Abstract
Purpose
To asses the cardiovascular changes after either lightwand or conventional laryngoscopic endotracheal intubation (EI) in patients with coronary artery disease.
Methods
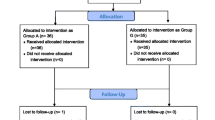
Following Institutional approval and informed consent, 80 consecutive patients undergoing elective coronary artery bypass grafting were enrolled in this prospective, controlled, single-blinded study. General anesthesia was induced with fentanyl 5 μ·kg−1 and thiopental 5 mg·kg−1 followed by pancuronium 0.1 mg·kg−1. After loss-of-eyelash reflex the lungs were manually ventilated with 2% isoflurane in oxygen for five minutes. Patients were then randomly allocated to receive either the lightwand (lightwand group,n = 41) or direct-vision laryngoscopy (laryngoscopy group,n = 39). Heart rate (HR) and direct blood pressure were recorded before induction, after induction but before EI, during EI, immediately after EI and at ten-second intervals for the following five minutes. Hemodynamic management during induction was standardized. Hypotension was treated with volume replacement, ephedrine, or phenylephrine as indicated; hypertension was treated withiv nitroglycerin; tachycardia was treated with boluses of esmolol; and, bradycardia was treated with atropine or ephedrine.
Results
In both groups, mean arterial blood pressures and HR increased significantly after EI. There was a tendency for the light-wand group to have lower arterial blood pressures and slower HR. However, the differences between the two groups did not reach statistical significance. Requirements for drugs to control HR and mean arterial pressure were similar in both groups.
Conclusion
In patients with coronary artery disease using a light-wand intubation technique does not modify the hemodynamic response associated with EI as compared with standard direct-vision laryngoscopy.
Résumé
Objectif
Évaluer les modifications cardiovasculaires suivant l’intubation endotrachéale (IE) avec un stylet lumineux ou un laryngoscope traditionnel chez des malades atteints de cardiopathie ischémique.
Méthode
Ayant reçu l’approbation de l’institution et le consentement éclairé des participants, nous avons recruté 80 patients consécutifs, qui devaient subir un pontage aortocoronarien, pour notre étude prospective, contrôlée et à simple insu. L’anesthésie générale a été induite avec 5 μg·kg−1 de fentanyl et 5 mg·kg−1 de thiopental, suivis de 0,1 mg·kg−1 de pancuronium. Après la perte du réflexe ciliaire, les poumons ont été ventilés manuellement avec de l’isoflurane à 2% dans de l’oxygène pendant cinq minutes. Les patients ont été répartis au hasard pour l’intubation avec le stylet lumineux (n =41) ou par laryngoscopie à vision directe (n = 39). La fréquence cardiaque (FC) et la tension artérielle (TA) directe ont été enregistrées avant l’induction, après l’induction mais avant l’IE, pendant l’IE, immédiatement après l’IE et à 10s d’intervalle pendant les cinq minutes suivantes. La prise en charge hémodynamique a été normalisée pendant l’induction. L’hypotension a été traitée par remplissage vasculaire, éphédrine, ou phényléphrine selon l’indication; l’hypertension, par nitroglycérine iv; la tachycardie, par de l’esmolol en bolus et la bradycardie, par de l’atropine ou de l’éphédrine.
Résultats
Dans les deux groupes, les tensions artérielles moyennes (TAM) et la FC ont significativement augmenté après l’IE. Dans le groupe d’intubation au stylet lumineux, les TA avaient tendance à baisser et la FC à ralentir. Cependant, les différences intergroupes n’étaient pas statistiquement significatives. Les besoins de médicaments pour contrôler la FC et la TAM ont été similaires dans les deux groupes.
Conclusion
Chez les malades atteints de cardiopathie ischémique, l’intubation avec un stylet lumineux, comparée à la laryngoscopie traditionnelle à vision directe, ne modifie pas la réponse hémodynamique associée à l’IE.
Article PDF
Similar content being viewed by others
References
Stoelting RK. Circulatory changes during direct laryngoscopy and tracheal intubation. Influence of duration of laryngoscopy with or without prior lidocaine. Anesthesiology 1977; 47: 381–3.
Ebert JP, Pearson JD, Gelman S, Harris C, Bradley EL. Circulatory responses to laryngoscopy: the comparative effects of placebo, fentanyl and esmolol. Can J Anaesth 1989; 36: 301–6.
Stone DJ, Gal TJ. Airway management.In: Miller RD (Ed.) Anesthesia, 5th ed. New York: Churchill Livingstone Inc.; 2000: 1444–6.
Hung OR, Pytka S, Morris I, et al. Clinical trial of a new lightwand device (Trachlight) to intubate the trachea. Anesthesiology 1995; 83: 509–14.
Hung OR, Pytka S, Morris I, Murphy M, Stewart RD. Lightwand intubation: II-clinical trial of a new lightwand for tracheal intubation in patients with difficult airways. Can J Anaesth 1995; 42: 826–30.
Montes FR, Sanchez SI, Giraldo JC, et al. The lack of benefit of tracheal extubation in the operating room after coronary artery bypass surgery. Anesth Analg 2000; 91: 776–80.
Knight RG, Castro T, Rastrelli AJ, Maschke S, Scavone JA. Arterial blood pressure and heart rate response to lighted stylet or direct laryngoscopy for endotracheal intubation. Anesthesiology 1988; 69: 269–72.
Casati A, Aldegheri G, Fanelli G, et al. Lightwand intubation does not reduce the increase in intraocular pressure associated with tracheal intubation. J Clin Anesth 1999; 11: 216–9.
Hirabayashi Y, Hiruta M, Kawakami T, et al. Effects of lightwand (Trachlight) compared with direct laryngoscopy on circulatory responses to tracheal intubation. Br J Anaesth 1998; 81: 253–5.
Friedman PG, Rosenberg MK, Lebenbom-Mansour M. A comparison of light wand and suspension laryngoscopic intubation techniques in outpatients. Anesth Analg 1997; 85: 578–82.
Takahashi S, Mizutani T, Miyabe M, Toyooka H Hemodynamic responses to tracheal intubation with laryngoscope versus lightwand intubating device (Trachlight®) in adults with normal airway. Anesth Analg 2002; 95: 480–4.
Nishikawa K, Omote K, Kawana S, Namiki A. A comparison of hemodynamic changes after endotracheal intubation by using the Lightwand device and the laryngoscope in normotensive and hypertensive patients. Anesth Analg 2000; 90: 1203–7.
O’Connor JP, Ramsay JG, Wynands JE, Kaplan JA. Anesthesia for myocardial revascularization.In: Kaplan JA (Ed.). Cardiac Anesthesia, 3th ed. Philadelphia: W.B. Saunders Company; 1993: 587–628.
Milocco I, Lof BA, William-Olsson G, Appelgren LK. Haemodynamic stability during anaesthesia induction and sternotomy in patients with ischaemic heart disease. A comparison of six anaesthetic techniques. Acta Anaesthesiol Scand 1985; 29: 465–73.
Atlee JL, Dhamee MS, Olund TL, George V. The use of esmolol, nicardipine, or their combination to blunt hemodynamic changes after laryngoscopy and tracheal intubation. Anesth Analg 2000; 90: 280–5.
Takita K, Morimoto Y, Kemmotsu O. Tracheal lidocaine attenuates the cardiovascular response to endotracheal intubation. Can J Anesth 2001; 48: 732–6.
Ko SH, Kim DC, Han YJ, Song HS. Small-dose fentanyl: optimal time of injection for blunting the circulatory responses to tracheal intubation. Anesth Analg 1998; 86: 658–61.
Splinter WM, Cervenko F. Haemodynamic responses to laryngoscopy and tracheal intubation in geriatric patients: effects of fentanyl, lidocaine and thiopentone. Can J Anaesth 1989; 36: 370–6.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Monte, F.R., Giraldo, J.C., Betancur, L.A. et al. Endotracheal intubation with a lightwand or a laryngoscope results in similar hemodynamic variations in patients with coronary artery disease. Can J Anesth 50, 824–828 (2003). https://doi.org/10.1007/BF03019380
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF03019380