Abstract
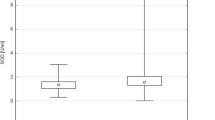
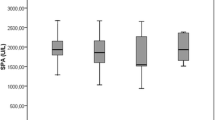
Reactive oxygen species and other free radicals are known to be the mediators of phenotypic and genotypic changes that lead from mutation to neoplasia. There are some primary antioxidants such as glutathione peroxidase (GPx), glutathione S-transferases (GSTs) and reduced glutathione, which protect against callular and molecular damage caused by the reactive oxygen metabolites (ROMs). The present study was conducted to determine the level of malondialdehyde (MDA), as an index of lipid peroxidation, along with the GPx, GSTs activities and level of reduced glutathione in 45 prostate cancer (PC) patients, 55 benign prostate hyperplasia (BPH) patients as compared to the controls. Significant higher levels of MDA and GSTs activities in the serum, (P<0.005) and significant lower levels of reduced GSH concentration and GPx activity in blood haemolysates (P<0.05) of PC and BPH patients were observed as compared to the controls. The relatively higher GSTs activity and low level of reduced GSH may be due to the response of increased reactive oxygen metabolites production in the blood. The higher MDA and lower GPx activities may be inadequate to detoxify high levels of H2O2 into H2O leading to the formation of the*OH radical followed by MDA. This result hypothesizes that oxidant-antioxidant imbalance may be one of the major factor responsible for the development of prostate cancer and benign prostate hyperplasia.
Similar content being viewed by others
References
Ray, G., Batra, S., Shukla, N.K., Deo, S., Raina, V., Ashok, S. and Husain, S.A. (2000) Lipid peroxidation free radical production and antioxidant status in breast cancer. Breast Cancer Res. Treat. 59, 163–70.
Zheng, Q.S., Sun, X.L. and Wang, C.H. (2002) Re-differentiation of human gastric cancer cells induced by ascorbic acid and sodium selenite. Biomed. Environ. Sci. 15, 223–232.
Olusi, S.O. (2002) Obesity is an independent risk factor plasma lipid peroxidation and depletion of erythrocyte cytoprotective enzymes in humans. Int. J. Obes. Relat. Metab. Disord. 26, 1159–64
Zima, T., Spicka, I., Stipek, S., Crkovska, J., Platenik, J., Merta, M. and Tesar, V. (1996) Antioxidant enzymes and lipid peroxidation in patients with multiple myeloma. Neoplasma 43, 69–73.
Sabitha, K.E. and Shyamaladevi, C.S. (1999) Oxidant and antioxidant activity changes in patients with oral cancer and treated with radiotherapy. Oral Oncol. 35, 273–277.
Ghalia, A.A., Rabboh, N.A., el, Shalakani, A., Seada, L. and Khalifa, A. (2000) Estimation of glutathione S-transferase and its Pi isoenzyme in tumor tissues and sera of patients with ovarian cancer. Anticancer Res. 20, 1229–1235.
Kehrer, J.P. (1993) Free radicals as mediators of tissue injury and disease. Critical reviews in toxicology, 23, 21–48.
Guven, M., Ozturk, B., Sayal, A., Ozeturk, A. and Ulutin, T. (1999) Lipid peroxidation and antioxidant system in the blood of cancerous patients with metastasis. Cancer Biochem. Biophys. 17, 155–162.
Yoshioka, T., Kawada, K., Shimada, T. and Mori, M. (1979) Lipid peroxidation in maternal and cord blood and protective mechanisms against activated oxygen toxicity in the blood. Am. J. Obster. Gynecology. 135, 372–376.
Habig, W.H., Pabst, M.J. and Jakoby W.B. (1974) Glutathione S-transferases. The first enzymatic step in mercapturic acid formation. J. Biol. Chem. 249, 7130–7139.
Beutler, E., Duron, O., and Kelly, B.M. (1961) Improved method for the determination of blood glutathione. J. Lab. and Clin. Med. May, 882–888.
Hayes, J.D. and Pulford, D.J. (1995) The Glutathione S-transferases (GST) supergene family: regulation of GST and contriburion of the isoenzymes to cancer prevention and drug resistance. Cret. Rev. Biochem. Mol. Biol. 30, 445–600.
Armstrong, R.N. (1997) Structure, catalytic mechanism and evolution of the glutathione transferases. Chem. Res. Toxicol. 10, 2–18.
Kitly, C.G. and Doyle, S.M. (1996). Glutathione S-transferases as a biomarkers of organ viability and damage. In: Vermeulen, N.P.E., Mulder, G.J., Nieuwenhuyse, H., Peters, W.H.M. and Van Bladerns, P.J., editors, Glutathione S-transferases: structure function and clinical implication. London: Taylor and Francis. pp.249–58.
Lee, W.H., Morton, R.A., Epstein, J.I., Brooks, J.D., Campbell, P.A., Bova, G.S., Hsieh, W.S., Isaacs, W.B. and Nelson, W.G. (1994) Cytidine methylation of regulatory sequences near the piclass glutathione S-transferase gene accompanies human prostatic carcinogenesis. Proc. Natl. Acad. Sci. USA, 91 (24), 11733–11737.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Srivastava, D.S.L., Mittal, R.D. Free radical injury and antioxidant status in patients with benign prostate hyperplasia and prostate cancer. Indian J Clin Biochem 20, 162–165 (2005). https://doi.org/10.1007/BF02867419
Issue Date:
DOI: https://doi.org/10.1007/BF02867419