Summary
In general practice it is common to prescribe antibiotics for patients with acute bronchitis presumed to be of bacterial origin. This phase III double-blind randomised multicentre study compared the efficacy and safety of clarithromycin 250mg twice daily administered for 5 days, and azithromycin 500mg once daily on day 1 followed by 250mg once daily on days 2 to 5, in the treatment of 214 adult patients with acute bronchitis. Clinical evaluations were performed pretreatment, on day 6 or 7, and at a follow-up visit between 20 to 30 days after the start of treatment.
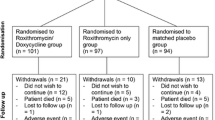
Of the 214 patients enrolled in the study, 109 were in the clarithromycin group and 105 in the azithromycin group. The groups were matched for age, sex, smoking history and severity of actual disease.
Both regimens were well tolerated and effective. No significant differences were observed between the clarithromycin and azithromycin groups in post-treatment clinical cure (65%, 70 of 108; 53%, 55 of 103, respectively), in clinical success (96%, 104 of 108; 92%, 95 of 103, respectively), in relapse rates (1%, 1 of 101; 2%, 2 of 95) or in the numbers of patients reporting drug- related adverse events (12%, 13 of 109; 16%, 17 of 105, respectively).
Clarithromycin, administered for 5 days, was at least as effective and as safe as a 5-day azithromycin regimen in the treatment of acute bronchitis.
Similar content being viewed by others
References
Adam D. Clarithromycin, 250mg twice daily for 5 days or 10 days, in the treatment of adult patients with bronchitis. Infection, in press, 1993
Anthonissen NR, Manfreda J, Warren CPW, et al. Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Annals of Internal Medicine 106: 196–203, 1987
O’Neill SJ, Millar ED, Coles SJ, Bachand RT. Safety and efficacy of clarithromycin in the treatment of acute mild to moderate respiratory tract infections. Irish Medical Journal 84: 33–35, 1991
Pennington JE. Community acquired pneumonia and acute bronchitis. In Pennington (Ed.) Respiratory infections: diagnosis and management, 2nd ed., pp. 159–170, Raven Press, New York, 1988
Peters DH, Clissold SP. Clarithromycin. A review of its antimicrobial activity, pharmacokinetic properties and therapeutic potential. Drugs 44: 117–164, 1992
Peters DH, Friedel HA, McTavish D. Azithromycin. A review of its antimicrobial activity, pharmacokinetic properties and clinical efficacy. Drugs 44: 750–799, 1992
Sanson-Fisher R, Bowman J, Armstrong S. Factors affecting nonadherence with antibiotics. Diagnostic Microbiology and Infectious Diseases 15: 103S–109S, 1992
Verhaegen J, Verbist L. Macroliden. Tijdschrift voor Genees- kunde 48: 908–913, 1992
Vogel F. Efficacy and tolerability of clarithromycin in the short-course treatment of acute respiratory tract infections. Drug Investigation 3: 205–209, 1991
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Vincken, W., Yernault, J.C. Efficacy and Tolerability of Clarithromycin versus Azithromycin in the Short-Course Treatment of Acute Bronchitis. Drug Invest. 6, 170–175 (1993). https://doi.org/10.1007/BF03259738
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03259738