Abstract
Purpose
To evaluate the tracheal intubating conditions and neuromuscular blocking charactenstics of divided dose mivacurium or single dose rocuronium.
Methods
Thirty-two patients undergoing elective surgery were studied. Anaesthesia was with propofol 2 mg · kg−1, followed by an infusion of l50 μg · kg−1 · min−1. Patients were randomized to receive either mivacurium-0.15 mg · kg−1 followed 30 sec later by 0.1 mg · kg−1, or rocuronium-0.9 mg · kg−1, followed 30 sec later by placebo. Tracheal intubating conditions were assessed 90 sec after the initial dose of relaxant by an anaesthetist who was unaware of patient group. The electromyographic (EMG) response of the first dorsal interosseus muscle to ulnar nerve train-of-four was measured.
Results
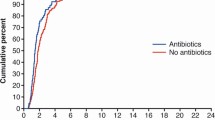
Successful tracheal intubation was performed in all patients after both mivacurium and rocuronium. Intubating conditions (jaw relaxation, open visible vocal cords) were judged to be good-excellent in all but one patient before insertion of the tracheal tube. However, patients receiving mivacunum were more likely to experience coughing and bucking after tracheal tube insertion (10/16 patients) than those receiving rocuronium (3/16 patients, P < 0.05). No patient in the rocuronium group experienced moderately vigorous coughing and bucking after insertion of the tracheal tube vs six patients in the mivacurium group (P < 0.05). Time to 10 and 25% recovery of neuromuscular function was faster (P < 0.05) after divided dose mivacunum (20 ± 1 and 23 ± 1 min, respectively) than after rocuronium (45 ± 5 and 57 ± 8 min, respectively).
Conclusion
The results suggest that, during conditions of the study, divided dose mivacurium is not recommended for a 90-sec tracheal intubation in patients where moderate coughing and bucking is deemed unacceptable.
Résumé
Objectif
Évaluer les conditions de l’intubation de la trachée et les caractéristiques du bloc neuromusculaire au mivacunum à dose fractionnée et au rocuronium à dose unique.
Méthodes
Cette étude réunissait 22 patients programmés pour une chirurgie non urgente. Lanesthésie était réalisée avec du propofol 2 mg · kg−1, suivi d’une perfusion de 150 μg · kg−1 · min−1. Les patients recevaient aléatoirement soit du mivacunum 0, 15 mg · kg−1 suivi 30 sec plus tard par 0, 1 mg · kg−1, sort du rocuronium 0, 9 mg · kg−1, suivi 30 sec plus tard d’un placebo. Les conditions d’intubation de la trachée étaient évaluées 90 sec après la dose initiale de myorelaxant par un anesthésiste ignorant le groupe auquel le patient appartenait. La réponse électromyographique (EMG) à la stimulation au train-de-quatre (TOF) du premier muscle interosseux dorsal était mesurée.
Résultats
Lintubation de la trachée a été réussie chez tous les patients des deux groupes. Les conditions d’intubation (relaxation de la mâchoire, visualisation de cordes vocales béantes) avant l’insertion de la canule tracheale étaient jugées de bonnes à excellentes chez tous les patients à l’exception d’un seul. Cependant, les patients sous mivacunum étaient plus sujets à la toux et au cabrage après l’insertion de la canule (10/16 patients) que ceux qui avaient reçu le rocuronium. (3/16 patients, P< 0,05). Aucun des patients du groupe rocuronium n’a présenté de toux et de cabrage notoires après l’insertion de la canule comparativement à six patients du groupe mivacunum (P< 0,05). Le temps de récupération à 10% et 25% de la fonction neuromusculaire était plus rapide (P< 0,05) après le mivacurium à dose fractionnée (respectivement 20±1 min et 23 ±1 min) qu’après le rocuronium (respectivement 45 ±5 et 57 ±8 min).
Conclusion
Ces résultats suggèrent que dans les conditions de l’étude, le mivacurium à dose fractionnée n’est pas recommandé après 90 sec pour une intubation de la trachée chez des patients chez qui une toux ou un cabrage d’intensité modérée sont jugés inacceptables.
Article PDF
Similar content being viewed by others
References
Levy JH, Davis GK, Duggan J, Szlam F. Determination of the hemodynamics and histamine release of rocuronium (ORG 9426) when administered in increased doses under N2O/O2 — sufentanil anesthesia. Anesth Analg 1994; 78: 318–21.
Magorian T, Flannery KB, Miller RD. Comparison of rocuronium, succinylcholine, and vecuronium for rapid-sequence induction of anesthesia in adult patients. Anesthesiology 1993; 79: 913–8.
Law Min JC, Bekavec I, Glavinovic MI, Donati F, Bevan DR. Iontophoretic study of speed of action of various muscle relaxants. Anesthesiology 1992; 77: 351–6.
Savarese JJ, Ali HH, Basta SJ, et al. The clinical neuromuscular pharmacology of mivacurium chloride (BW B1090U). A short-acting nondepolarizing ester neuromuscular blocking drug. Anesthesiology 1988; 68: 723–32.
Wrigley SR, Jones RM, Harrop-Griffiths AW, Platt MW. Mivacurium chloride: a study to evaluate its use during propofolnitrous oxide anaesthesia. Anaesthesia 1992; 47: 653–7.
Goldhill DR, Whitehead JP, Emmott RS, Griffith AP, Bracey BJ, Flynn PJ. Neuromuscular and clinical effects of mivacurium chloride in healthy adult patients during nitrous oxideenflurane anaesthesia. Br J Anaesth 1991; 67: 289–95.
Ali HH, Lien CA, Witkowski T, et al. Efficacy and safety of divided dose administration of mivacurium for a 90-second tracheal intubation. J Clin Anesth 1996; 8: 276–81.
Scheller MS, Zornow MH, Saidman LJ. Tracheal intubation without the use of muscle relaxants: a technique using propofol and varying doses of alfentanil. Anesth Analg 1992; 75: 788–93.
Donati F, Meistelman C. A kinetic-dynamic model to explain the relationship between high potency and slow onset time for neuromuscular blocking drugs. J Pharmacokinet Biopharm 1991; 19: 537–52.
Cantineau JP, Porte F, d’Honneur G, Duvaldestin P. Neuromuscular effects of rocuronium on the diaphragm and adductor pollicis muscles in anesthetized patients. Anesthesiology 1994; 81: 585–90.
Meistelman C, Plaud B, Donati F. Rocuronium (ORG 9426) neuromuscular blockade at the adductor muscles of the larynx and adductor pollicis in humans. Can J Anaesth 1992; 39: 665–9.
Wright PMC, Caldwell JE, Miller RD. Onset and duration of rocuronium and succinylcholine at the adductor pollicis and laryngeal adductor muscles in anesthetized humans. Anesthesiology 1994; 81: 1110–5.
Plaud B, Debaene B Lequeau F, Meistelman C, Donati F. Mivacurium neuromuscular block at the adductor muscles of the larynx and adductor pollicis in humans. Anesthesiology 1996; 85: 77–81.
Debaene B, Beaussier M, Meistelman C, Donati F, Lienhart A. Monitoring the onset of neuromuscular block at the orbicularis oculi can predict good intubating conditions during atracurium-induced neuromuscular block. Anesth Analg 1995; 80: 360–3.
Sayson SC, Mongan PD. Onset of action of mivacurium chloride. A comparison of neuromuscular blockade monitoring at the adductor pollicis and the orbicularis oculi. Anesthesiology 1994; 81: 35–42.
Davidson JAH, Gillespie JA. Tracheal intubation after induction of anaesthesia with propofol, alfentanil and i.v. lignocaine. Br J Anaesth 1993; 70: 163–6.
Mulholland D, Carlisle RJT. Intubation with propofol augmented with intravenous lignocaine. Anaesthesia 1991; 46: 312–3.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by the MetroHealth Foundation (N. Kamath). Presented in part at the Canadian Anaesthetists Society Annual Meeting, June, 1995 and the Ohio Society of Anesthesiologists Annual Meeting, September 9, 1995. Burroughs Wellcome Inc. donated the mivacurium, and Organon Inc. donated the rocuronium.
Rights and permissions
About this article
Cite this article
Patel, N., Kamath, N., Smith, C.E. et al. Intubating conditions and neuromuscular block after divided dose mivacurium or single dose rocuronium. Can J Anesth 44, 49–53 (1997). https://doi.org/10.1007/BF03014324
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF03014324