Abstract
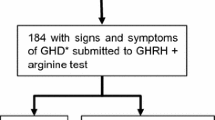
Primary empty sella (PES) is generally not associated with overt endocrine abnormalities, although mild hyperprolactinemia and, in children, deficient GH secretion have been reported. The aim of this multi-center collaborative study was to evaluate basal and stimulated GH secretion in a large series of adult PES patients. The study group consisted of 51 patients [41 women and 10 men, age range: 20–78 yr; (mean±SD) 47±11 yr]; results were compared with those in normal subjects (Ns) (Ns: no.=110, 55 women, age: 20–50 yr, 37±14 yr), and in hypopituitaric patients (HYP) with GH deficiency (HYP: no.=44, 17 women, age: 20–72, 49±16 yr). Baseline IGF-I levels and GH responses to insulin-induced hypoglycemia (insulin tolerance test, ITT) and/or GHRH+arginine (ARG) stimulation tests were evaluated. PES patients were also subdivided according to BMI in lean (BMI <28 kg/m2 no.=22) or obese (BMI >28 kg/m2 no.=29). PES patients had serum total IGF-I concentrations (mean±SE: 142.2±9.6 ng/ml) higher than HYP patients (77.4±6.4 ng/ml, p<0.001), but lower than Ns (213.3±17.2 ng/ml, p<0.005), with no differences between lean and obese PES subjects. The increase in serum GH concentrations following ITT and/or GHRH+ARG stimulation tests, although higher than that observed in HYP patients, was markedly reduced with respect to Ns. No difference was observed in the GH response to provocative tests between lean and obese PES patients. When individual GH responses to ITT or GHRH+ARG were taken into account, a large proportion of PES patients (52% after ITT, 61% after GHRH+ARG) showed a GH peak increase below the 1st centile of normal limits. Serum IGF-I levels in PES patients with blunted GH responses to provocative tests were significantly (p<0.001) lower in PES patients with normal GH responses, and a positive correlation was observed between IGF-I levels and serum GH peak concentrations after GHRH+ARG. In conclusion, the results of the present study provide evidence that adult PES patients often have an impairment of GH secretion, as indicated by the blunted GH response to ITT and GHRH+ARG provocative tests, and by the reduction in serum IGF-I levels. These changes are independent of body mass.
Similar content being viewed by others
References
Bergland R.M., Ray B.S., Torack R.M. Anatomical variations in the pituitary gland and adjacent structures in 225 human autopsy cases. J. Neurosurg. 1968, 28: 93–99.
Kaufman B. The “empty” sella turcica: a manifestation of the intrasellar subarachnoid space. Radiology 1968, 90: 931–941.
Lambert M., Gaillard R.C., Vallotton M.B., Megret M., Delavelle J. Empty sella syndrome associated with diabetes insipidus: case report and review of the literature. J. Endocrinol. Invest. 1989, 12: 433–437.
Gallardo E., Schacter D., Caceres E., et al. The empty sella: results of treatment in 76 successive cases and high frequency of endocrine and neurological disturbances. Clin. Endocrinol. (Oxf.) 1992, 37: 529–533.
Brismar K., Efendic S. Pituitary function in the empty sella syndrome. Neuroendocrinology 1981, 32: 70–77.
Buchfelder M., Brockmeier S., Pichl J., Schrell U., Fahlbush R. Results of dynamic endocrine testing of hypothalamic pituitary function in patients with a primary “empty” sella syndrome. Horm. Metab. Res. 1989, 21: 573–576.
Ishikawa S., Furuse M., Saito T., Okada K., Kuzuya T. Empty sella in control subjects and patients with hypopituitarism. Endocrinol. Jpn. 1988, 35: 665–674.
Impallomeni M., Yeo T., Rudd A., Carr D., Aber V. Investigation of anterior pituitary function in elderly patients over the age of 75. Quart. J. Med. 1987, 63: 505–515.
Pocecco M., De Campo C., Marinoni S., et al. High frequency of empty sella syndrome in children with growth hormone deficiency. Helv. Paediatr. Acta 1989, 43: 295–301.
Cacciari E., Zucchini S., Ambrosetto P., et al. Empty sella in children and adolescents with possible hypothalamic-pituitary disorders. J. Clin. Endocrinol. Metab. 1994, 78: 767–771.
De Boer H., Block G., van Der Veen E.A. Clinical aspects of growth hormone deficiency in adults. Endocr. Rev. 1995, 16: 63–86.
Growth Hormone Research Society (GRS). Consensus guidelines for diagnosis and treatment of adults with GH deficiency: summary statement of Growth Hormone Research Society workshop on adult growth hormone deficiency. J. Clin. Endocrinol. Metab. 1998, 83: 379–381.
Hoffman D.M., O’Sullivan A.J., Baxter R.C., Ho K.Y. Diagnosis of growth hormone deficiency in adults. Lancet. 1994, 1: 1064–1068.
Thorner M.O., Bentsson B.A., Ho K.Y., et al. Diagnosis of growth hormone deficiency in adults. J. Clin. Endocrinol. Metab. 1995, 80: 3097–3098.
Svensson J., Johannsson G., Bengtsson B.A. Insulin-like growth factor-I in growth hormone-deficient adults: relationship to population-based normal value, body composition and insulin tolerance test. Clin. Endocrinol. (Oxf.) 1997, 46: 579–586.
Jones S.L., Trainer P.J., Perry L., Wass J.A.H., Besser G.M., Grossman A. An audit of the insulin tolerance test in adult subjects in an acute investigation unit over one year. Clin. Endocrinol. (Oxf.) 1994, 41: 123–128.
Alba-Roth J., Muller O.A., Schopohl J., von Werder K. Arginine stimulates growth hormone secretion by suppressing endogenous somatostatin secretion. J. Clin. Endocrinol. Metab. 1988, 67: 1186–1189.
Ghigo E., Aimaretti G., Gianotti L., Bellone J., Arvat E., Camanni F. New approch to the diagnosis of growth hormone deficiency in adults. Eur. J. Endocrinol. 1996, 134: 352–356.
Aimaretti G., Corneli G., Razzore P., et al. Comparison between insulin-induced hypoglicemia and growth hormone (GH)-releasing hormone plus arginine as provocative test for the diagnosis of GH deficiency in adults. J. Clin. Endocrinol. Metab. 1998, 83: 1615–1618.
Bellone J., Aimaretti G., Bellone S., et al. Sequential administration of arginine and arginine plus GHRH to test somatotroph function in short children. J. Endocrinol. Invest. 2000, 23: 97–101.
Valetto M.R., Bellone J., Baffoni C., et al. Reproducibility of the growth hormone response to stimulation with growth hormone-releasing hormone plus arginine during lifespan. Eur. J. Endocrinol. 1996, 135: 568–572.
Gasperi M., Aimaretti G., Scarcello G., et al. Low dose hexarelin and growth hormone (GH)-releasing hormone as a diagnostic tool for the diagnosis of GH deficiency in adults: comparison with insulin-induced hypoglycemia test. J. Clin. Endocrinol. Metab. 1999, 84: 2633–2637.
Liotta A., Maggio C., Giuffrè M., Carta M., Manfrè L.J. Sequential contrast-enhanced magnetic resonance imaging in the diagnosis of growth hormone deficiencies. J. Endocrinol. Invest. 1999, 22: 740–746.
Hall K., Hilding A., Thoren M. Determinants of circulating insulin-like growth factor-I. J. Endocrinol. Invest. 1999, 22: 48–57.
Span J.P.T., Pieters G.F.F.M., Sweep C.G.J., Swinkels L.M.J.W., Smals A.G.H. Plasma IGF-I is a useful marker of growth hormone deficiency in adults. J. Endocrinol. Invest. 1999, 22: 446–450.
Maccario M., Gauna C., Procopio M., et al. Assessment of GH-IGF-I axis in obesity by evaluation of IGF-I levels and the GH response to GHRH+arginine test. J. Endocrinol. Invest. 1999, 22: 424–429.
Casanueva F.F., Villanueva L., Dieguez C, et al. Free fatty acids block growth hormone (GH) releasing hormone-stimulated GH secretion in man directly at the pituitary. J. Clin. Endocrinol. Metab. 1987, 65: 634–642.
Pombo M., Pombo C.M., Astorga R., et al. Regulation of growth hormone secretion by signals produced by the adipose tissue. J. Endocrinol. Invest. 1999, 22: 22–26.
Littley M.D., Shalet S.M., Beardwell C.G., Ahmed S.R., Applegate G., Sutton M.L. Hypopituitarism following external radiotherapy for pituitary tumours in adults. Q. J. Med. 1989, 70: 145–160.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gasperi, M., Aimaretti, G., Cecconi, E. et al. Impairment of GH secretion in adults with primary empty sella. J Endocrinol Invest 25, 329–333 (2002). https://doi.org/10.1007/BF03344013
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03344013