Abstract
Introduction
Little is known about the frequency and nature of medication errors (MEs) and adverse drug events (ADEs) that occur in mental health hospitals.
Objectives
This systematic review aims to provide an up-to-date and critical appraisal of the epidemiology and nature of MEs and ADEs in this setting.
Method
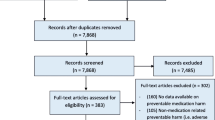
Ten electronic databases were searched, including MEDLINE, Embase, CINAHL, International Pharmaceutical Abstracts, PsycINFO, Scopus, British Nursing Index, ASSIA, Web of Science, and Cochrane Database of Systematic Reviews (1999 to October 2016). Studies that examined the rate of MEs or ADEs in mental health hospitals were included, and quality appraisal of the included studies was conducted.
Result
In total, 20 studies were identified. The rate of MEs ranged from 10.6 to 17.5 per 1000 patient-days (n = 2) and of ADEs from 10.0 to 42.0 per 1000 patient-days (n = 2) with 13.0–17.3% of ADEs found to be preventable. ADEs were rated as clinically significant (66.0–71.0%), serious (28.0–31.0%), or life threatening (1.4–2.0%). Prescribing errors occurred in 4.5–6.3% of newly written or omitted prescription items (n = 3); dispensing errors occurred in 4.6% of opportunities for error (n = 1) and in 8.8% of patients (n = 1); and medication administration errors occurred in 3.3–48.0% of opportunities for error (n = 5). MEs and ADEs were frequently associated with psychotropics, with atypical antipsychotic drugs commonly involved. Variability in study setting and data collection methods limited direct comparisons between studies.
Conclusion
Medication errors occur frequently in mental health hospitals and are associated with risk of patient harm. Effective interventions are needed to target these events and improve patient safety.

Similar content being viewed by others
References
World Health Organization. World alliance for patient safety. Geneva: WHO; 2005. http://www.who.int/patientsafety/en/brochure_final.pdf. Accessed 15 April 2016.
De Vries EN, Ramrattan MA, Smorenburg SM, Gouma DJ, Boermeester MA. The incidence and nature of in-hospital adverse events: a systematic review. Qual Saf Health Care. 2008;17(3):216–23.
Lewis PJ, Dornan T, Taylor D, Tully MP, Wass V, Ashcroft DM. Prevalence, incidence and nature of prescribing errors in hospital inpatients. Drug Saf. 2009;32(5):379–89.
Keers RN, Williams SD, Cooke J, Ashcroft DM. Prevalence and nature of medication administration errors in health care settings: a systematic review of direct observational evidence. Ann Pharmacother. 2013;47(2):237–56.
James KL, Barlow D, McArtney R, Hiom S, Roberts D, Whittlesea C. Incidence, type and causes of dispensing errors: a review of the literature. Int J Pharm Pract. 2009;17(1):9–30.
Hert M, Correll CU, Bobes J, Cetkovich-Bakmas M, Cohen D, Asai I, et al. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry. 2011;10(1):52–77.
Hert M, Cohen D, Bobes J, Marcelo CB, Leucht S, Ndetei DM, et al. Physical illness in patients with severe mental disorders. II. Barriers to care, monitoring and treatment guidelines, plus recommendations at the system and individual level. World Psychiatry. 2011;10(2):138–51.
Procyshyn RM, Barr AM, Brickell T, Honer WG. Medication errors in psychiatry: a comprehensive review. CNS Drugs. 2010;24(7):595–609.
Latoo J, Mistry M, Dunne FJ. Physical morbidity and mortality in people with mental illness. Br J Med Pract. 2013;6(3):621–3.
Kane JM, Kishimoto T, Correll CU. Non-adherence to medication in patients with psychotic disorders: epidemiology, contributing factors and management strategies. World Psychiatry. 2013;12(3):216–26.
Chapman SC, Horne R. Medication nonadherence and psychiatry. Curr Opin Psychiatry. 2013;26(5):446–52.
The National Archives. Mental Health Act 2007. http://www.legislation.gov.uk/ukpga/2007/12/contents. Accessed 1 Feb 2017.
Newcomer JW. Metabolic considerations in the use of antipsychotic medications: a review of recent evidence. J Clin Psychiatry. 2007;68(1):20–7.
Teixeira PJR, Rocha FL. The prevalence of metabolic syndrome among psychiatric inpatients in Brazil. Revista Brasileira de Psiquiatria. 2007;29(4):330–6.
Kukreja S, Kalra G, Shah N, Shrivastava A. Polypharmacy in psychiatry: a review. Mens Sana Monographs. 2013;11(1):82–99.
Centorrino F, Goren JL, Hennen J, Salvatore P, Kelleher JP, Baldessarini RJ. Multiple versus single antipsychotic agents for hospitalized psychiatric patients: case–control study of risks versus benefits. Am J Psychiatr. 2004;161(4):700–6.
Lelliott P, Paton C, Harrington M, Konsolaki M, Sensky T, Okocha C. The influence of patient variables on polypharmacy and combined high dose of antipsychotic drugs prescribed for in-patients. Psychiatrist. 2002;26(11):411–4.
Sinclair LI, Davies SJ, Parton G, Potokar JP. Drug–drug interactions in general hospital and psychiatric hospital in-patients prescribed psychotropic medications. Int J Psychiatry Clin Pract. 2010;14(3):212–9.
Maidment ID, Lelliott P, Paton C. Medication errors in mental healthcare: a systematic review. Qual Saf Health Care. 2006;15(6):409–13.
Maidment ID, Haw C, Stubbs J, Fox C, Katona C, Franklin BD. Medication errors in older people with mental health problems: a review. Int J Geriatr Psychiatry. 2008;23(6):564–73.
Grasso BC, Rothschild JM, Genest R, Bates DW. What do we know about medication errors in inpatient psychiatry? Joint Comm J Qual Saf. 2003;29(8):391–400.
Keers RN, Williams SD, Vattakatuchery JJ, Brown P, Miller J, Prescott L, et al. Prevalence, nature and predictors of prescribing errors in mental health hospitals: a prospective multicentre study. BMJ Open. 2014;4(9):e006084.
Keers RN, Williams SD, Vattakatuchery JJ, Brown P, Miller J, Prescott L, et al. Medication safety at the interface: evaluating risks associated with discharge prescriptions from mental health hospitals. J Clin Pharm Ther. 2015;40(6):645–54.
Cottney A. Improving the safety and efficiency of nurse medication rounds through the introduction of an automated dispensing cabinet. BMJ Qual Improve Rep. 2014;3(1):u204237–w1843.
Cottney A, Innes J. Medication administration errors in an urban mental health hospital: a direct observation study. Int J Ment Health Nurs. 2015;24(1):65–74.
Ito H, Yamazumi S. Common types of medication errors on long-term psychiatric care units. Int J Qual Health Care. 2003;15(3):207–12.
Haw CM, Dickens G, Stubbs J. A review of medication administration errors reported in a large psychiatric hospital in the United Kingdom. Psychiatr Serv. 2005;56(12):1610–3.
Meyer-Massetti C, Cheng CM, Schwappach DL, Paulsen L, Ide B, Meier CR, et al. Systematic review of medication safety assessment methods. Am J Health Syst Pharm. 2011;68(3):227–40.
Bates DW, Cullen DJ, Laird N, et al. Incidence of adverse drug events and potential adverse drug events: implications for prevention. JAMA. 1995;274(1):29–34.
Bates DW, Miller EB, Cullen DJ, Burdick L, Williams L, Laird N, et al. Patient risk factors for adverse drug events in hospitalized patients. Arch Intern Med. 1999;159(21):2553–60.
National Coordinating Council for Medication Error Reporting and Prevention. About medication errors: what is a medication error. 2015. http://www.nccmerp.org/aboutMedErrors. Accessed 2 Feb 2016.
Mueller SK, Sponsler KC, Kripalani S, Schnipper JL. Hospital-based medication reconciliation practices: a systematic review. Arch Intern Med. 2012;172(14):1057–69.
Kohn LT, Corrigan JM, Donaldson MS. To err is human: building a safer health system. Washington, D.C: National Academies Press; 1999.
Stelfox HT, Palmisani S, Scurlock C, Orav EJ, Bates DW. The “To Err is Human” report and the patient safety literature. Qual Saf Health Care. 2006;15(3):174–8.
Buetow SA, Sibbald B, Cantrill JA, Halliwell S. Prevalence of potentially inappropriate long term prescribing in general practice in the United Kingdom, 1980–95: systematic literature review. BMJ. 1996;313(7069):1371–4.
Allan E, Barker K. Fundamentals of medication error research. Am J Health Syst Pharm. 1990;47(3):555–71.
Ghaleb MA, Barber N, Franklin BD, Yeung VW, Khaki ZF, Wong IC. Systematic review of medication errors in pediatric patients. Ann Pharmacother. 2006;40(10):1766–76.
Alsulami Z, Conroy S, Choonara I. Medication errors in the Middle East countries: a systematic review of the literature. Eur J Clin Pharmacol. 2013;69(4):995–1008.
McLeod MC, Barber N, Franklin BD. Methodological variations and their effects on reported medication administration error rates. BMJ Qual Saf. 2013;22(4):278–89.
Grasso BC, Genest R, Jordan CW, Bates DW. Use of chart and record reviews to detect medication errors in a state psychiatric hospital. Psychiatr Serv. 2003;54(5):677–81.
Sørensen AL, Lisby M, Nielsen LP, Poulsen BK, Mainz J. The medication process in a psychiatric hospital: are errors a potential threat to patient safety? Risk Manag Healthc Pol. 2013;2013(6):23–31.
Rothschild JM, Mann K, Keohane CA, Williams DH, Foskett C, Rosen SL, et al. Medication safety in a psychiatric hospital. Gen Hosp Psychiatry. 2007;29(2):156–62.
Sirithongthavorn S, Narkpongphun A, Kamduang N, Isarapongs P, Kanjanarat P. Common types of medication errors of outpatient service in pediatric psychiatry care. Pharmacoepidemiol Drug Saf. 2009;18(S1):S245–6.
Ayani N, Sakuma M, Morimoto T, Kikuchi T, Watanabe K, Narumoto J, et al. The epidemiology of adverse drug events and medication errors among psychiatric inpatients in Japan: the JADE study. BMC Psychiatry. 2016;16(1):303.
Hema K, Mohammad I, Manoranjani Reddy J, Nandha Kishore G, Ramesh M, Sebastian J. Assessment of medication errors in psychiatry practice in a tertiary care hospital. Int J Pharm Sci Res. 2015;6(1):226–32.
Scott H, Brown D, Herreraa H. Prevalence and nature of prescribing errors in a mental health setting: analysis of preliminary data from a prospective study. Int J Pharm Pract. 2016;3:8–13.
Haw C, Stubbs J. Prescribing errors at a psychiatric hospital. Pharm Pract. 2003;13(2):64–6.
Grasso BC, Genest R, Yung K, Arnold C. Reducing errors in discharge medication lists by using personal digital assistants. Psychiatr Serv. 2002;53(10):1325–6.
Stubbs J, Haw C, Taylor D. Prescription errors in psychiatry—a multi-centre study. J Psychopharmacol. 2006;20(4):553–61.
Jhanjee A, Bhatia M, Oberoi A, Srivastava S. Medication errors in psychiatric practice—a cross-sectional Study. Delhi Psychiatry J. 2012;15(1):5–13.
Shawahna R, Rahman N. Prescribing errors in psychiatry department: an audit from a hospital in Lahore. J Pak Psychiatr Soc. 2008;5:31–3.
Nirodi P, Mitchell A. The quality of psychotropic drug prescribing in patients in psychiatric units for the elderly. Aging Ment Health. 2002;6(2):191–6.
Brownlie K, Schneider C, Culliford R, Fox C, Boukouvalas A, Willan C, et al. Medication reconciliation by a pharmacy technician in a mental health assessment unit. Int J Clin Pharm. 2014;36(2):303–9.
Abduldaeem H, Masters K, Patel N, Donyai P. A direct observation study of medication administration errors in a mental health inpatient setting. Int J Pharm Pract. 2016;24(1):4–15.
Haw C, Stubbs J, Dickens G. An observational study of medication administration errors in old-age psychiatric inpatients. Int J Qual Health Care. 2007;19(4):210–6.
Dean B, Barber N, Schachter M. What is a prescribing error? Qual Health Care. 2000;9(4):232–7.
Lisby M, Nielsen LP, Mainz J. Errors in the medication process: frequency, type, and potential clinical consequences. Int J Qual Health Care 2005;17(1):15–22.
Morimoto T, Sakuma M, Matsui K, Kuramoto N, Toshiro J, Murakami J. Incidence of adverse drug events and medication errors in Japan: the JADE study. J Gen Intern Med. 2011;26(2):148–153.
Aljadhey H, Mahmoud MA, Ahmed Y, Sultana R, Zouein S, Alshanawani S, et al. Incidence of adverse drug events in public and private hospitals in Riyadh, Saudi Arabia: the (ADESA) prospective cohort study. BMJ Open. 2016;6(7):e010831.
Hug BL, Witkowski DJ, Sox CM, Keohane CA, Seger DL, Yoon C, et al. Adverse drug event rates in six community hospitals and the potential impact of computerized physician order entry for prevention. J Gen Intern Med. 2010;25(1):31–8.
Barker KN, Flynn EA, Pepper GA, et al. Medication errors observed in 36 health care facilities. Arch Intern Med. 2002;162:1897–903. doi:10.1001/archinte.162.16.1897.
Dean B, Barber N. Validity and reliability of observational methods for studying medication administration errors. Am J Health Syst Pharm. 2001;58(1):54–9.
Bourgeois FT, Shannon MW, Valim C, Mandl KD. Adverse drug events in the outpatient setting: an 11-year national analysis. Pharmacoepidemiol Drug Saf. 2010;19(9):901–10.
Thomsen LA, Winterstein AG, Søndergaard B, Haugbølle LS, Melander A. Systematic review of the incidence and characteristics of preventable adverse drug events in ambulatory care. Ann Pharmacother. 2007;41(9):1411–26.
Taché SV, Sönnichsen A, Ashcroft DM. Prevalence of adverse drug events in ambulatory care: a systematic review. Ann Pharmacother. 2011;45(7–8):977–89.
Morcos S, Francis S-A, Duggan C. Where are the weakest links? A descriptive study of discrepancies in prescribing between primary and secondary sectors of mental health service provision. Psychiatrist. 2002;26(10):371–4.
Nelson LA, Graham MR, Schaefer MG. Characterization of medication discrepancies occurring at the time of discharge from a state psychiatric inpatient facility. Hosp Pharm. 2011;46(4):254–61.
National Mental Health Development Unit. Getting the medicines right 2: medicines management in mental health crisis resolution and home treatment teams. 2010. http://www.crisiscareconcordat.org.uk/wp-content/uploads/2015/07/Getting-the-Medicines-Right-2.pdf Accessed 10 Sept 2016.
The Joint Commission . National patient safety goals. 2015. http://www.jointcommission.org/assets/1/6/2015_NPSG_HAP.pdf. Accessed 10 Sept 2016.
Lizer MH, Brackbill ML. Medication history reconciliation by pharmacists in an inpatient behavioral health unit. Am J Health Syst Pharm. 2007;64:1087–91.
Paton C, McIntyre S, Bhatti SF, Shingleton-Smith A, Gray R, Gerrett D, et al. Medicines reconciliation on admission to inpatient psychiatric care: findings from a UK quality improvement programme. Ther Adv Psychopharmacol. 2011;1(4):101–10.
Kothari M, Maidment I, Lyon R, Haygarth L. Medicines reconciliation in comparison with NICE guidelines across secondary care mental health organisations. Int J Clin Pharm. 2016;38(2):289–95.
Jayaram G, Doyle D, Steinwachs D, Samuels J. Identifying and reducing medication errors in psychiatry: creating a culture of safety through the use of an adverse event reporting mechanism. J Psychiatr Pract. 2011;17(2):81–8.
Keers RN, Williams SD, Cooke J, Ashcroft DM. Causes of medication administration errors in hospitals: a systematic review of quantitative and qualitative evidence. Drug Saf. 2013;36(11):1045–67.
Tully MP, Ashcroft DM, Dornan T, Lewis PJ, Taylor D, Wass V. The causes of and factors associated with prescribing errors in hospital inpatients. Drug Saf. 2009;32(10):819–36.
Neale G, Woloshynowych M, Vincent C. Exploring the causes of adverse events in NHS hospital practice. J R Soc Med. 2001;94(7):322–30.
Keers R, Placido M, Bennett K, Clayton K, Brown P, Ashcroft D. Understanding the causes of medication administration errors in a mental health hospital using qualitative interviews with the critical incident technique. Pharmacoepidemiol Drug Saf. 2016;25:3–23. doi:10.1002/pds.4019.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Ghadah H. Alshehri gratefully acknowledges the Princess Nora Bint Abdul Rahman University for funding her PhD programme at the University of Manchester.
Conflict of interest
Ghadah H. Alshehri, Richard N. Keers and Darren M. Ashcroft have no conflicts of interest that are directly relevant to the content of this study.
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Alshehri, G.H., Keers, R.N. & Ashcroft, D.M. Frequency and Nature of Medication Errors and Adverse Drug Events in Mental Health Hospitals: a Systematic Review. Drug Saf 40, 871–886 (2017). https://doi.org/10.1007/s40264-017-0557-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-017-0557-7