Abstract
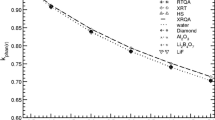
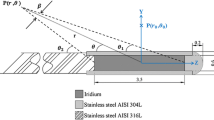
The use of a non-water-equivalent personalised mould for gynaecological brachytherapy treatments can result in a substantial dose reduction at the treatment site, compared to calculated dose, in lieu of a dose calculation algorithm capable of modelling non-water-equivalent materials. This study describes the characterisation of the radiological properties of a brachytherapy applicator moulding material. Simple line source correction factors for an 192Ir source are obtained through Monte Carlo simulations and verified by film measurements. The dwell position corrections are used to estimate aggregate correction factors for dose deliveries that involve multiple dwell positions, in terms of treatment length, applicator radii and depth of reference dose. For the Fricotan moulding material used locally, the dose reductions varied from 1% for an applicator radius of 0.5 cm to > 4% for radii exceeding 2 cm. The method described in this paper could be used to develop correction factors for other non-water-equivalent moulding materials, in a TG-43UI dose calculation environment.


Similar content being viewed by others
References
Nag S, Erickson B, Parikh S, Gupta N, Varia M, Glasgow G (2000) American Brachytherapy Society: The American Brachytherapy Society recommendations for high-dose-rate brachytherapy for carcinoma of the endometrium. Int J Radiat Oncol Biol Phys 48(3):779–790
Small W Jr, Beriwal S, Demanes DJ, Dusenbery KE, Eifel P, Erickson B, Jones E, Rownd JJ, De Los Sangos JF, Viswanathan AN, Gaffney D (2012) American Brachytherapy Society consensus guidelines for adjuvant vaginal cuff brachytherapy after hysterectomy. Brachytherapy 11(1):58–67
Bertoni F, Bertoni G, Bignardi M (1983) Vaginal molds for intracavitary curietherapy: a new method of preparation. Int J Radiat Oncol Biol Phys 9(10):1579–1582
Albano M, Dumas I, Haie-Meder C (2008) Brachytherapy at the Institut Gustave-Roussy: personalized vaginal mould applicator: technical modification and improvement. Cancer Radiother 12(8):822–826
Nilsson S, Moutrie Z, Cheuk R, Chan P, Lancaster C, Markwell T, Dawes J, Back P (2015) A unique approach to high-dose-rate vaginal mold brachytherapy of gynecologic malignancies. Brachytherapy 14(2):267–272
Rivard MJ, Coursey BM, DeWerd LA, Hanson WF, Saiful Huq M, Ibbott GS, Mitch MG, Nath R, Williamson JF (2004) Update of AAPM Task Group No. 43 Report: a revised AAPM protocol for brachytherapy dose calculations. Med Phys 31(3):633–674
Beaulieu L, Carlsson Tedgren Å, Carrier JF, Davis SD, Mourtada F, Rivard MJ, Thomson RM, Verhaegen F, Wareing TA, Williamson JF (2012) Report of the Task Group 186 on model-based dose calculation methods in brachytherapy beyond the TG-43 formalism: current status and recommendations for clinical implementation. Med Phys 39(10):6208–6236
Hill R, Brown S, Baldock C (2008) Evaluation of the water equivalence of solid phantoms using gamma ray transmission measurements. Radiat Meas 43(7):1258–1264
Hill R, Kuncic Z, Baldock C (2010) The water equivalence of solid phantoms for low energy photon beams. Med Phys 37(8):4355–4363
Yu PC, Chao TC, Lee CC, Wu CJ, Tung CJ (2010) A Monte Carlo dosimetry study using Henschke applicator for cervical brachytherapy. Nucl Instrum Methods Phys Res A 619(1):411–414
Taylor REP, Rogers DWO (2008) EGSnrc monte carlo calculated dosimetry parameters for 192Ir and 169Yb brachytherapy sources. Med Phys 35(11):4933–4944
Daskalov GM, Loffler E, Williamson JF (1998) Monte Carlo-aided dosimetry of a new high dose-rate brachytherapy source. Med Phys 25(11):2200–2208
Ubrich F, Wulff J, Engenhart-Cabillic R, Zink K (2014) Correction factors for source strength determination in HDR brachytherapy using the in-phantom method. Zeitschrift für Medizinische Physik 24(2):138–152
Poludniowski G, Landry G, DeBlois F, Evans P, Verhaegen F (2009) SpekCalc: a program to calculate photon spectra from tungsten anode X-ray tubes. Phys Med Biol 54(19):N433
Peet SC, Wilks R, Kairn T, Trapp JV, Crowe SB (2016) Calibrating radiochromic film in beams of uncertain quality. Med Phys 43(10):5647–5652
Aland T, Kairn T, Kenny J (2011) Evaluation of a Gafchromic EBT2 film dosimetry system for radiotherapy quality assurance. Australas Phys Eng Sci Med 34(2):251–260
Fonseca GP, Antunes PC, Reniers B, Yoriyaz H, Verhaegen F (2013) A brachytherapy model-based dose calculation algorithm-AMIGOBrachy. In: International Nuclear Atlantic Conference - INAC, Recife
Zourari K, Pantelis E, Moutsatsos A, Sakelliou L, Georgiou E, Karaiskos P, Papagiannis P (2013) Dosimetric accuracy of a deterministic radiation transport based 192Ir brachytherapy treatment planning system. Part III. Comparison to monte carlo simulation in voxelized anatomical computational models. Med Phys 40(1):011712
Pantelis E, Peppa V, Lahanas V, Pappas E, Papagiannis P (2015) BrachyGuide: a brachytherapy-dedicated dicom rt viewer and interface to monte carlo simulation software. J Appl Clin Med Phys 16(1):208–218
Chamberland M, Taylor R, Rogers D, Thomson R (2016) TU-AB-BRC-08: Egs_brachy, a fast and versatile monte carlo code for brachytherapy applications. Med Phys 43(6):3731–3731
Acknowledgements
The authors wish to thank the Queensland University of Technology’s Central Analytical Research Facility, particularly Charlotte Allen, for their assistance in characterising the composition of the Fricotan material. The authors also wish to thank staff involved with the brachytherapy program at the Royal Brisbane & Women’s Hospital, Queensland, Australia.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare they have no conflicts of interest.
Research involving human and animal participants
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Crowe, S.B., Pross, Z., Nilsson, S. et al. Characterisation of radiological properties of a brachytherapy moulding material. Australas Phys Eng Sci Med 41, 731–737 (2018). https://doi.org/10.1007/s13246-018-0673-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13246-018-0673-4