Abstract
Introduction
Different definitions of breakthrough pain (BTP) influence the observed BTP prevalence. This study examined BTP prevalence variability due to use of different cutoffs for controlled background pain, different assessment periods for background pain, and difference between worst and average pain intensity (PI).
Methods
Cancer patients from the EPCRC-CSA study who reported flare-ups of pain past 24 h were potential BTP cases. BTP prevalence was calculated for different cutoffs for background PI on numeric rating scales (NRS 0–10) for the past week, past 48 and past 24 h period. Furthermore, BTP cases were categorized based on the difference between maximum and average PI past 24 h (range, 0 to > 2 points, NRS 0–10).
Results
Of 696 respondents, 302 patients (43.4%) reported pain flares the past 24 h. The BTP prevalence when using a defined background PI ≤ 4 for the past week was 19.8%. This number varied for different defined cutoffs for background PI. Actual background PI and BTP prevalence also varied between the assessment periods “past week”, “past 48 h”, and “past 24 h” (PI 4.0, 3.6, and 3.4; BTP prevalence 19.8, 22.7, and 24.9% for background PI ≤ 4). For patients with background PI ≤ 4 past week, 105 had a difference between maximum and average PI ≥ one point and 48 had a difference > two points.
Conclusions
The reported BTP prevalence is dependent on the cutoff for background PI in the BTP definition, population background PI during the assessment period, and defined cutoff for the difference between worst and average PI.
Funding
NTNU, Norwegian University of Science and Technology.
Similar content being viewed by others
Introduction
The prevalence range in breakthrough pain (BTP) literature is wide [1]. Variability in diagnostic criteria and inclusion of patients with poorly controlled background pain may contribute to this feature [1]. The definition of BTP includes an adequately controlled and stable background pain [2, 3]. In addition, the patient must have transient exacerbations of pain, which are pain flares well distinguished from the background pain [2,3,4,5]. Despite international agreement on these basic characteristics, controversies about the definition of BTP continue in clinical as well as in research settings [6]. Differences in definitional criteria complicate both the clinical diagnosis and the comparison of epidemiological data between studies [6]. Within the scope of defining BTP according to characteristics that are universally understood and measurable [6], the current study explores consequences of definitional variability.
Background pain of moderate intensity or less was a criterion in the pioneer definition [5]. In more recent literature, adequately controlled background pain is defined as “mild”, or specified as ≤ 4 on the 11-point numeric rating scale (NRS 0–10) [2, 4]. Furthermore, BTP prevalence has been reported for patients with background PI ≤ 6 (NRS 0–10) [7]. Pain flares are also described in cancer patients with uncontrolled background pain [7, 8]. It has been argued that narrow criteria for background pain intensity (PI) may result in the exclusion of clinically important pain flares [6]. How the prevalence of BTP varies with the defined cutoff for background PI has not been studied in detail.
The assessment period for background pain was originally defined as the past 24 h [5]. In a follow-up paper, the assessment period for background pain was changed to the previous week [9], an approach adopted in current BTP literature [2,3,4, 10]. The different recall periods for background pain have been compared [11, 12], showing a high correlation between PI for a 24-h and 7-day recall period [13]. The potential consequences for the BTP prevalence caused by different assessment periods for background pain have not been reported.
The magnitude of the pain flare was originally defined as a transitory increase in pain to greater than moderate intensity, which occurred on a background pain of moderate intensity or less [5]. Since then, extensive work has been undertaken to identify meaningful cutoffs for PI and relevant measures of changes in PI [14,15,16,17,18,19]. Different interpretations exist for the necessary size of a transient pain exacerbation in cancer patients in order to classify it as a significant pain flare [3, 16, 20, 21]. In a recently published study by Mercadante et al. [3], a difference of one point or more (NRS 0–10) between breakthrough PI and background PI was accepted as a significant transient increase in PI. Mercadante et al. also suggested a PI ≥ 7 (NRS 0–10) as a meaningful cutoff for BTP medication, aiming for a PI ≤ 4 (NRS 0–10) after treatment [16]. In a Delphi study including expert opinions from researchers within the field of BTP, the panel agreed with the statement that the increase in PI has to be more than two points on an NRS scale (0–10) for a transient cancer pain exacerbation to be clinically significant [20].
The EPCRC-CSA study included cancer patients whose pain was evaluated by several self-reported assessment methods [22], providing an opportunity to address the research question: How is the assessed BTP prevalence affected by different definitions for cutoffs for controlled background PI, assessment periods for background pain, and cutoffs for the difference between worst and average PI past 24 h?
Methods
Study Design and Patient Population
The EPCRC-CSA (Trial registration: ClinicalTrials.gov identifier, NCT00972634) is a cross-sectional observational international study conducted in 17 centers within eight countries in 2008 and 2009 [22]. Adult patients with incurable cancer and able to complete a computer-based symptom assessment were eligible. Patients who rated their worst PI ≥ 1 (NRS 0–10) for the previous 24 h, were subject to further pain assessment and included in the present study, which is a secondary analysis of a study originally designed to assess the feasibility of computer-based symptom assessment [22].
Measurement Tools and Data Collection
The measurements used in the secondary analysis included: (I) A simplified item from the Alberta Breakthrough Pain Assessment Tool (ABPAT) [23], where all patients with worst PI ≥ 1 (NRS 0–10) for the past 24 h were introduced to the concept of BTP as characterized in the ABPAT instructions [23]. They were then presented with the question: “Have you had flare-ups of BTP in the last 24 h?” (Yes/No). (II) Elements from the Brief Pain Inventory (BPI), which is a widely used assessment tool for pain where each PI scale ranges from 0 (no pain) to 10 (pain as bad as you can imagine) [24]. BPI questions on worst PI past 24 h and past week were supplemented with questions on worst PI past 48 h, and average PI specified for the time periods “past 24 h”, “past 48 h”, and “past week”. All data were collected electronically and obtained the same day.
Terminology and Statistical Analysis
Average pain was used as a measurement for background pain and, unless stated otherwise, with the assessment period “past week” [2]. Patients answering “yes” to the ABPAT-based BTP screening question were classified as “ABPAT+”. The ABPAT-positive patients were grouped according to background PI past week, and the cumulative percentages of ABPAT-positive patients within each potential level of maximal background PI were computed. Subsequently, the procedure was repeated for the assessment periods for background pain “past 48 h” and past “24 h”. Kappa statistic was used to compare agreement beyond chance between the cumulative percentages of ABPAT-positive patients with background pain ≤ 4 (NRS 0–10) for the three different assessment periods for background pain. Kappa values 0.61–0.80 indicate substantial agreement, and kappa values 0.81–1.0 indicate almost perfect agreement [25]. Finally, the ABPAT-positive patients grouped according to background PI past week were further categorized based on the difference between reported worst and average PI past 24 h. The chosen categories were: A difference of at least one point, a difference of at least two points, and a difference of more than two points (NRS 0–10) between worst and average PI past 24 h. Hypothetical BTP prevalences were calculated from percentages of ABPAT-positive patients satisfying specified criteria for background PI and difference between worst and average PI past 24 h.
Compliance with Ethics Statement
This article is based on a previously conducted study. All procedures performed in the primary study were in accordance with the ethics committees at the respective study sites and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the primary study.
Results
Participant Characteristics
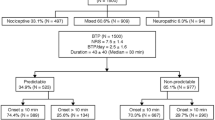
Among 1017 patients included in the EPCRC-CSA study, 715 persons reported worst PI ≥ 1 (NRS 0–10) past 24 h. Patient-reported BTP registrations according to the ABPAT-based screening question, and average PI registrations for the three assessment periods “past week”, “past 48 h”, and “past 24 h” were available for 696 patients. Essential patient characteristics for the 696 patients included in the present analysis are displayed in Table 1.
Prevalence of self-reported flare-ups of pain in the past 24 h related to the level of background PI, the assessment period for background pain, and the difference between worst and average PI
Three hundred and two out of 696 patients (43.4%) who answered the APBAT-based screening question reported flare-ups of BTP for the past 24 h and were classified as “ABPAT +”. The distributions of background PI for ABPAT-positive patients are displayed in Fig. 1 for the three assessment periods “past week”, “past 48 h”, and “past 24 h”. The mean (median) average PI scores for the assessment periods “past week”, “past 48 h”, and “past 24 h” were 4.0 (4.0), 3.6 (3.0), and 3.4 (3.0) (NRS 0–10), respectively. Figure 1 illustrates that a large proportion of the ABPAT-positive patients had uncontrolled background pain.
Distribution of background pain intensitya in ABPAT-positiveb patients. aBackground pain intensity assessed for the three time periods “past week”, “past 48 h”, and “past 24 h”. bPatients answering “yes” to the Alberta Breakthrough Pain Assessment Tool (ABPAT)-based breakthrough pain screening question were classified as ABPAT-positive
Defining a cutoff for background PI ≤ 3 (NRS 0–10) in ABPAT-positive patients resulted in a BTP prevalence of 14.9%. The corresponding number for a defined cutoff for background PI ≤ 4 was 19.8% (Table 2). Table 2 shows the cumulative percentage of ABPAT-positive patients in relation to each score for background pain, resulting in increased BTP prevalence when including patients with higher background PI.
The cumulative percentages of ABPAT-positive patients related to background PI scores are displayed in Fig. 2 for the different assessment periods for background pain “past week”, “past 48 h, and “past 24 h”. As indicated in the figure, differences between the assessments periods result in variable percentages of patients meeting the requirements for having BTP. For instance, compared to a 19.8% BTP prevalence using background PI ≤ 4 (NRS 0–10) assessed for the past week, the corresponding percentages were 22.7 using background PI the past 48 h (93% agreement, kappa 0.80), and 24.9 using background PI the past 24 h (92% agreement, kappa 0.76).
ABPAT-positivea prevalence variabilityb related to different assessment periods for background pain intensityc. aPatients answering “yes” to the Alberta Breakthrough Pain Assessment Tool (ABPAT)-based breakthrough pain screening question were classified as ABPAT-positive. bABPAT-positive prevalence variability related to different assessment periods for background pain indicated for a cutoff for background pain intensity ≤ 4 (NRS 0–10). cBackground pain intensity assessed for the three time periods “past week”, “past 48 h”, and “past 24 h”. Mean pain intensity for the three assessment periods were 4.0, 3.6, and 3.4 (NRS 0–10), respectively. All calculations include the cumulative percentages of patients with the respective background pain intensity or less
As illustrated in Fig. 3, among ABPAT-positive patients, the difference between worst and average PI past 24 h ranged from zero to more than two points (NRS 0–10). Defining a minimum difference between worst and average PI past 24 h of one point and background PI ≤ 4 (past week), resulted in a BTP prevalence of 15.1%. Using the same definition for background PI, but with a minimum difference of two points between worst and average PI, resulted in a BTP prevalence of 9.5%. Figure 3 illustrates a BTP prevalence variability related to difference between worst and average PI past 24 h ranging from 6.9% (48 out of 696 patients) to 19.8% (138 out of 696 patients), using the same definition for background pain (PI ≤ 4 past week). In addition, Fig. 3 illustrates that 60 of the ABPAT-positive patients reported no difference between worst and average PI past 24 h.
ABPAT-positivea prevalence variabilityb related to difference between worst and average pain intensityc. aPatients answering “yes” to the Alberta Breakthrough Pain Assessment Tool (ABPAT) based breakthrough pain screening question were classified as ABPAT-positive. bABPAT-positive prevalence variability related to difference between worst and average pain intensity past 24 h, indicated for a difference of at least one point and a difference of more than two points, and a cutoff for background pain intensity ≤ 4 (NRS 0–10). cDifference between worst and average pain intensity for the past 24 h, displayed for the differences: ≥ 0 points, ≥ 1 point, ≥ 2 points, and > 2 points (NRS 0–10). dBackground pain intensity assessed for time period “past week”. All calculations include the cumulative percentages of patients with the respective background pain intensity or less
Discussion
BTP prevalence estimates, defined as proportions of ABPAT-positive patients, were dependent on both the cutoff for controlled background pain and the population background PI during the assessment period for background pain. The prevalence estimates were approximately doubled if assessed without including controlled background pain as a criterion. Different cutoff criteria for a necessary numeric difference between worst and average PI also had a substantial impact on the assessed BTP prevalence.
Appraisal of Methods
Uncontrolled background pain should be treated before assessing BTP [2]. For the purpose of this analysis, the diagnosis of BTP was based on a screening question of pain flares, and afterwards the prevalence was calculated according to reported background PI. Without the intention of presenting precise prevalence estimates, but merely to demonstrate the effect of background PI when assessing BTP, this procedure was found acceptable.
Despite the demonstrated reliability and validity of recalled pain measures as used in the present study, these registrations are still prone to recall bias and/or actual variations in PI [12, 13]. With 58% being in-patients and 42% of the patients still on chemotherapy, the observed lower background PI for the past 1 and 2 days compared to past week might represent a treatment effect increasing the proportion of patients with controlled background pain. For matters of stringency, the assessment periods for background pain and BTP should ideally be concurrent.
To get a precise measurement of the magnitude of a transient exacerbation of pain, as a minimum, PI before and during the painful episode is needed. Without this information at hand, worst and average PI recollected from the same period as the pain flare occurred may provide proxy knowledge on the size of PI fluctuations. Still, background PI before an episode of BTP may not be equivalent to average pain, and peak PI during the flare-up of pain may be different from patient-reported worst pain.
The screening question for BTP used in the primary study assessed the past 24 h [22]. Patients with BTP, but not experiencing any pain flares within this period were not included. Nor did the study specifically examine whether the pain flares were cancer related. However, the majority of the patients believed the cancer caused their pain (Table 1). Finally, average PI was used as a measure for background pain. The approach may open for interpretations, but the method has been used in both older and more recent studies [7, 9].
Comparison with Previous Work
Besides prevalence variations related to disease stage and symptom burden, the identification of BTP depends on the characteristics used to define BTP [1, 6]. The primary publication from the EPCRC-CSA study indicated that more than 40% of the patients had BTP last 24 h [22]. In a follow-up paper on the same study population, which demonstrated a nation-based range in prevalence from 14 to 75%, the authors emphasized the point that research on BTP has been challenged by a lack of consensus on standard language and taxonomy [26]. A commentary on the follow-up paper implied that many of the patients with a pain flare might have uncontrolled background pain, a claim confirmed in the present analysis [27].
Patients with BTP are reported to have more intense background pain [9]. This seems reasonable considering that the transient exacerbations of pain increase the average pain, reflecting all variations in PI [1]. In line with this, previous studies have shown higher prevalence of transient exacerbations of pain when including patients regardless of background PI compared to a subgroup of the patient population with an average background PI of ≤ 6 or ≤ 4 (NRS 0–10), respectively [7, 28]. The present study supported these findings, and explored the implications of different intensity levels for background pain. Usually, no more than mild background PI is accepted as a prerequisite for diagnosing BTP [2]. Different cutoffs are applied for distinguishing mild from moderate pain, and a systematic review on symptoms included in the Edmonton Symptom Assessment Scale found NRS scores 1–4 best reflecting mild pain [17, 18, 29, 30]. As shown in Table 2, by raising the accepted level of maximum background PI by one point from 3 to 4 (NRS 0–10), the calculated BTP prevalence will increase from 15% to almost 20%.
Choice of recall periods for patient-reported outcomes should depend on the specific purpose of the trial, the characteristics of the disease, and the treatment to be tested [13]. Recalled average pain from the past 48 h has been shown to be a reliable and valid measure of actual pain in cancer patients [12]. The present study demonstrated a high degree of agreement beyond chance for prevalence estimates when changing the assessment period for background pain from “past week” to “past “48 h”, supporting that possibility when appropriate due to trial purposes. In addition, there was substantial agreement between the prevalence estimates for BTP when changing the assessment period for background pain from “past week” to “past 24 h”. However, despite this agreement, Fig. 2 illustrates a change in BTP prevalence from 19.8 to 24.9% for different assessment periods for background pain (background PI ≤ 4), reliant on the distribution (Fig. 1) and central tendency measure (average PI) of the background pain [31].
A transient pain exacerbation can be assessed as an increase in absolute score, an increase to a predefined score, or as a proportion of increase on a numeric rating scale, with different degree of support in favor of the various views [14, 20]. For raw numerical scores, a commonly cited clinically important difference in PI is two points (NRS 0–10) [14]. A large study exploring the responsiveness of the Edmonton Symptom Assessment Scale in cancer patients concluded that the optimal cutoff for improvement and deterioration was one point or more (NRS 0–10) for each of the ten symptoms, pain included [19]. The discussion in the aftermath of the study pointed out that although being a useful measure for power calculations and response determinations in trials, for the individual patient additional measures like personalized symptom goals may be useful [32,33,34]. The present study indicated that to predefine the necessary size of a transient pain exacerbation might add stringency to a study design. Interestingly, approximately 20% of the patients who reported pain flares the past 24 h also reported no difference between worst and average PI for the same period. Lack of clarity and misunderstandings may represent challenges when interpreting patient-reported questionnaires, and can result in information bias and systematic errors in study results [23, 35].
The present study supports previous findings and underlines that valid comparisons of prevalence and treatment effects are dependent on standardized and universally agreed upon criteria for BTP [6, 7, 28].
Limitations
The current study is based on a 10-year-old data set. Pain prevalence and pain control may have changed during the following years [36]. However, a recent study found no improvement in cancer pain management in a 5-year perspective from 2008 [37]. Furthermore, the study population is patients with advanced cancer, limiting the generalizability of the conclusions.
Conclusions
The study underlined that BTP prevalence assessment needs to be standardized [6]. To reduce inter-study variability, both the numerically defined cutoff for controlled background PI and the actual background PI in the population should be reported. The necessary increase in PI for a transient pain exacerbation to be considered significant also should be stated, as this may have a substantial impact on the prevalence. However, the present study did not aim to identify the optimal definition of BTP, but simply addressed that variable use of BTP definitions will result in variable prevalence estimates. Lack of definition consensus makes it difficult to know to what extent differences between studies are due to the use of different BTP definitions or reflect actual differences in clinical pain experienced by the patients. Further international collaboration to improve standardization in assessment and reporting of BTP should be prioritized.
The present study also demonstrated that pain flares outside the definition of BTP is frequent, and hence must be accounted for in inclusion and exclusion criteria in research and addressed in clinical practice [20]. Finally, the study demonstrated that PI assessments that reflect the most recent changes in pain medication are applicable.
Due to the methodology of this study, which is based on a 10-year-old dataset, the findings should be studied prospectively and with a controlled design investigating a broader spectrum of pain characteristics and patient populations. Whether broad or narrow diagnostic criteria for BTP influence the number of treatment interventions, patients’ pain reports and treatment satisfaction should also be addressed.
References
Deandrea S, Corli O, Consonni D, Villani W, Greco MT, Apolone G. Prevalence of breakthrough cancer pain: a systematic review and a pooled analysis of published literature. J Pain Symptom Manag. 2014;47(1):57–76.
Davies AN, Dickman A, Reid C, Stevens AM, Zeppetella G. The management of cancer-related breakthrough pain: recommendations of a task group of the Science Committee of the Association for Palliative Medicine of Great Britain and Ireland. Eur J Pain. 2009;13(4):331–8.
Mercadante S, Marchetti P, Cuomo A, Caraceni A, Mediati RD, Mammucari M, et al. Breakthrough cancer pain: preliminary data of the Italian Oncologic Pain Multisetting Multicentric Survey (IOPS-MS). Adv Ther. 2017;34(1):120–35.
Mercadante S, Lazzari M, Reale C, Cuomo A, Fusco F, Marchetti P, et al. Italian Oncological Pain Survey (IOPS): a multicentre Italian study of breakthrough pain performed in different settings. Clin J Pain. 2015;31(3):214–21.
Portenoy RK, Hagen NA. Breakthrough pain: definition, prevalence and characteristics. Pain. 1990;41(3):273–81.
Mercadante S, Portenoy RK. Breakthrough cancer pain: twenty-five years of study. Pain. 2016;157(12):2657–63.
Caraceni A, Bertetto O, Labianca R, Maltoni M, Mercadante S, Varrassi G, et al. Episodic (breakthrough) pain prevalence in a population of cancer pain patients. Comparison of clinical diagnoses with the QUDEI—Italian questionnaire for intense episodic pain. J Pain Symptom Manag. 2012;43(5):833–41.
Gatti A, Gentili M, Baciarello M, Lazzari M, Marzi R, Palombo E, et al. Breakthrough pain in patients with controlled or uncontrolled basal pain: an observational study. Pain Res Manag J Can Pain Soc journal de la societe canadienne pour le traitement de la douleur. 2014;19(6):e168–71.
Portenoy RK, Payne D, Jacobsen P. Breakthrough pain: characteristics and impact in patients with cancer pain. Pain. 1999;81(1–2):129–34.
Davies A, Buchanan A, Zeppetella G, Porta-Sales J, Likar R, Weismayr W, et al. Breakthrough cancer pain: an observational study of 1000 European oncology patients. J Pain Symptom Manag. 2013;46(5):619–28.
Shi Q, Wang XS, Mendoza TR, Pandya KJ, Cleeland CS. Assessing persistent cancer pain: a comparison of current pain ratings and pain recalled from the past week. J Pain Symptom Manag. 2009;37(2):168–74.
Jensen MP, Wang W, Potts SL, Gould EM. Reliability and validity of individual and composite recall pain measures in patients with cancer. Pain Med. 2012;13(10):1284–91.
Shi Q, Trask PC, Wang XS, Mendoza TR, Apraku WA, Malekifar M, et al. Does recall period have an effect on cancer patients’ ratings of the severity of multiple symptoms? J Pain Symptom Manag. 2010;40(2):191–9.
Farrar JT, Portenoy RK, Berlin JA, Kinman JL, Strom BL. Defining the clinically important difference in pain outcome measures. Pain. 2000;88(3):287–94.
Farrar JT, Polomano RC, Berlin JA, Strom BL. A comparison of change in the 0–10 numeric rating scale to a pain relief scale and global medication performance scale in a short-term clinical trial of breakthrough pain intensity. Anesthesiology. 2010;112(6):1464–72.
Mercadante S, Adile C, Torta R, Varetto A, Fulfaro F, Giarratano A, et al. Meaningful cut-off pain intensity for breakthrough pain changes in advanced cancer patients. Curr Med Res Opin. 2013;29(1):93–7.
Oldenmenger WH, de Raaf PJ, de Klerk C, van der Rijt CC. Cut points on 0–10 numeric rating scales for symptoms included in the Edmonton Symptom Assessment Scale in cancer patients: a systematic review. J Pain Symptom Manag. 2013;45(6):1083–93.
Serlin RC, Mendoza TR, Nakamura Y, Edwards KR, Cleeland CS. When is cancer pain mild, moderate or severe—grading pain severity by its interference with function. Pain. 1995;61(2):277–84.
Hui D, Shamieh O, Paiva CE, Perez-Cruz PE, Kwon JH, Muckaden MA, et al. Minimal clinically important differences in the Edmonton Symptom Assessment Scale in cancer patients: a prospective, multicenter study. Cancer. 2015;121(17):3027–35.
Lohre ET, Klepstad P, Bennett MI, Brunelli C, Caraceni A, Fainsinger RL, et al. From “breakthrough” to “episodic” cancer pain? A European Association for palliative care research network expert Delphi survey toward a common terminology and classification of transient cancer pain exacerbations. J Pain Symptom Manag. 2016;51(6):1013–9.
Mercadante S, Marchetti P, Cuomo A, Mammucari M, Caraceni A, IOPS MS Study Group. Breakthrough pain and its treatment: critical review and recommendations of IOPS (Italian Oncologic Pain Survey) expert group. Support Care Cancer. 2016;24(2):961–8.
Hjermstad MJ, Lie HC, Caraceni A, Currow DC, Fainsinger RL, Gundersen OE, et al. Computer-based symptom assessment is feasible in patients with advanced cancer: results from an international multicenter study, the EPCRC-CSA. J Pain Symptom Manag. 2012;44(5):639–54.
Hagen NA, Stiles C, Nekolaichuk C, Biondo P, Carlson LE, Fisher K, et al. The Alberta Breakthrough Pain Assessment Tool for cancer patients: a validation study using a Delphi process and patient think-aloud interviews. J Pain Symptom Manag. 2008;35(2):136–52.
Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singap. 1994;23(2):129–38.
McGinn T, Wyer PC, Newman TB, Keitz S, Leipzig R, Guyatt G, The Evidence-Based Medicine Teaching Tips Working Group. Tips for learners of evidence-based medicine: 3. Measures of observer variability (kappa statistic). CMAJ. 2004;171(11):1369–73. https://doi.org/10.1503/cmaj.1031981.
Hjermstad MJ, Kaasa S, Caraceni A, Loge JH, Pedersen T, Haugen DF, et al. Characteristics of breakthrough cancer pain and its influence on quality of life in an international cohort of patients with cancer. BMJ Support Palliat Care. 2016;6(3):344–52.
Davies A, Dickman A, Farquhar-Smith P, Webber K, Zeppetella J. Letter to the Editor re ‘Characteristics of breakthrough cancer pain and its influence on quality of life in an international cohort of patients with cancer (BMJ Support Palliat Care 2016;6:344–52)’. BMJ Support Palliat Care. 2017;7(3):264.
Valeberg BT, Miaskowski C, Hanestad BR, Bjordal K, Paul S, Rustoen T. Demographic, clinical, and pain characteristics are associated with average pain severity groups in a sample of oncology outpatients. J Pain. 2008;9(10):873–82.
Fainsinger RL, Fairchild A, Nekolaichuk C, Lawlor P, Lowe S, Hanson J. Is pain intensity a predictor of the complexity of cancer pain management? J Clin Oncol. 2009;27(4):585–90.
Fainsinger RL, Nekolaichuk C, Lawlor P, Hagen N, Bercovitch M, Fisch M, et al. An international multicentre validation study of a pain classification system for cancer patients. Eur J Cancer. 2010;46(16):2896–904.
Cardinal LJ. Central tendency and variability in biological systems. J Community Hosp Intern Med Perspect. 2015;5(3):27930.
Johnson MJ, Currow DC. Minimal clinically important difference and Edmonton Symptom Assessment Scale. Cancer. 2016;122(1):158–9.
Hui D, Bruera E. Reply to minimal clinically important difference and Edmonton Symptom Assessment Scale. Cancer. 2016;122(1):159–60.
Hui D, Bruera E. The Edmonton symptom assessment system 25 years later: past, present, and future developments. J Pain Symptom Manag. 2017;53(3):630–43.
Tripepi G, Jager KJ, Dekker FW, Zoccali C. Selection bias and information bias in clinical research. Nephron Clin Pract. 2010;115(2):c94–9.
Greco MT, Roberto A, Corli O, Deandrea S, Bandieri E, Cavuto S, et al. Quality of cancer pain management: an update of a systematic review of undertreatment of patients with cancer. J Clin Oncol. 2014;32(36):4149–54.
Thronaes M, Raj SX, Brunelli C, Almberg SS, Vagnildhaug OM, Bruheim S, et al. Is it possible to detect an improvement in cancer pain management? A comparison of two Norwegian cross-sectional studies conducted 5 years apart. Support Care Cancer. 2016;24(6):2565–74.
Acknowledgements
We thank the participants of the primary study.
Funding
The study is sponsored by NTNU, Norwegian University of Science and Technology. Article processing charges are covered by a publication fund organized by the sponsor. All authors had full access to all of the data in the study and take complete responsibility for the integrity of the data and accuracy of the data analysis.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Erik T. Løhre, Marianne J. Hjermstad, Cinzia Brunelli, Anne K. Knudsen and Pål Klepstad have nothing to disclose. Stein Kaasa is one of the shareholders in Eir Solutions A/S. He declares no income, dividend or financial benefits from the work presented here.
Compliance with Ethics Guidelines
This article is based on a previously conducted study. All procedures performed in the primary study were in accordance with the ethics committees at the respective study sites and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the primary study.
Data Availability
The dataset generated and analyzed during the current study is available from the corresponding author on reasonable request.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced digital features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.7246817.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Løhre, E.T., Hjermstad, M.J., Brunelli, C. et al. Pain Intensity Factors Changing Breakthrough Pain Prevalence in Patients with Advanced Cancer: A Secondary Analysis of a Cross-Sectional Observational International Study. Pain Ther 7, 193–203 (2018). https://doi.org/10.1007/s40122-018-0107-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-018-0107-8