Abstract
Purpose of Review
The 5-year survival rate of patients with pancreatic cancer (PanCA) has remained stagnant. Unfortunately, the incidence is almost equal to mortality rates. These facts underscore the importance of concerted efforts to understand the pathology of this disease. Deregulation of multiple signaling pathways involved in a wide variety of cellular processes including proliferation, apoptosis, invasion, and metastasis contribute not only to cancer development but also to therapeutic resistance. The purpose of this review is to summarize current understanding of etiological factors including emerging evidence on the role of infectious agents, factors associated with therapeutic resistance, and therapeutic options.
Recent Findings
The unique aspect of PanCA is “desmoplasia,” a process that involves proliferation of stromal fibroblasts and collagen deposition in and around the filtrating cancer. Recent studies have identified pancreatic stellate cells (PSCs) as a potential source of such desmoplasia. Biphasic interactions between PSCs and cancer cells, endothelial cells, and/or myeloid-derived suppressor cells in the tumor microenvironment contribute to pancreatic carcinogenesis.
Summary
We summarize limitations of current therapeutic approaches and potential strategies to overcome these limitations using natural products including botanicals as adjuvant/neo-adjuvant for effective management of PanCA.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Ilic M, Ilic I. Epidemiology of pancreatic cancer. World J Gastroenterol. 2016;22(44):9694–705. https://doi.org/10.3748/wjg.v22.i44.9694.
Wong C-H, Li Y-J, Chen Y-C. Therapeutic potential of targeting acinar cell reprogramming in pancreatic cancer. World J Gastroenterol. 2016;22(31):7046.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin. 2017;67(1):7–30. https://doi.org/10.3322/caac.21387.
Kamisawa T, Wood LD, Itoi T, Takaori K. Pancreatic cancer. Lancet. 2016;388(10039):73–85. https://doi.org/10.1016/s0140-6736(16)00141-0.
Ryan D, Hong T, Bardeesy N. Pancreatic adenocarcinoma. N Engl J Med. 2014;371:1039–49. https://doi.org/10.1056/NEJMra1404198.
Binenbaum Y, Na'ara S, Gil Z. Gemcitabine resistance in pancreatic ductal adenocarcinoma. Drug Resist Updat. 2015;23:55–68. https://doi.org/10.1016/j.drup.2015.10.002.
Jemal A. Global burden of cancer: opportunities for prevention. Lancet. 2012;380(9856):1797–9. https://doi.org/10.1016/S0140-6736(12)61688-2.
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136(5):E359–86. https://doi.org/10.1002/ijc.29210.
Silverberg E, Lubera J. Cancer statistics, 1987. CA Cancer J Clin. 1987;37(1):2–19.
Conroy T, Desseigne F, Ychou M, Bouché O, Guimbaud R, Bécouarn Y, et al. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med. 2011;364(19):1817–25. https://doi.org/10.1056/NEJMoa1011923.
Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62(1):10–29. https://doi.org/10.3322/caac.20138.
Zhen DB, Rabe KG, Gallinger S, Syngal S, Schwartz AG, Goggins MG, et al. BRCA1, BRCA2, PALB2, and CDKN2A mutations in familial pancreatic cancer: a PACGENE study. Genet Med : Off J Am Coll Med Genet. 2014; https://doi.org/10.1038/gim.2014.153.
Hruban RH, Canto MI, Goggins M, Schulick R, Klein AP. Update on familial pancreatic cancer. Adv Surg. 2009;44:293–311.
Habbe N, Langer P, Sina-Frey M, Bartsch DK. Familial pancreatic cancer syndromes. Endocrinol Metab Clin N Am. 2006;35(2):417–430, xi. https://doi.org/10.1016/j.ecl.2006.02.016.
• Bailey P, Chang DK, Nones K, Johns AL, Patch A-M, Gingras M-C, et al. Genomic analyses identify molecular subtypes of pancreatic cancer. Nature. 2016;531(7592):47–52. https://doi.org/10.1038/nature16965. http://www.nature.com/nature/journal/v531/n7592/abs/nature16965.html#supplementary-information . This pivotal study identifies four different molecular subsets of pancreatic cancer that may be utilized in developing more efficacious therapies for patients.
Barone E, Corrado A, Gemignani F, Landi S. Environmental risk factors for pancreatic cancer: an update. Arch Toxicol. 2016;90(11):2617–42. https://doi.org/10.1007/s00204-016-1821-9.
Pandol SJ, Apte MV, Wilson JS, Gukovskaya AS, Edderkaoui M. The burning question: why is smoking a risk factor for pancreatic cancer? Pancreatology : Off J Int Assoc Pancreatol (IAP) [et al]. 2012;12(4):344–9. https://doi.org/10.1016/j.pan.2012.06.002.
Maisonneuve P, Lowenfels AB. Risk factors for pancreatic cancer: a summary review of meta-analytical studies. Int J Epidemiol. 2015;44(1):186–98. https://doi.org/10.1093/ije/dyu240.
Bosetti C, Rosato V, Li D, Silverman D, Petersen GM, Bracci PM, et al. Diabetes, antidiabetic medications, and pancreatic cancer risk: an analysis from the International Pancreatic Cancer Case-Control Consortium. Ann Oncol. 2014;25(10):2065–72. https://doi.org/10.1093/annonc/mdu276.
Bosetti C, Lucenteforte E, Silverman DT, Petersen G, Bracci PM, Ji BT, et al. Cigarette smoking and pancreatic cancer: an analysis from the International Pancreatic Cancer Case-Control Consortium (Panc4). Ann Oncol. 2012;23(7):1880–8. https://doi.org/10.1093/annonc/mdr541.
Yadav D, Lowenfels AB. The epidemiology of pancreatitis and pancreatic cancer. Gastroenterology. 2013;144(6):1252–61. https://doi.org/10.1053/j.gastro.2013.01.068.
Go VL, Gukovskaya A, Pandol SJ. Alcohol and pancreatic cancer. Alcohol. 2005;35(3):205–11. https://doi.org/10.1016/j.alcohol.2005.03.010.
Song S, Wang B, Zhang X, Hao L, Hu X, Li Z, et al. Long-term diabetes mellitus is associated with an increased risk of pancreatic cancer: a meta-analysis. PLoS One. 2015;10(7):e0134321. https://doi.org/10.1371/journal.pone.0134321.
Lashinger LM, Ford NA, Hursting SD. Interacting inflammatory and growth factor signals underlie the obesity-cancer link. J Nutr. 2014;144(2):109–13. https://doi.org/10.3945/jn.113.178533.
McCall K, Schwartz AL, Schwartz FL. Linking obesity and pancreatic cancer. Pancreatic cancer—insights into molecular mechanisms and novel approaches to early detection and treatment 2014. p. 83–104.
Hassan M, Bondy M, Wolff R, Abbruzzese J, Vauthey J-N, Pisters P, et al. Risk factors for pancreatic cancer: case-control study. Am J Gastroenterol. 2007;102(12):2696–707. https://doi.org/10.1111/j.1572-0241.2007.01510.x.
Jiao L, de Gonzalez AB, Hartge P, Pfeiffer RM. Body mass index, effect modifiers, and risk of pancreatic cancer: a pooled study of seven prospective cohorts. Cancer Causes Control. 2010; https://doi.org/10.1007/s10552-010-9558-x.
Tang H, Wei P, Duell EJ, Risch HA, Olson SH, Bueno-de-Mesquita HB, et al. Genes-environment interactions in obesity- and diabetes-associated pancreatic cancer: a GWAS data analysis. Cancer Epidemiol Biomark Prev. 2014;23(1):98–106. https://doi.org/10.1158/1055-9965.EPI-13-0437-T.
Rebours V, Gaujoux S, d'Assignies G, Sauvanet A, Ruszniewski P, Levy P, et al. Obesity and fatty pancreatic infiltration are risk factors for pancreatic precancerous lesions (PanIN). Clin Cancer Res. 2015; https://doi.org/10.1158/1078-0432.CCR-14-2385.
Pinho AV, Chantrill L, Rooman I. Chronic pancreatitis: a path to pancreatic cancer. Cancer Lett. 2014;345(2):203–9. https://doi.org/10.1016/j.canlet.2013.08.015.
Zambirinis CP, Pushalkar S, Saxena D, Miller G. Pancreatic cancer, inflammation and microbiome. Cancer J (Sudbury, Mass). 2014;20(3):195–202. https://doi.org/10.1097/PPO.0000000000000045.
Zheng W, McLaughlin JK, Gridley G, Bjelke E, Schuman LM, Silverman DT, et al. A cohort study of smoking, alcohol consumption, and dietary factors for pancreatic cancer (United States). Cancer Causes Control : CCC. 1993;4(5):477–82. https://doi.org/10.1007/BF00050867.
Gold EB, Gordis L, Diener MD, Seltser R, Boitnott JK, Bynum TE, et al. Diet and other risk factors for cancer of the pancreas. Cancer. 1985;55(2):460–7. https://doi.org/10.1002/1097-0142(19850115)55:2<460::AID-CNCR2820550229>3.0.CO;2-V.
Falk RT, Pickle LW, Fontham ET, Correa P, Fraumeni JF, Jr. Life-style risk factors for pancreatic cancer in Louisiana: a case-control study. Am J Epidemiol. 1988;128(2):324–36.
Raimondi S, Maisonneuve P, Lowenfels A. Epidemiology of pancreatic cancer: an overview. Nat Rev Gastroenterol Hepatol. 2009;6(12):699–708. https://doi.org/10.1038/nrgastro.2009.177.
Lowenfels A, Maisonneuve P. Risk factors for pancreatic cancer. J Cell Biochem. 2005;95(4):649–56. https://doi.org/10.1002/jcb.20461.
Shen QW, Yao QY. Total fat consumption and pancreatic cancer risk: a meta-analysis of epidemiologic studies. Eur J Cancer Prev: Off J Eur Cancer Prev Organ. 2014; https://doi.org/10.1097/CEJ.0000000000000073.
Andreotti G, Silverman DT. Occupational risk factors and pancreatic cancer: a review of recent findings. Mol Carcinog. 2012;51(1):98–108.
Chen C, Xun P, Nishijo M, Sekikawa A, He K. Cadmium exposure and risk of pancreatic cancer: a meta-analysis of prospective cohort studies and case–control studies among individuals without occupational exposure history. Environ Sci Pollut Res. 2015;22(22):17465–74. https://doi.org/10.1007/s11356-015-5464-9.
Behrens G, Jochem C, Schmid D, Keimling M, Ricci C, Leitzmann MF. Physical activity and risk of pancreatic cancer: a systematic review and meta-analysis. Eur J Epidemiol. 2015;30(4):279–98. https://doi.org/10.1007/s10654-015-0014-9.
Farrell JJ, Zhang L, Zhou H, Chia D, Elashoff D, Akin D, et al. Variations of oral microbiota are associated with pancreatic diseases including pancreatic cancer. Gut. 2012;61(4):582–8. https://doi.org/10.1136/gutjnl-2011-300784.
Jandhyala SM, Madhulika A, Deepika G, Rao GV, Reddy DN, Subramanyam C, et al. Altered intestinal microbiota in patients with chronic pancreatitis: implications in diabetes and metabolic abnormalities. Sci Rep. 2017;7:43640. https://doi.org/10.1038/srep43640.
Huang XIN, Li X, Ma Q, Xu Q, Duan W, Lei J, et al. Chronic alcohol exposure exacerbates inflammation and triggers pancreatic acinar-to-ductal metaplasia through PI3K/Akt/IKK. Int J Mol Med. 2015;35(3):653–63. https://doi.org/10.3892/ijmm.2014.2055.
Zanet E, Berretta M, Di Benedetto F, Talamini R, Ballarin R, Nunnari G, et al. Pancreatic cancer in HIV-positive patients: a clinical case-control study. Pancreas. 2012;41(8):1331–5.
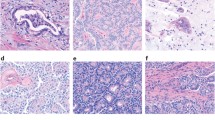
Brosens LA, Hackeng WM, Offerhaus GJ, Hruban RH, Wood LD. Pancreatic adenocarcinoma pathology: changing “landcape”. J Gastrointest Oncol. 2015;6(4):358–74. https://doi.org/10.3978/j.issn.2078-6891.2015.032.
Knudsen ES, Balaji U, Mannakee B, Vail P, Eslinger C, Moxom C, et al. Pancreatic cancer cell lines as patient-derived avatars: genetic characterisation and functional utility. Gut. 2017; https://doi.org/10.1136/gutjnl-2016-313133.
Macgregor-Das A, Iacobuzio-Donahue C. Molecular pathways in pancreatic carcinogenesis. J Surg Oncol. 2013;107(1):8–14. https://doi.org/10.1002/jso.23213.
Srivastava SK, Arora S, Singh S, Bhardwaj A, Averett C, Singh AP. MicroRNAs in pancreatic malignancy: progress and promises. Cancer Lett. 2014;347(2):167–74. https://doi.org/10.1016/j.canlet.2014.02.015.
Feig C, Gopinathan A, Neesse A, Chan DS, Cook N, Tuveson DA. The pancreas cancer microenvironment. Clin Cancer Res. 2012;18(16):4266–76. https://doi.org/10.1158/1078-0432.CCR-11-3114.
Watari N, Hotta Y, Mabuchi Y. Morphological studies on a vitamin A-storing cell and its complex with macrophage observed in mouse pancreatic tissues following excess vitamin A administration. Okajimas Folia Anat Jpn. 1982;58(4–6):837–58.
Haqq J, Howells LM, Garcea G, Metcalfe MS, Steward WP, Dennison AR. Pancreatic stellate cells and pancreas cancer: current perspectives and future strategies. Eur J Cancer. 2014;50(15):2570–82. https://doi.org/10.1016/j.ejca.2014.06.021.
• Pothula SP, Xu Z, Goldstein D, Pirola RC, Wilson JS, Apte MV. Key role of pancreatic stellate cells in pancreatic cancer. Cancer Lett. 2016;381(1):194–200. https://doi.org/10.1016/j.canlet.2015.10.035. This review outlines the multiple roles and functions of PSCs in pancreatic cancer tumorigenesis, progression, and metastasis.
Collins MA, Bednar F, Zhang YQ, Brisset JC, Galban S, Galban CJ, et al. Oncogenic Kras is required for both the initiation and maintenance of pancreatic cancer in mice. J Clin Investig. 2012;122(2):639–53. https://doi.org/10.1172/Jci59227.
Erkan M, Hausmann S, Michalski CW, Fingerle AA, Dobritz M, Kleeff J, et al. The role of stroma in pancreatic cancer: diagnostic and therapeutic implications. Nat Rev Gastroenterol Hepatol. 2012;9(8):454–67.
Jakubowska MA, Ferdek PE, Gerasimenko OV, Gerasimenko JV, Petersen OH. Nitric oxide signals are interlinked with calcium signals in normal pancreatic stellate cells upon oxidative stress and inflammation. Open Biol. 2016;6(8).
Apte M, Pirola RC, Wilson JS. Pancreatic stellate cell: physiologic role, role in fibrosis and cancer. Curr Opin Gastroenterol. 2015;31(5):416–23. https://doi.org/10.1097/MOG.0000000000000196.
Carr RM, Fernandez-Zapico ME. Pancreatic cancer microenvironment, to target or not to target? EMBO Mol Med. 2016;8(2):80–2.
Ozdemir BC, Pentcheva-Hoang T, Carstens JL, Zheng X, Wu CC, Simpson TR, et al. Depletion of carcinoma-associated fibroblasts and fibrosis induces immunosuppression and accelerates pancreas cancer with reduced survival. Cancer Cell. 2014;25(6):719–34. https://doi.org/10.1016/j.ccr.2014.04.005.
Rhim AD, Oberstein PE, Thomas DH, Mirek ET, Palermo CF, Sastra SA et al. Stromal elements act to restrain, rather than support, pancreatic ductal adenocarcinoma. Cancer Cell. 2014;25(6):735–47. doi:https://doi.org/10.1016/j.ccr.2014.04.021.
Katt ME, Placone AL, Wong AD, Xu ZS, Searson PC. In vitro tumor models: advantages, disadvantages, variables, and selecting the right platform. Front Bioeng Biotechnol. 2016;4:12. https://doi.org/10.3389/fbioe.2016.00012.
Logsdon CD, Arumugam T, Ramachandran V. The difficulty of animal modeling of pancreatic cancer for preclinical evaluation of therapeutics. Am J Physiol Gastrointest Liver Physiol. 2015; https://doi.org/10.1152/ajpgi.00169.2015.
Boj SF, Hwang CI, Baker LA, Chio II, Engle DD, Corbo V, et al. Organoid models of human and mouse ductal pancreatic cancer. Cell. 2015;160(1–2):324–38. https://doi.org/10.1016/j.cell.2014.12.021.
Unger F, Bentz S, Kruger J, Rosenbrock C, Schaller J, Pursche K, et al. Precision cut cancer tissue slices in anti-cancer drug testing. J Mol Pathophysiol. 2015;4(3):108. https://doi.org/10.5455/jmp.20151023055556.
• Albritton JL, Miller JS. 3D bioprinting: improving in vitro models of metastasis with heterogeneous tumor microenvironments. Dis Model Mech. 2017;10(1):3–14. https://doi.org/10.1242/dmm.025049. This review discusses the advancements made in 3D bioprinting and its beneficial use in studying tumor microenvironment using in vitro methods.
Weidenhofer J, Colvin E, Bond D, Scarlett C. Animal models of pancreatic cancer and their application in clinical research. Gastrointest Cancer: Targets Ther. 2016;6:31–9. https://doi.org/10.2147/gictt.s84531.
Ponz-Sarvise M, Tuveson DA, Yu KH. Mouse models of pancreatic ductal adenocarcinoma. Hematol Oncol Clin North Am. 2015;29(4):609–17. https://doi.org/10.1016/j.hoc.2015.04.010.
McIntyre CA, Winter JM. Diagnostic evaluation and staging of pancreatic ductal adenocarcinoma. Semin Oncol. 2015;42(1):19–27. https://doi.org/10.1053/j.seminoncol.2014.12.003.
Chang JC, Kundranda M. Novel diagnostic and predictive biomarkers in pancreatic adenocarcinoma. Int J Mol Sci. 2017;18(3):667.
O’Donoghue AJ, Ivry SL, Chaudhury C, Hostetter DR, Hanahan D, Craik CS. Procathepsin E is highly abundant but minimally active in pancreatic ductal adenocarcinoma tumors. Biol Chem. 2016;397(9):871–81.
Lines KE, Chelala C, Dmitrovic B, Wijesuriya N, Kocher HM, Marshall JF, et al. S100P-binding protein, S100PBP, mediates adhesion through regulation of cathepsin Z in pancreatic cancer cells. Am J Pathol. 2012;180(4):1485–94.
Melo SA, Luecke LB, Kahlert C, Fernandez AF, Gammon ST, Kaye J, et al. Glypican-1 identifies cancer exosomes and detects early pancreatic cancer. Nature. 2015;523(7559):177–82. https://doi.org/10.1038/nature14581. http://www.nature.com/nature/journal/v523/n7559/abs/nature14581.html#supplementary-information
Sogawa K, Takano S, Iida F, Satoh M, Tsuchida S, Kawashima Y, et al. Identification of a novel serum biomarker for pancreatic cancer, C4b-binding protein [alpha]-chain (C4BPA) by quantitative proteomic analysis using tandem mass tags. Br J Cancer. 2016;115(8):949–56. https://doi.org/10.1038/bjc.2016.295.
Hadano N, Murakami Y, Uemura K, Hashimoto Y, Kondo N, Nakagawa N, et al. Prognostic value of circulating tumour DNA in patients undergoing curative resection for pancreatic cancer. Br J Cancer. 2016;115(1):59–65. https://doi.org/10.1038/bjc.2016.175.
Kaur S, Smith LM, Patel A, Menning M, Watley DC, Malik SS, et al. A combination of MUC5AC and CA19-9 improves the diagnosis of pancreatic cancer: a multicenter study. Am J Gastroenterol. 2017;112(1):172–83. https://doi.org/10.1038/ajg.2016.482.
Poruk KE, Firpo MA, Scaife CL, Adler DG, Emerson LL, Boucher KM, et al. Serum osteopontin and TIMP-1 as diagnostic and prognostic biomarkers for pancreatic adenocarcinoma. Pancreas. 2013;42(2):193–7. https://doi.org/10.1097/MPA.0b013e31825e354d.
Sun L, Burnett J, Guo C, Xie Y, Pan J, Yang Z, et al. CPA4 is a promising diagnostic serum biomarker for pancreatic cancer. Am J Cancer Res. 2016;6(1):91–6.
Fukutake N, Ueno M, Hiraoka N, Shimada K, Shiraishi K, Saruki N, et al. A novel multivariate index for pancreatic cancer detection based on the plasma free amino acid profile. PLoS One. 2015;10(7):e0132223. https://doi.org/10.1371/journal.pone.0132223.
Radon TP, Massat NJ, Jones R, Alrawashdeh W, Dumartin L, Ennis D, et al. Identification of a three-biomarker panel in urine for early detection of pancreatic adenocarcinoma. Clin Cancer Res. 2015;21(15):3512.
Suker M, Beumer BR, Sadot E, Marthey L, Faris JE, Mellon EA, et al. FOLFIRINOX for locally advanced pancreatic cancer: a systematic review and patient-level meta-analysis. Lancet Oncol. 2016;17(6):801–10. https://doi.org/10.1016/S1470-2045(16)00172-8.
Yardley DA. nab-Paclitaxel mechanisms of action and delivery. J Control Release. 2013;170(3):365–72. https://doi.org/10.1016/j.jconrel.2013.05.041.
Von Hoff D, Ervin T, Arena F, Chiorean E, Infante J, Moore M, et al. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med. 2013;369(18):1691–703. https://doi.org/10.1056/NEJMoa1304369.
Alvarez R, Musteanu M, Garcia-Garcia E, Lopez-Casas PP, Megias D, Guerra C, et al. Stromal disrupting effects of nab-paclitaxel in pancreatic cancer. Br J Cancer. 2013;109(4):926–33. https://doi.org/10.1038/bjc.2013.415.
Abbruzzese JL, Grunewald R, Weeks EA, Gravel D, Adams T, Nowak B, et al. A phase I clinical, plasma, and cellular pharmacology study of gemcitabine. J Clin Oncol. 1991;9(3):491–8. https://doi.org/10.1200/JCO.1991.9.3.491.
Burris HA, Moore MJ, Andersen J, Green MR, Rothenberg ML, Modiano MR, et al. Improvements in survival and clinical benefit with gemcitabine as first-line therapy for patients with advanced pancreas cancer: a randomized trial. J Clin Oncol. 1997;15(6):2403–13. https://doi.org/10.1200/JCO.1997.15.6.2403.
Vickers MM, Powell ED, Asmis TR, Jonker DJ, Hilton JF, O’Callaghan CJ, et al. Comorbidity, age and overall survival in patients with advanced pancreatic cancer—results from NCIC CTG PA.3: a phase III trial of gemcitabine plus erlotinib or placebo. Eur J Cancer. 2012;48(10):1434–42. https://doi.org/10.1016/j.ejca.2011.10.035.
Moore M, Goldstein D, Hamm J, Figer A, Hecht J, Gallinger S, et al. Erlotinib plus gemcitabine compared with gemcitabine alone in patients with advanced pancreatic cancer: a phase III trial of the National Cancer Institute of Canada Clinical Trials Group. J Clin Oncol: Off J Am Soc Clin Oncol. 2007;25(15):1960–6. https://doi.org/10.1200/JCO.2006.07.9525.
• Goldstein D, El-Maraghi RH, Hammel P, Heinemann V, Kunzmann V, Sastre J, et al. nab-Paclitaxel plus gemcitabine for metastatic pancreatic cancer: long-term survival from a phase III trial. JNCI: J Natl Cancer Inst. 2015;107(2):dju413–dju. https://doi.org/10.1093/jnci/dju413. This study demonstrated the ability of the nab -paclitaxel/gemcitabine combination therapy to significantly increase the median survival of pancreatic cancer patients when compared to gemcitabine monotherapy. Median survivals were 8.5 months for the nab -paclitaxel/gemcitabine combination and 6.7 months for gemcitabine monotherapy.
Bachmann J, Michalski CW, Martignoni ME, Buchler MW, Friess H. Pancreatic resection for pancreatic cancer. HPB (Oxford). 2006;8(5):346–51. https://doi.org/10.1080/13651820600803981.
Paulson A, Tran Cao H, Tempero M, Lowy A. Therapeutic advances in pancreatic cancer. Gastroenterology. 2013;144(6):1316–26. https://doi.org/10.1053/j.gastro.2013.01.078.
Garrido-Laguna I, Hidalgo M. Pancreatic cancer: from state-of-the-art treatments to promising novel therapies. Nat Rev Clin Oncol. 2015;12(6):319–34. https://doi.org/10.1038/nrclinonc.2015.53.
Singh D, Upadhyay G, Srivastava RK, Shankar S. Recent advances in pancreatic cancer: biology, treatment, and prevention. Biochim Biophys Acta. 2015;1856(1):13–27. https://doi.org/10.1016/j.bbcan.2015.04.003.
Dhillon N, Aggarwal BB, Newman RA, Wolff RA, Kunnumakkara AB, Abbruzzese JL, et al. Phase II trial of curcumin in patients with advanced pancreatic cancer. Clin Cancer Res : Off J Am Assoc Cancer Res. 2008;14(14):4491–9. https://doi.org/10.1158/1078-0432.ccr-08-0024.
Kanai M, Yoshimura K, Asada M, Imaizumi A, Suzuki C, Matsumoto S, et al. A phase I/II study of gemcitabine-based chemotherapy plus curcumin for patients with gemcitabine-resistant pancreatic cancer. Cancer Chemother Pharmacol. 2010;68(1):157–64. https://doi.org/10.1007/s00280-010-1470-2.
Epelbaum R, Schaffer M, Vizel B, Badmaev V, Bar-Sela G. Curcumin and gemcitabine in patients with advanced pancreatic cancer. Nutr Cancer. 2010;62(8):1137–41. https://doi.org/10.1080/01635581.2010.513802.
Morimoto T, Sunagawa Y, Katanasaka Y, Hirano S, Namiki M, Watanabe Y, et al. Drinkable preparation of Theracurmin exhibits high absorption efficiency—a single-dose, double-blind, 4-way crossover study. Biol Pharm Bull. 2013;36(11):1708–14.
Kanai M, Otsuka Y, Otsuka K, Sato M, Nishimura T, Mori Y, et al. A phase I study investigating the safety and pharmacokinetics of highly bioavailable curcumin (Theracurmin(A ®)) in cancer patients. Cancer Chemother Pharmacol. 2013;71(6):1521–30. https://doi.org/10.1007/s00280-013-2151-8.
Shankar S, Nall D, Tang SN, Meeker D, Passarini J, Sharma J, et al. Resveratrol inhibits pancreatic cancer stem cell characteristics in human and KrasG12D transgenic mice by inhibiting pluripotency maintaining factors and epithelial-mesenchymal transition. PLoS One. 2011;6(1):e16530. https://doi.org/10.1371/journal.pone.0016530.
Pramanik KC, Srivastava SK. Apoptosis signal-regulating kinase 1–thioredoxin complex dissociation by capsaicin causes pancreatic tumor growth suppression by inducing apoptosis. Antioxid Redox Signal. 2012;17(10):1417–32. https://doi.org/10.1089/ars.2011.4369.
El-Rayes BF, Philip PA, Sarkar FH, Shields AF, Ferris AM, Hess K, et al. A phase II study of isoflavones, erlotinib, and gemcitabine in advanced pancreatic cancer. Investig New Drugs. 2011;29(4):694–9. https://doi.org/10.1007/s10637-010-9386-6.
Vendrely V, Peuchant E, Buscail E, Moranvillier I, Rousseau B, Bedel A, et al. Resveratrol and capsaicin used together as food complements reduce tumor growth and rescue full efficiency of low dose gemcitabine in a pancreatic cancer model. Cancer Lett. 2017;390:91–102. https://doi.org/10.1016/j.canlet.2017.01.002.
Appari M, Babu KR, Kaczorowski A, Gross W, Herr I. Sulforaphane, quercetin and catechins complement each other in elimination of advanced pancreatic cancer by miR-let-7 induction and K-ras inhibition. Int J Oncol. 2014;45(4):1391–400.
Shankar S, Marsh L, Srivastava RK. EGCG inhibits growth of human pancreatic tumors orthotopically implanted in Balb C nude mice through modulation of FKHRL1/FOXO3a and neuropilin. Mol Cell Biochem. 2013;372(1):83–94. https://doi.org/10.1007/s11010-012-1448-y.
Gong J, Muñoz AR, Chan D, Ghosh R, Kumar AP. Stat3 down regulates LC3 to inhibit autophagy and pancreatic cancer cell growth: role of NexrutineR. Oncotarget. 2014;5(9):2529–41.
Gong J, Xie J, Bedolla R, Rivas P, Chakravarthy D, Freeman J, et al. Combined targeting of STAT3/NF-κB/COX-2/EP4 for effective management of pancreatic cancer. Clin Cancer Res. 2014;20(5):1259–73. https://doi.org/10.1158/1078-0432.CCR-13-1664.
Gong J, Muñoz AR, Pingali S, Payton-Stewart F, Chan DE, Freeman JW, et al. Downregulation of STAT3/NF-κB potentiates gemcitabine activity in pancreatic cancer cells. Mol Carcinog. 2017;56(2):402–11. https://doi.org/10.1002/mc.22503.
Forster T, Rausch V, Zhang Y, Isayev O, Heilmann K, Schoensiegel F, et al. Sulforaphane counteracts aggressiveness of pancreatic cancer driven by dysregulated Cx43-mediated gap junctional intercellular communication. Oncotarget. 2014;5(6):1621–34.
Li Y, Karagöz GE, Seo YH, Zhang T, Jiang Y, Yu Y, et al. Sulforaphane inhibits pancreatic cancer through disrupting Hsp90-p50(Cdc37) complex and direct interactions with amino acids residues of Hsp90. J Nutr Biochem. 2012;23(12):1617–26. https://doi.org/10.1016/j.jnutbio.2011.11.004.
Subramani R, Gonzalez E, Arumugam A, Nandy S, Gonzalez V, Medel J, et al. Nimbolide inhibits pancreatic cancer growth and metastasis through ROS-mediated apoptosis and inhibition of epithelial-to-mesenchymal transition. Sci Rep. 2016;6:19819. https://doi.org/10.1038/srep19819.
Funding
We acknowledge support provided by the CTRC at UTHSA through the NCI support grant no. 2P30 CA 054174-17 (APK) and the CTRC 40th Anniversary Distinguished Professor of Oncology Endowment (APK). This work was supported in part by the funds from Veterans Affairs-Merit Award I01 BX 000766-01 and BX003876; National Center for Complementary and Alternate Medicine 1R01 AT007448 (APK) and National Cancer Institute R01 CA 149516 (RG).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This review article contains no animal or human studies performed by any of the authors.
Additional information
This article is part of the Topical Collection on Cancer Chemoprevention
Rights and permissions
About this article
Cite this article
Muñoz, A.R., Chakravarthy, D., Gong, J. et al. Pancreatic Cancer: Current Status and Challenges. Curr Pharmacol Rep 3, 396–408 (2017). https://doi.org/10.1007/s40495-017-0112-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40495-017-0112-3