Abstract
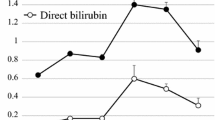
Hepatic venous oxygen saturation (Shvo2), parameters of systemic circulation and cytokine (Interleukin 6) (IL-6)) level were measured in 21 patients with thoracic esophageal cancer in order to analyze the mechanism of occurrence of postoperative hyperbilirubinemia (PHB). Shvo2 fell during operation, especially during intrathoracic procedures, and a significant correlation was noted between the total time during which Shvo2 was below 60% and the postoperative peak serum bilirubin level (peak-Bil) (r = 0.595, p = 0.0037). Patients with PHB (group H) had worse systemic circulation and a lower oxygen supply postoperatively than patients without PHB (group N). Body weight and water balance recovered earlier in group N. Postoperatively, numbers of peripheral lymphocytes and platelets changed lower in group H, while CRP and IL-6 changed higher in group H. Furthermore, a significant correlation was noted between the IL-6 level just after operation and peak-Bil (r = 0.669, p = 0.0006). These results suggests PHB results from intraoperative liver hypoxia and poor postoperative systemic circulation. Individual severeness of reactions to the operative stress, excessive or adequate, plays a role in the occurrenceof PHB as well.
Similar content being viewed by others
References
Shirota T, Sasajima K: Hyperbilirubinemia after esophagectomy. A possible role of lipid peroxidation. J Nippon Med Sch 59: 21–28, 1992
Tsujinaka T, Kido Y, Ogawa M, Shiozaki H, Murata A, Kobayasi K, Mori T: Postoperative hyperbilirubinemia after resection of thoracic esophageal cancer. Am J Gastroenterology 85: 1473–1479, 1990
Schmid M, Hefti ML, Gattiker R, Kistler HJ, Senning A: Benign postoperative intrahepatic cholestasis. N Engl J Med 272: 545–558, 1965
Members of the American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference Committee: Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med 20: 864–874, 1992
Gelman S: Disturbances in hepatic blood flow during anesthesia and surgery. Arch Surg 111: 881–883, 1976
Shoemaker WC, Appel PL, Kram HB, Waxman K, Lee TS: Prospective trial of supranormal values of survivors as therapeutic goals in high risk surgical patients. Chest 94: 1176–1186, 1988
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Saito, R., Kitamura, M., Minamiya, Y. et al. An analysis of the mechanism of postoperative hyperbilirubinemia following resection of thoracic esophageal cancer in terms of hepatic venous oxygen saturation and excessive systemic reactions. Jpn J Thorac Caridovasc Surg 46, 155–163 (1998). https://doi.org/10.1007/BF03250611
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF03250611