Abstract
Purpose
To determine the effect of isoflurane on motor evoked potentials (MEP) in a new animal model designed to verify the applicability of MEPs in brachial plexus surgery, and to compare the results with previous reports in other animals.
Methods
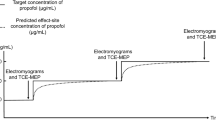
In seven goats, anesthesia was induced with 3 mg·kg−1 ketamine iv and maintained with nitrous oxide 40% in oxygen and 2 μg·kg−1·hr−1 fentanyl iv. The MEP were performed with two subcutaneous needle electrodes placed over the occiput (cathode) and the nasion (anode), with their plugs connected to the power output of a Digitimer D 180 electrical stimulator, connected to the trigger input of an electromyograph (model 8400, Cadwell Laboratories, Inc., Kennwick, Washington). Activation of the Digitimer caused central stimulation of the motor cortex, evoking baseline compound muscle action potentials (CMAPs) which were recorded from the left triceps muscle. Subsequently, isoflurane 2% was administered together with repeated central stimulation at 30 sec intervals.
Results
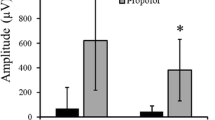
Onset of I-(indirect) waves increased from median 15,8 msec to median 26,8 msecP = 0,018 (latency increase ranged from: 9 to 11.5 msec), while peak-to-peak amplitudes decreased and subsequently disappeared. D-(direct) waves showed no latency increase, and finally disappeared as well. After disappearance of CMAPs, isoflurane administration was stopped and MEP repeated. The CMAPs reappeared (range: 210–360 sec) and regained initial peak-to-peak amplitudes and latencies.
Conclusion
These animal studies suggest that isoflurane should not be used during the recording of MEPs.
Résumé
Objectif
Déterminer l’effet de l’isoflurane sur les potentiels évoqués moteurs (PEM) chez un nouveau modèle animal conçu pour vérifier l’applicabilité des PEM à l’opération du plexus brachial, et comparer les résultats avec ceux d’articles antérieurs chez d’autres animaux.
Méthode
L’anesthésie a été induite chez sept chèvres avec 3 mg·kg−1 de kétamine iv et maintenue avec du protoxyde d’azote à 40% dans de l’oxygène et 2 μg·kg−1·hr−1 de fentanyl iv. Les PEM ont été réalisés avec deux aiguilles-électrodes sous-cutanées placées au niveau de l’occiput (cathode) et sur le nasion (anode) branchées à la borne d’entrée d’un électromyographe (modèle 8400, Cadwell Laboratories, Inc., Kennwick, Washington), leurs connecteurs étant reliés à la borne de sortie d’un stimulateur électrique Digitimer D 180. L’activation du Digitimer a provoqué une stimulation centrale du cortex moteur, évoquant les potentiels de base d’action musculaire combinée (PAMC) qui étaient enregistrés à partir des réactions du triceps gauche. Par la suite, l’isoflurane à 2% était administré en même temps qu’une stimulation centrale répétée à intervalles de 30 s.
Résultats
L’installation des ondes I (indirectes) a montré un accroissement d’une médiane de 15,8 msec à une médiane de 26,8 msecP = 0,018 (l’augmentation du temps de latence a varié de 9 à 11,5 msec), tandis que les amplitudes entre les pics ont baissé, puis disparu. Les ondes D (directes) n’ont pas présenté d’accroissement du temps de latence et ont finalement disparu également. Après la disparition des PAMC, l’administration d’isoflurane a été stoppée et le PEM, répété. Les PAMC sont réapparus (intervalle: 210–360 s) et ont affiché de nouveau les amplitudes entre les pics et les temps de latence initiaux.
Conclusion
Ces études animales suggèrent que l’isoflurane ne doit pas être utilisé pendant l’enregistrement des PEM.
Article PDF
Similar content being viewed by others
References
Merton PA, Morton HB. Stimulation of the cerebral cortex in the intact human subject. Nature 1980; 285: 227.
Turkof E, Monsivais J, Dechtyar I, Bellolo H, Millesi H, Mayr N. Motor evoked potential as a reliable method to verify the conductivity of anterior spinal roots in brachial plexus surgery: an experimental study on goats. J Reconstr Microsurg 1995; 11: 357–62.
Turkof E, Millesi H, Turkof R, Pfundner P, Mayr N. Intraoperative electroneurodiagnostics (transcranial electrical motor evoked potentials) to evaluate the functional status of anterior spinal roots and spinal nerves during brachial plexus surgery. Plast Reconstr Surg 1997; 99: 1632–41.
Turkof E, Monsivais J, Mayer N, Millesi H. The goat: a viable experimental anatomical model for testing spinal root conductivity with SSEP, MEP without laminectomy. Abstracts of the 11th Congress of the International Microsurgical Society; Rhodes, Greece, 1992; 51.
Turkof E, Bellolo H, Monsivais J. The anatomy of the vertebral column of the nubian goat: a peculiarity of the arcus vertebrae C5, C6 and C7 forming large spatia interarcualia. Can J Vet Res 1994; 58: 156.
Calancie B, Klose KJ, Baier S, Green BA Isofluraneinduced attenuation of motor evoked potentials caused by electrical motor cortex stimulation during surgery. J Neurosurg 1991; 74: 897–904.
Hicks RG, Woodforth IJ, Crawford MR, Stephen JPH, Burke DJ. Some effects of isoflurane on I waves of the motor evoked potential. Br J Anaesth 1992; 69: 130–6.
Schmid UD, Boll J, Liechti S, Schmid J, Hess CW. Influence of some anesthetic agents on muscle responses to transcranial magnetic cortex stimulation: a pilot study in humans. Neurosurgery 1992; 30: 85–92.
Haghighi SS, Green KD, Oro JJ, Drake RK, Kracke GR Depressive effect of isoflurane anesthesia on motor evoked potentials. Neurosurgery 1990; 26: 993–7.
Haghighi SS, Madsen R, Green KD, Oro JJ, Kracke GR Suppression of motor evoked potentials by inhalation anesthetics. J Neurosurg Anesthesiol 1990; 2: 73–8.
Zentner J, Kiss I, Ebner A Influence of anesthetics — nitrous oxide in particular — on electromyographic response evoked by transcranial electrical stimulation of the cortex. Neurosurgery 1989; 24: 253–6.
Toda Y. The effect of anesthetic agents on descending spinal cord evoked potential and the compound muscle action potentials elicited by stimuation at the cerebral motor cortex and the spinal cord. Japanese Journal of the Orthopaedic Association 1992; 66: 279–90.
Yamada H, Transfeldt EE, Tamaki T, Torres F, Iaizzo PA. The effects of volatile anesthetics on the relative amplitudes and latencies of spinal and mucsle potentials evoked by trancranial magnetic stimulation. Spine 1994; 19: 1512–7.
Amassian VE, Stewart M, Quirk GJ, Rosenthal JL. Physiological basis of motor effects of a transient stimulus to cerebral cortex. Neurosurgery 1987; 20: 74–93.
Jellinek D, Platt M, Jewkes D, Symon L. Effects of nitrous oxide on motor evoked potentials recorded from skeletal muscle in patients under total anesthesia with intravenously administered propofol. Neurosurgery 1991; 29: 558–62.
Zentner J, Albrecht T, Heuser D. Influence of halothane, enflurane and isoflurane on motor evoked potentials. Neurosurgery 1992; 31: 298–305.
Rothwell JC, Day BL, Thompson PD, Dick JPR, Marsden CD. Some experiences of techniques for stimulation of the human cerebral motor cortex through the scalp. Neurosurgery 1987; 20: 156–63.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Andel, H., Bayer, G.S., Ciovica, R. et al. Depressive effect of isoflurane on motor evoked potentials in the Nubian goat. Can J Anesth 47, 81–86 (2000). https://doi.org/10.1007/BF03020739
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF03020739