: 1068–1076.
De Fronzo R.A., Ferrannini E.F. Insulin resistance: a multifactorial syndrome responsible for NIDDM, obesity, hypertension, dyslipidemia and atherosclerotic cardiovascular disease. Diabetes Care 1991, 14: 173–194.
Björntorp P. Body fat distribution, insulin resistance, and metabolic diseases. Nutrition 1997, 13: 795–803.
Seidell J.C. Time trends in obesity: an epidemiological perspective. Horm. Metab. Res. 1997, 29: 155–158.
Haffner SM. The importance of hyperglycemia in the nonfasting state to the development of cardiovascular disease. Endocr. Rev. 1998, 19: 583–592.
Laakso M., Lehto S. Epidemiology of risk factors for cardiovascular disease in diabetes and impaired glucose tolerance. Atherosclerosis 1998, 137: S65–73.
Wild R.A. Obesity, lipids, cardiovascular risk, and androgen excess. Am. J. Med. 1995, 16: 27S–32S.
Khaw K.T. Dehydroepiandrosterone, dehydroepiandrosterone sulphate and cardiovascular disease. J. Endocrinol. 1996, 150: S149–153.
Dunaif A. Insulin resistance and the polycystic ovary syndrome: mechanism and implications for pathogenesis. Endocr. Rev. 1997, 18: 774–800.
Carmina E., Lobo R.A. Polycystic ovary syndrome (PCOS): arguably the most common endocrinopathy is associated with significant morbidity in women. J. Clin. Endocrinol. Metab. 1999, 84: 1897–1899.
Nestler J.E. Regulation of human dehydroepiandrosterone metabolism by insulin. Ann. N. Y. Acad. Sci. 1995, 774: 73–81.
Yamaguchi Y., Tanaka S., Yamakawa T., et al. Reduced dehydroepiandrosterone levels in diabetic patients with hyperinsulinaemia. Clin. Endocrinol. (Oxf) 1998, 49: 377–383.
Feldman H.A., Johannes C.B., McKinlay J.B., Longcope C. Low dehydroepiandrosterone sulfate and hearth disease in middle-aged men: cross-sectional results from the Massachusetts Male Aging Study. Ann. Epidemiol. 1998, 8: 217–228.
Johannes C.B., Stellato R.K., Feldman H.A., Longcope C., McKinlay J.B. Relation of dehydroepiandrosterone and dehydroepiandrosterone sulfate with cardiovascular disease risk factors in women: longitudinal results from the Massachusetts Women’s Health Study. J. Clin. Epidemiol. 1999, 52: 95–103.
De Pergola G., Giagulli V.A., Garruti G., et al. Low dehydroepiandrosterone circulating levels in premenopausal obese women with very high body mass index. Metabolism 1991, 40: 187–190.
De Pergola G., Zamboni M., Sciaraffia M., et al. Body fat accumulation is possibly responsible for lower dehydroepiandrosterone circulating levels in premenopausal obese women. Int. J. Obes. Relat. Metab. Disord. 1996, 20: 1105–1110.
Orentreich N., Brind J., Rizer R., Vegelman J. Age changes and sex differences in serum dehydroepiandrosterone sulfate concentrations throughout adulthood. J. Clin. Endocrinol. Metab. 1985, 59: 551–555.
Barrett-Connor E., Ferrara A. Dehydroepiandrosterone, dehydro-epiandrosterone sulphate, obesity, waist-hip ratio, and noninsulin dependent diabetes in post-menopausal women: the Rancho Bernardo Study. J. Clin. Endocrinol. Metab. 1996, 81: 59–64.
Ivandic A., Prpic-Krizevac I., Sucic M., Juric M. Hyperinsulinaemia and sex hormones in healthy premenopausal women: relative contribution of obesity, obesity type, and duration of obesity. Metabolism 1998, 47: 13–19.
Vicennati V., Calzoni F., Gambineri A., et al. Secretion of major adrenal androgens following ACTH administration in obese women with different body fat distribution. Horm. Metab. Res. 1998, 30: 133–136.
Maccario M., Mazza E., Ramunni J., et al. Relationships between dehydroepiandrosterone sulphate and anthropometric, metabolic and hormonal variables in a large cohort of obese women. Clin. Endocrinol. (Oxf.) 1999, 50: 595–600.
Salonen J.T., Salonen R. Ultrasonographically assessed carotid morphology and the risk of coronary heart disease. Arterioscler. Thromb. 1991, 11: 1245–1249.
De Luca N., Rosiello G., Lamenza F., et al. Reversal of cardiac and large artery structural abnormalities induced by long term antihypertensive treatment with trandolapril. Am. J. Cardiol. 1992, 70: 52–59.
Crouse J.R. III, Craven T.E., Hagaman A.P., Bond M.G. Associations of coronary disease with segment specific intimal-medial thickening of the extracranial carotid artery. Circulation 1995, 92: 1141–1147.
Kuzmak L.I. A review of seven years’ experience with silicone gastric banding. Obes. Surg. 1991, 1: 403–408.
Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 1997, 20: 1183–1197.
Carnovale E., Marletta L. Tabelle di Composizione degli Alimenti. Istituto Nazionale della Nutrizione, Roma, 1997.
Wilkstrand J., Wendelhang I. Quantitative ultrasonography of carotid and femoral arteries. In: Lantzer P., Rösch J. (Eds.), Vascular diagnostics. Springer-Verlag, Heidelberg, 1994, pp.129–138
National Institut of Health Consensus Development Conference Statement. Gastrointestinal Surgery for severe obesity. National Institutes of Health, Bethesda, MD, 1991.
Angrisani L., Lorenzo M., Esposito G., et al. Laparoscopic adjustable silicone gastric banding: preliminary results of Naples experience. Obes. Surg. 1997, 7: 19–21.
Moghetti P., Castello R., Negri C., et al. Insulin infusion amplifies 17a-hydroxycorticosteroid intermediates response to adrenocorticotropin in hyperandrogenic women: apparent relative impairment of 17,20 lyase activity. J. Clin. Endocrinol. Metab. 1996, 81: 881–886.
De Pergola G., Ciccone M., Pannacciulli N., et al. Lower insulin sensitivity as an independent risk factor for carotid wall thickening in normotensive, non-diabetic, non-smoking normal weight and obese premenopausal women. Int. J. Obes. Relat. Metab. Disord. 2000, 24: 825–829.
Zietz B., Watzlawek E., Palitzsch K.D., Scholmerich J., Schaffler A. GG-genotype in the promotor region of uncoupling-protein-1 gene is associated with lower level of dehydroepiandrosterone in type 2 diabetes. Exp. Clin. Endocrinol. Diabetes 2001, 109: 102–106.
Clore J.N. Dehydroepiandrosterone and body fat. Obes. Res. 1995, 3: 613S–616S.
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article is available at http://dx.doi.org/10.1007/BF03345190.
Rights and permissions
About this article
Cite this article
Savastano, S., Valentino, R., Belfiore, A. et al. Early carotid atherosclerosis in normotensive severe obese premenopausal women with low DHEA(S). J Endocrinol Invest 26, 236–243 (2003). https://doi.org/10.1007/BF03345163
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03345163