Abstract
Purpose
Hemodilutional anemia is associated with acute kidney injury (AKI) and mortality in patients undergoing cardiac surgery by mechanisms that may include tissue hypoxia. Our hypothesis was to assess if changes in the potential hypoxic biomarkers, including methemoglobin and erythropoietin, correlated with a decrease in hemoglobin (Hb) concentration following hemodilution on cardiopulmonary bypass (CPB).
Methods
Arterial blood samples were taken from patients (n = 64) undergoing heart surgery and CPB at baseline, during CPB, following CPB, and in the intensive care unit (ICU). Potential hypoxic biomarkers were measured, including methemoglobin, plasma Hb, and erythropoietin. Data were analyzed by repeated measures one-way analysis of variance on ranks and linear regression.
Results
Hemoglobin levels decreased following CPB and methemoglobin increased in the ICU (P < 0.001 for both). No correlation was observed between the change in Hb and methemoglobin (P = 0.23). By contrast, reduced Hb on CPB correlated with increased lactate, reduced pH, and increased erythropoietin levels following CPB (P ≤ 0.004 for all). Increased plasma Hb (P < 0.001) also correlated with plasma erythropoietin levels (P < 0.001).
Conclusion
These data support the hypothesis that erythropoietin rather than methemoglobin is a potential biomarker of anemia-induced tissue hypoxia. The observed relationships between decreased Hb during CPB and the increase in lactate, reduced pH, and increase in erythropoietin levels suggest that early changes in plasma erythropoietin may be a pragmatic early biomarker of anemia-induced renal hypoxia. Further study is required to determine if anemia-induced increases in erythropoietin may predict AKI in patients undergoing cardiac surgery.
Trial registration
www.clinicaltrials.gov (NCT01883713). Registered 21 June 2013.
Résumé
Objectif
L’anémie par hémodilution est associée à des lésions rénales aiguës (LRA) et à la mortalité des patients subissant une chirurgie cardiaque par des mécanismes qui pourraient inclure l’hypoxie tissulaire. Notre hypothèse consistait à évaluer si les modifications de biomarqueurs potentiels de l’hypoxie, incluant la méthémoglobine et l’érythropoïétine, étaient corrélées à une baisse de la concentration en hémoglobine (Hb) après hémodilution au cours d’une circulation extracorporelle (CEC).
Méthodes
Des échantillons de sang artériel ont été prélevés chez des patients (n = 64) subissant une chirurgie cardiaque et une CEC au début de la chirurgie, au cours de la CEC et après la CEC en unité de soins intensifs (USI). Les biomarqueurs potentiels de l’hypoxie ont été mesurés, notamment la méthémoglobine, l’hémoglobine plasmatique et l’érythropoïétine. Les données ont été analysées par des mesures répétées de la variance à un facteur sur des régressions des rangs et linéaires.
Résultats
Les taux d’hémoglobine ont diminué après la CEC et la méthémoglobine a augmenté pendant le séjour à l’USI (P < 0,001 pour les deux). Aucune corrélation n’a été trouvée entre la variation de l’hémoglobine et celle de la méthémoglobine (P = 0,23). En revanche, la baisse de l’hémoglobine sous CEC a été corrélée à une augmentation des lactates, une baisse du pH et une augmentation des taux d’érythropoïétine après la CEC (P ≤ 0,004 pour tous). L’augmentation de l’hémoglobine plasmatique (P < 0,001) a aussi été corrélée aux taux d’érythropoïétine plasmatique (P < 0,001).
Conclusion
Ces données soutiennent l’hypothèse selon laquelle l’érythropoïétine plutôt que la méthémoglobine serait un biomarqueur potentiel de l’hypoxie tissulaire induite par l’anémie. Les liens constatés entre la baisse de l’hémoglobine au cours de la CEC et l’augmentation des lactates, la baisse du pH et l’augmentation des taux d’érythropoïétine suggèrent que des modifications précoces de l’érythropoïétine plasmatique peuvent être un biomarqueur pragmatique précoce de l’hypoxie rénale induite par l’anémie. D’autres études sont nécessaires pour déterminer si les augmentations de l’érythropoïétine induite par l’anémie peuvent prédire des LRA chez les patients subissant une chirurgie cardiaque.
Enregistrement de l’essai clinique
www.clinicaltrials.gov (NCT01883713). Enregistré le 21 juin 2013.
Similar content being viewed by others
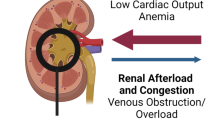
Anemia is prevalent in patients undergoing cardiac surgery1 and is associated with an increased risk of acute kidney injury (AKI)2,3,4 and mortality.3,5,6 Acute hemodilutional anemia during cardiopulmonary bypass (CPB) leads to a reduction in the intraoperative hematocrit/hemoglobin (Hb) concentration. A low hematocrit during CPB has been associated with increased stroke, cardiac injury, AKI, and mortality.2,3,7,8 Anemia-induced tissue hypoxia may be a central mechanism of organ injury and morbidity during acute hemodilution.6,9 Nevertheless, clinical evidence of tissue hypoxia at low Hb levels has not been clearly shown. Identifying biomarkers of anemia-induced tissue hypoxia, in addition to Hb concentration, could provide additional patient-specific evidence of tissue hypoxia, which could be utilized to inform treatment decisions, including the optimal threshold to transfuse red blood cells (RBCs).10
Upregulation of hypoxia-inducible factor (HIF)-dependent cellular responses has been shown to maintain oxygen homeostasis and support survival in anemic animals undergoing acute hemodilution.9,11,12 In previous studies, we explored the possibility that anemia-induced increases in methemoglobin (MetHb) may be linked to these HIF-dependent responses, suggesting that MetHb is a potential biomarker for anemia-induced tissue hypoxia.10,11,13 In animal models, the anemia-induced increase in MetHb has been shown to be linked to HIF and neural nitric oxide synthase (nNOS)-derived nitric oxide (NO), as the increase in MetHb is attenuated in nNOS-deficient mice.10 Thus, there is a potential link among anemia-induced tissue hypoxia, hypoxic adaptive responses (HIF, erythropoietin, nNOS, NO), and generation of increased MetHb levels in anemic animals.9,12,14,15 In addition, downregulation of hepcidin by HIF and erythropoietin (EPO)-dependent mechanisms may provide additional evidence of anemic hypoxia.16,17
Another potential mechanistic link among tissue hypoxia, deoxyhemoglobin, and MetHb has been supported by experimental studies.10,18 During anemia, the proportion of deoxyhemoglobin is elevated because of increases in O2 extraction at the level of the tissue. Experimental evidence suggests that increased deoxyhemoglobin may contribute to hypoxic signaling and increased tissue blood flow through its activity as a nitrite reductase by transforming stable NO metabolites (nitrite) to biologically active NO.10 An increase in biologically active NO may contribute to arteriolar vasodilation and increase blood flow to hypoxic vascular beds.18 In this reaction, MetHb is a measured byproduct and potential biomarker of these cellular mechanisms. Furthermore, an increase in MetHb has been observed in proportion to decreased Hb in both animal and human studies.11,13 Thus, increased levels of MetHb may be a biomarker of adaptive tissue responses to anemia-induced hypoxic stress.19
Finally, RBC hemolysis, and the subsequent elevation of plasma Hb levels, has been associated with increased oxidation of Hb to MetHb.20 We wished to assess whether CPB-induced trauma to RBC resulted in cell lysis/damage and an increase in plasma Hb. Increased levels of plasma Hb may result in vasoconstriction via NO binding, causing tissue hypoxia, providing a further rationale for MetHb as a potential biomarker for tissue hypoxia.
In the current prospective study, we hypothesized that hemodilutional anemia during CPB would increase the MetHb level as an indicator of anemia-induced tissue hypoxia during cardiac surgery. The primary purpose was to determine if levels of MetHb changed in response to reductions in Hb. Secondary and exploratory candidate biomarkers for anemia-induced tissue hypoxia included traditional hypoxia-regulated molecules (EPO and hepcidin). In addition, we wished to determine if increased levels of plasma Hb were detectable and could be correlated to MetHb. Finally, cerebral oximetry was measured to determine if any changes in brain oxygen saturation occurred in our cohort.
Methods
Upon registering this trial (ClinicalTrials.gov ID: NCT01883713) and with Institutional Research Ethics Board approval (27 March 2012), we conducted a prospective observational study of 64 patients undergoing cardiac surgery using CPB at St. Michael’s Hospital, Toronto, Ontario, Canada. Eligibility criteria included all patients undergoing cardiac surgery with CPB. Patients excluded from the study included those with baseline hypoxemia (oxygen saturation < 90%), preoperative anemia, history of congenital methemoglobinemia, comorbidities including acute or chronic renal failure requiring dialysis, and patients requiring emergency surgery.
With informed consent, five arterial blood samples were taken from each patient at the following time points: 1) baseline—the sample was obtained just prior to perfusion; 2) pump one to 15 min after the start of CPB; 3) pump two to 45 min after the start of CPB; 4) post-CPB—15 min following weaning from CPB and restoration of physiological circulation; 5) intensive care unit (ICU)—upon admission to the ICU. On-pump time points within one hour from the start of CPB were chosen to maximize complete data collection because of the interpatient variability for time on CPB. For example, in the recently published TRICS III trial, > 75% of all patients were on CPB for at least one hour.21 Therefore, selection of on-pump time points within one hour on CPB was predicted to be most inclusive for patients undergoing cardiac surgery on CPB. Erythropoietin and hepcidin were not measured on-pump because of known hemodilution for these samples.
Each fresh arterial sample was collected into a heparinized syringe for routine arterial blood gas and co-oximetry assessment including total Hb, MetHb, plasma Hb, and EPO.
An EDTA tube was collected to allow plasma hepcidin measurement, with an additional tube containing citrate and diethylenetriaminepentaacetic acid as anticoagulant used for blood and plasma nitrite and nitrate measurement.
Patient demographics and clinical data were obtained at the time of consent and from the clinical database Sorian Clinicals (Cerner Health Sciences, Kansas City, MO, USA). Clinical data were recorded pre-, intra-, and postoperatively until discharge to include demographics, preadmission medical history, medications, and transfusion of blood products. Postoperative AKI was assessed utilizing the KDIGO guidelines (increase in serum creatinine > 26.5 umol·L−1 within 48 hr of surgery or > 1.5 times the baseline value within seven days of surgery).22
The Hb and MetHb were measured by co-oximetry along with complete arterial blood gas values. For the first phase of the study, all samples were analyzed with a Radiometer ABL 800 flex analyzer (Copenhagen, Denmark, n = 36); for the second phase of the study, all samples were analyzed with a GEM Premier 4000 analyzer (Instrumentation Laboratory, Bedford, MA, USA, n = 28). This was due to an equipment change in the core laboratory at St. Michael’s Hospital. The core laboratory at our institution had two comparable machines, and samples were analyzed in either one of these two machines. Quality assurance and calibration were routinely completed for both machines. The MetHb level is presented as a measured percentage of total hemoglobin and as a calculated value of MetHb concentration (g·L−1).
Plasma nitrate and nitrite were measured utilizing previously published methodology.23 Plasma Hb was assessed by the method of Fairbanks et al. by measuring the absorbance (A) of 11-fold diluted heparin plasma at 415 nm, 450 nm, and 700 nm and using the following equation: Hb (g·L−1) = 1.55·A415-1.3·A450 – 1.24·A700.24 Plasma was obtained after centrifuging whole blood samples at 300 rpm for 15 min. Samples were aliquoted and stored at − 80°C. Plasma EPO levels were measured utilizing the Beckman DXI erythropoietin assay #A16364 (Beckman Coulter, Mississauga, ON, Canada). A subset of samples was utilized to measure hepcidin levels by ELISA (Bachem, Torrance, CA, USA).
Cerebral oximetry allowing brain oxygen saturation measurement was continuously monitored by placement of right and left cerebral probes in 12 patients throughout the surgery using non-invasive near-infrared spectroscopy technology (NIRS; EQUANOX™ Advance Sensory Model 8004CA, Nonin Medical Inc; Plymouth, MN, USA).
Sample size calculation and statistical analysis
The primary outcome was the correlation of the changes in Hb and MetHb concentrations. A sample size estimate was based on the method of DuPont and Plummer25 and our published preliminary human data from180 patients.13 The standard deviation of the delta Hb and MetHb was observed to be 26 and 0.0031, respectively, with a slope estimate of -0.00005 obtained when the change in MetHb was regressed against Hb. Assuming that the true slope (measured in the current study) is consistent with these data, then the line obtained by regressing the change of MetHb against Hb remains at -0.00005. We estimate that we will need to study 58 subjects to be able to reject the null hypothesis that this slope equals zero (α = 0.05, power = 0.80). Taking into consideration an attrition rate of 10% to account for dropouts, we will need a total of 64 patients. Secondary outcomes included arterial blood gasses and changes in potential hypoxic biomarkers including EPO and hepcidin, plasma Hb, nitrate, and nitrite.
All data are presented as median [interquartile range (IQR)] and were analyzed by repeated measures analysis of variance (ANOVA) on ranks with Dunn’s correction for multiple comparisons for all arterial blood gas and hypoxic biomarker analyses. Linear regression was utilized to assess potential relationships between measured parameters, specifically, to determine if there were any relationships between changes in Hb upon initial hemodilution on CPB (i.e., change in Hb from baseline to pump 1). In addition, we assessed potential relationships between Hb and any potential hypoxic biomarkers in measurements in post-CPB or ICU samples. A sensitivity analysis was performed removing patients who received RBC transfusions perioperatively, as RBC transfusion may influence levels of MetHb.10
A post hoc assessment of multiple linear regression was performed to determine if a linear combination of independent variables may have contributed to any observed associations. Subjects with missing data points for each outcome were excluded from the analysis. Repeated measures ANOVA on ranks and regressions was performed with Sigmaplot 11.0 software (Systat, San Jose, CA, USA). P < 0.05 was taken to be significant.
Results
A total of 68 patients consented to participate in the study (Fig. 1). Data from four patients were excluded because of the lack of sample collection as a result of surgical complications (n = 2), change of surgical management to off-pump surgery (n = 1), and change in surgical date (n = 1). Data for biomarker outcomes were acquired for 64 patients. Complete data for the primary outcome of MetHb were available in 58 patients. Complete data for the plasma EPO concentration were obtained in 51 patients, hepcidin concentration was measured in 36 patients, plasma Hb was measured in 40 patients, and cerebral oximetry was measured in 12 patients. Baseline and operative characteristics are displayed in Table 1. Arterial blood gas analysis did not reveal any evidence of significant hypoxemia (partial pressure of oxygen [PaO2] < 60 mmHg) throughout the study period (Table 2). Minor changes in pH, PaO2, and lactate were observed most frequently in the ICU sample (Table 2).
Hemoglobin and biomarker outcomes
Hemoglobin concentration fell immediately upon initiation of CPB and remained reduced through to ICU admission (P < 0.001 vs baseline; Table 3, Fig. 2A). MetHb levels increased upon ICU admission, both when assessed as a percent of total Hb and as a concentration of MetHb (P < 0.001 vs baseline; Table 3, Fig. 2 B, D). As for the primary outcome, no correlation was observed between the initial change in Hb (pump 1-baseline) and change in MetHb (ICU-baseline) (r2 = 0.03; P = 0.23, Fig. 3). Preoperative and ICU MetHb levels were not different in patients with a smoking history relative to those without a smoking history (baseline: 1.0 [0.7-1.3] g·L−1 vs 0.8 [0.5-1.2] g·L−1, P = 0.55; ICU: 1.4 [0.8-2.0] g·L−1 vs 1.2 [0.7-1.6] g·L−1, P = 0.60).
Panel A) Hemoglobin concentrations decreased following baseline, and this reduction was sustained into intensive care unit (ICU) admission. Panel B/D) Methemoglobin levels remained at baseline levels and increased upon ICU admission. Panel C) Plasma hemoglobin concentration remained at baseline levels and increased after cardiopulmonary bypass (CPB). The elevation in plasma hemoglobin level was sustained into ICU admission. (*P < 0.001 vs baseline. Repeated measures analysis of variance on ranks)
No correlation was observed when change in methemoglobin concentration from baseline to intensive care unit (ICU) admission was regressed against change in hemoglobin concentration from baseline to pump 1 (R2 = 0.03; P = 0.23; dotted curved lines represent the 95% confidence intervals. Solid black line represents slope of linear regression)
Erythropoietin levels increased upon entry into the ICU (P < 0.001 vs baseline; Table 3; Fig. 4A). By contrast, hepcidin levels did not change perioperatively (Table 3; Fig. 4B). Erythropoietin levels in the ICU correlated with the Hb concentration within 15 min of CPB (pump 1) (R2 = 0.15; P = 0.004; Fig. 5). Multiple linear regression showed that both lactate post-CPB and pH post-CPB independently contributed to the correlation between EPO in the ICU and Hb at pump 1 (lactate post-CPB, R2 = 0.25; P < 0.001; pH post-CPB, R2 = 0.24; P = 0.001) (Fig. 6). Furthermore, in patients without evidence of AKI, EPO levels were increased upon entry to the ICU (P < 0.001 vs baseline; Table 4; Fig. 7). Eight patients experienced transient increases in creatinine, consistent with a diagnosis of AKI (KDIGO, Table 4). On average, patients with AKI had a numerical trend toward a larger increase in EPO in the ICU relative to patients who did not experience an acute rise in creatinine, though this was not significant (P = 0.08, Table 4, Fig. 7). In patients with acute kidney injury, EPO levels increased in the ICU relative to post-CPB values (P = 0.008; Table 4; Fig. 7).
Panel A) A correlation was observed when erythropoietin in the intensive care unit (ICU) was regressed against both lactate after cardiopulmonary bypass (CPB) and hemoglobin concentration at pump 1 (R2 = 0.25; P < 0.001). Panel B) A correlation was observed when erythropoietin in the ICU was regressed against both pH post-cardiopulmonary bypass and hemoglobin concentration at pump 1 (R2 = 0.24; P = 0.001; the multiple linear regression of two independent variables on erythropoietin levels is represented as a plane of best fit)
In patients with normal creatinine clearance, erythropoietin levels decreased following cardiopulmonary bypass (CPB) and increased upon entry into the intensive care unit (ICU). In patients with acute kidney injury, erythropoietin levels did not change from baseline; however, erythropoietin levels increased from post-CPB levels upon entry into the ICU. (*P < 0.001 vs baseline; #P = 0.008 vs post-CPB. Repeated measures analysis of variance on ranks)
Plasma Hb levels increased at the post-CPB and ICU time points (P < 0.001 vs baseline for both; Table 3; Fig. 2C). In addition, plasma Hb levels during the post-CPB time point correlated with EPO levels in the ICU (R2 = 0.27; P < 0.001; Fig. 8A) and MetHb levels in the ICU (R2 = 0.17; P = 0.008; Fig. 8B). A significant reduction in the plasma nitrate levels was observed upon entry to the ICU (P = 0.004; Table 3). Nevertheless, no change in plasma nitrite was observed. Furthermore, no correlations were observed between initial changes in Hb or MetHb vs plasma nitrite or nitrate. Hypothesis-generating correlations were observed between several other biomarkers including: 1) EPO in the ICU and change in MetHb (ICU-baseline; R2= 0.09; P = 0.03); 2) hepcidin in the ICU and initial delta Hb (pump 1-baseline; R2 = 0.41; P < 0.001). Left and right brain oxygen saturation was reduced at the pump 2 time point (P = 0.008 vs baseline; Fig. 8). This reduction in right brain oxygen saturation was sustained into the post-CPB time point (P = 0.001 vs baseline; Fig. 9).
Panel A) A correlation was observed when the erythropoietin concentration in the intensive care unit (ICU) was regressed against the plasma hemoglobin concentration after cardiopulmonary bypass (CPB) (R2 = 0.27, P < 0.001). Panel B) A correlation was observed when the methemoglobin concentration in the ICU was regressed against the plasma hemoglobin concentration after CPB (R2 = 0.17; P = 0.008; dotted curved lines represent the 95% confidence intervals. Solid black line represents slope of linear regression)
Left brain oxygen saturation levels were reduced during the pump 2 time point. Right brain oxygen saturation levels were reduced during the pump 2 time point, and this reduction was sustained following cardiopulmonary bypass (CPB) (P ≤ 0.008 vs baseline, repeated measures analysis of variance on ranks)
Of the 64 patients, 17 (27%) were transfused with red cells, plasma, platelets, and/or cryoprecipitate. Fifteen patients received a total of 37 units of RBCs (Table 5). Five patients received an RBC transfusion in the operating room. Intraoperative RBC transfusion did not have a clear impact on MetHb levels (Table 6). Removal of these five patients from our analysis did not change the significance of any of the observed statistical findings.
Discussion
In this prospective observational study, patients undergoing acute hemodilutional anemia during CPB showed an increase in serum MetHb, EPO, and plasma Hb postoperatively. Previously, we had observed a consistent increase in MetHb that correlated with a decrease in Hb in our anemic animal models.11,19 In addition, we, and others, have observed a relationship between increased MetHb and decreased Hb in clinical studies.13,26,27 These background studies provided the rationale for pursing the current prospective trial. While we observed that MetHb was increased in the ICU, no clear relationship was observed between the acute decrease in Hb following initiation of CPB and the subsequent increase in MetHb. In addition, no significant correlations were shown between change in nitrite (potential substrate for NO production) and increased MetHb (reaction byproduct). We anticipated a decrease in nitrite levels, but did not observe this change or any evidence that hemodilution altered the balance between nitrite reduction to NO.19 The small changes in MetHb, coupled with the finding that we did not observe a change in plasma nitrite, explain the absence of a correlation between these two metabolites. We note that the patient-to-patient variance in plasma nitrite and nitrate levels would likely mask any hemodilution-dependent changes and that measurements in the systemic circulation may not clearly reflect important changes in the microcirculation. Thus, the current data did not support our primary hypothesis that MetHb would be correlated with an acute drop in Hb or that increased deoxyhemoglobin levels resulted in increased nitrite reductase activity and generation of active NO.
By contrast, we observed a significant correlation among the early decrease in Hb, after initiation of CPB, an increase in lactate (and drop in pH) following CPB, and a later rise in plasma EPO in the ICU. This suggests that acute hemodilutional anemia resulted in renal tissue hypoxia, anerobic metabolism,28 and subsequent secretion of EPO. An alternate argument to explain the reduction in pH could be an effect of anemia-induced tissue hypoxia on the ability of the kidney to generate or absorb bicarbonate.29 These data suggest that the traditional mechanism by which a low hematocrit triggers an increase in renal EPO secretion can be detected in real time at an early point following heart surgery.
Experimental studies assessing the relationship among acute anemia, renal tissue hypoxia, and increased expression of EPO show that the kidney is a primary sensor for acute reductions in hematocrit.30 Utilizing different models of anemia, we have shown that a measurable reduction in renal tissue partial pressure of oxygen (PO2) occurs at an Hb threshold near 90 g·L−1.31 This is directly associated with increased real-time expression of HIF-luciferase within the region of the kidney in anemic transgenic mice possessing a firefly luciferase/reporter system.9,31 Assessment of tissue-specific HIF responses within the kidney shows a 20- to100-fold increase in EPO messenger ribonucleic acid (mRNA) levels. This is much higher than observed in other organs, such as the liver and brain, which show an approximate two-fold increase in mRNA expression.31 The thresholds for this response and of increased serum EPO levels both occur near an Hb threshold of 90 g·L−1.15 Assessment of these biomarkers, and the Hb threshold at which they are activated, may help guide clinical management of acutely anemic patients.
The lack of an increase in renal blood flow during anemia, in combination with a dramatic reduction in blood oxygen content, likely contributes to the degree of renal tissue hypoxia that we have observed in experimental models.15,31 By contrast, in these same experimental models, cardiac output and cerebral blood flow are dramatically increased, thereby preserving brain tissue PO2 and limiting the magnitude of HIF-dependent responses. It is conceivable that acute renal hypoxia and overall hypoxia signaling may trigger these adaptive cardiovascular responses to minimize the degree of cerebral hypoxia in vital organs with high metabolic requirements such as the brain. This may explain why we did not observe any severe reduction in cerebral oximetry in our clinical patients who exhibited a rise in systemic EPO.
Renal tissue hypoxia has been proposed as a cause of acute renal failure in clinical settings including CPB.32 Acute hemodilution on CPB has been associated with AKI2,3,4 and renal medullary tissue hypoxia in experimental models,33,34,35 and acute anemia-induced renal hypoxia is associated with increased HIF and EPO expression.15,31 A potential link between renal tissue hypoxia and AKI has been proposed by a recent clinical study that showed that decreased renal urinary PO2 (a surrogate of renal tissue hypoxia) predicted acute renal failure following heart surgery.36 Our finding that acute hemodilution on CPB results in a proportional increase in lactate, decrease in pH, and increase in systemic EPO levels suggests that EPO may be a real-time biomarker for hypoxic renal injury. Although we did not show a clear relationship between the EPO level and AKI, our data suggest that EPO levels were elevated in patients with an acute rise in creatinine (KDIGO) relative to those that did not have AKI. Further research may help to determine if a causal relationship exists among acute anemia, renal tissue hypoxia, elevated EPO, and AKI in patients undergoing cardiac surgery.
The observed rise in plasma Hb post-CPB likely represents a degree of red cell damage during CPB. Plasma Hb is a well-known renal toxin that has been associated with AKI in patients undergoing CPB and heart surgery.37 Further exploration of the potential significance of increased plasma Hb following CPB showed a correlation between increased plasma Hb and the subsequent increases in plasma MetHb and EPO levels. One explanation for these relationships is that plasma Hb is prone to oxidation to MetHb in the absence of the RBC MetHb reductase system. An alternate explanation is that plasma Hb is associated with enhanced NO binding in the renal microvasculature, leading to arteriolar vasoconstriction37,38 and subsequent renal tissue hypoxia. Such tissue hypoxia may contribute to the observed increase in EPO and, if severe, may be responsible for the development of AKI. Evidence in support of this hypothesis is provided by Kim-Campbell et al. who have shown a relationship between plasma Hb levels and the acute rise in creatinine in children undergoing CPB.37
Enhanced levels of tissue MetHb may also indicate activity of oxidative mechanisms within the kidney. Deuel et al. provide experimental evidence that plasma Hb is trapped within the kidney vasculature and oxidized to MetHb.38 This oxidative process has been associated with increased expression of hypoxic response molecules including HIF and hemoxygenase-1. Evidence of oxidative tissue damage by MetHb has also been observed in other experimental models of diseases including multiple sclerosis.39 Thus, enhanced oxidation of Hb to MetHb may be a potential mechanism contributing to the pathophysiology of AKI following CPB.37
We did not observe any change in serum hepcidin levels. The regulation of hepcidin is under multiple influences including increased expression by inflammatory mediators such as interleukin-6 and decreased expression by tissue hypoxia mediated by HIF.40,41 During non-cardiac surgery, increased hepcidin levels are thought to occur because of increased levels of circulating cytokines.42 By contrast, hypoxia and anemia are known to suppress hepcidin expression via upregulation of HIF.40,41,43,44 The HIF-dependent suppression of hepcidin is co-dependent on EPO expression by newly defined mechanisms.43,44 Thus, stable hepcidin levels in the plasma may provide additional evidence of hypoxic signaling within the kidney.
A protocolized approach to optimizing perfusion during CPB can result in improved cerebral oxygen saturation during CPB.45 Conversely, reduced brain oxygen saturation during cardiac surgery may be associated with adverse outcomes.46 We observed a small decrease in brain oximetry in a subgroup of our patients, likely reflecting the cerebral perfusion is preferentially maintained at Hb levels near 100 g·L−1. As previously mentioned, experimental studies have shown preferential brain perfusion relative to the kidney and liver during graded levels of acute hemodilution.15,31 Thus, measurement of cerebral oximetry may be reserved for detecting major changes in cerebral perfusion, but may not be suitable for assessing subtle changes in tissue PO2 associated with moderate hemodilutional anemia.
Limitations and future directions
There are several limitations to our study. For example, the current study did not confirm the findings of our previous retrospective study. One potential explanation could be due to differences in the timing of blood sampling between the studies. Data from the retrospective study were acquired from the clinical database, and measurement of arterial blood gases and MetHb was not protocolized.13 In the current study, we utilized routine protocolized measurements of Hb and MetHb, which may not be indicative of the retrospective study. Second, the sample size may have been inadequate to clearly show a relationship between changes in MetHb and Hb. Of interest, our sample size did allow us to independently associate acute anemia and lactic acidosis post-CPB to a late rise in EPO. This indicates that although our primary hypothesis was not demonstrated, other markers of tissue hypoxia may be more sensitive and biologically relevant. Third, the biological mechanism proposed, which was derived from rodent studies, may not translate into humans.
Conclusions
In this study, we observed evidence of an increase in MetHb, EPO, and plasma Hb following CPB and heart surgery. Correlations among the levels of plasma Hb, MetHb, and EPO suggest that a common mechanism may contribute to these changes. These measures may have clinical relevance as patient-specific biomarkers of anemic hypoxic and/or inflammatory organ injury following CPB and cardiac surgery.
References
Hung M, Besser M, Sharples LD, Nair SK, Klein AA. The prevalence and association with transfusion, intensive care unit stay and mortality of pre-operative anaemia in a cohort of cardiac surgery patients. Anaesthesia 2011; 66: 812-8.
Swaminathan M, Phillips-Bute BG, Conlon PJ, Smith PK, Newman MF, Stafford-Smith M. The association of lowest hematocrit during cardiopulmonary bypass with acute renal injury after coronary artery bypass surgery. Ann Thorac Surg 2003; 76: 784-91; discussion 792.
Loor G, Li L, Sabik JF 3rd, Rajeswaran J, Blackstone EH, Koch CG. Nadir hematocrit during cardiopulmonary bypass: end-organ dysfunction and mortality. J Thorac Cardiovasc Surg 2012; 144(654–62): e4.
Karkouti K, Beattie WS, Wijeysundera DN, et al. Hemodilution during cardiopulmonary bypass is an independent risk factor for acute renal failure in adult cardiac surgery. J Thorac Cardiovasc Surg 2005; 129: 391-400.
Hare GM, Freedman J, Mazer CD. Review article: risks of anemia and related management strategies: can perioperative blood management improve patient safety? Can J Anesth 2013; 60: 168-75.
Shander A, Javidroozi M, Ozawa S, Hare GM. What is really dangerous: anaemia or transfusion? Br J Anaesth 2011; 107(Suppl 1): i41-59.
Karkouti K, Djaiani G, Borger MA, et al. Low hematocrit during cardiopulmonary bypass is associated with increased risk of perioperative stroke in cardiac surgery. Ann Thorac Surg 2005; 80: 1381-7.
DeFoe GR, Ross CS, Olmstead EM, et al. Lowest hematocrit on bypass and adverse outcomes associated with coronary artery bypass grafting. Northern New England Cardiovascular Disease Study Group. Ann Thorac Surg 2001; 71: 769-76.
Tsui AK, Marsden PA, Mazer CD, et al. Priming of hypoxia-inducible factor by neuronal nitric oxide synthase is essential for adaptive responses to severe anemia. Proc Natl Acad Sci USA 2011; 108: 17544-9.
Hare GM, Tsui AK, Crawford JH, Patel RP. Is methemoglobin an inert bystander, biomarker or a mediator of oxidative stress–the example of anemia? Redox Biol 2013; 1: 65-9.
Tsui AK, Dattani ND, Marsden PA, et al. Reassessing the risk of hemodilutional anemia: Some new pieces to an old puzzle. Can J Anesth 2010; 57: 779-91.
McLaren AT, Marsden PA, Mazer CD, et al. Increased expression of HIF-1alpha, nNOS, and VEGF in the cerebral cortex of anemic rats. Am J Physiol Regul Integr Comp Physiol 2007; 292: R403-14.
Hare GM, Mu A, Romaschin A, et al. Plasma methemoglobin as a potential biomarker of anemic stress in humans. Can J Anesth 2012; 59: 348-56.
Hare GM, Mazer CD, Mak W, et al. Hemodilutional anemia is associated with increased cerebral neuronal nitric oxide synthase gene expression. J Appl Physiol 1985; 2003(94): 2058-67.
Tsui AK, Marsden PA, Mazer CD, et al. Differential HIF and NOS responses to acute anemia: defining organ-specific hemoglobin thresholds for tissue hypoxia. Am J Physiol Regul Integr Comp Physiol 2014; 307: R13-25.
Gammella E, Diaz V, Recalcati S, et al. Erythropoietin’s inhibiting impact on hepcidin expression occurs indirectly. Am J Physiol Regul Integr Comp Physiol 2015; 308: R330-5.
Peyssonnaux C, Zinkernagel AS, Schuepbach RA, et al. Regulation of iron homeostasis by the hypoxia-inducible transcription factors (HIFs). J Clin Invest 2007; 117: 1926-32.
Cosby K, Partovi KS, Crawford JH, et al. Nitrite reduction to nitric oxide by deoxyhemoglobin vasodilates the human circulation. Nat Med 2003; 9: 1498-505.
Crawford JH, Isbell TS, Huang Z, et al. Hypoxia, red blood cells, and nitrite regulate NO-dependent hypoxic vasodilation. Blood 2006; 107: 566-74.
Kato GJ, Steinberg MH, Gladwin MT. Intravascular hemolysis and the pathophysiology of sickle cell disease. J Clin Invest 2017; 127: 750-60.
Mazer CD, Whitlock RP, Fergusson DA, et al. Restrictive or liberal red-cell transfusion for cardiac surgery. N Engl J Med 2017; 377: 2133-44.
KDIGO Board Members. Kidney disease: improving global outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO clinical practice guideline for acute kidney injury. Kidney International Supplements 2012. DOI: https://doi.org/10.1038/kisup.2012.4.
Lang JD Jr, Teng X, Chumley P, et al. Inhaled NO accelerates restoration of liver function in adults following orthotopic liver transplantation. J Clin Invest 2007; 117: 2583-91.
Fairbanks VF, Ziesmer SC, O’Brien PC. Methods for measuring plasma hemoglobin in micromolar concentration compared. Clin Chem 1992; 38: 132-40.
Dupont WD, Plummer WD Jr. Power and sample size calculations for studies involving linear regression. Control Clin trials 1998; 19: 589-601.
Ash-Bernal R, Wise R, Wright SM. Acquired methemoglobinemia: a retrospective series of 138 cases at 2 teaching hospitals. Medicine (Baltimore) 2004; 83: 265-73.
Kane GC, Hoehn SM, Behrenbeck TR, Mulvagh SL. Benzocaine-induced methemoglobinemia based on the Mayo Clinic experience from 28 478 transesophageal echocardiograms: incidence, outcomes, and predisposing factors. Arch Intern Med 2007; 167: 1977-82.
Rashkin MC, Bosken C, Baughman RP. Oxygen delivery in critically ill patients. Relationship to blood lactate and survival. Chest 1985; 87: 580-4.
Boron WF. Acid-base transport by the renal proximal tubule. J Am Soc Nephrol 2006; 17: 2368-82.
Ngo JP, Evans RG. Editorial focus: multitasking: a challenge for the kidney focus on - “red blood cell antibody induced anemia causes differential degrees of tissue hypoxia in..”. Am J Physiol Regul Integr Comp Physiol 2018. DOI: https://doi.org/10.1152/ajpregu.00011.2018.
Mistry N, Mazer CD, Sled JG, et al. Red blood cell antibody induced anemia causes differential degrees of tissue hypoxia in kidney and brain. Am J Physiol Regul Integr Comp Physiol 2018. DOI: https://doi.org/10.1152/ajpregu.00182.2017.
Ow CP, Ngo JP, Ullah MM, Hilliard LM, Evans RG. Renal hypoxia in kidney disease: cause or consequence? Acta Physiol (Oxf) 2017. DOI: https://doi.org/10.1111/apha.12999.
Darby PJ, Kim N, Hare GM, et al. Anemia increases the risk of renal cortical and medullary hypoxia during cardiopulmonary bypass. Perfusion 2013; 28: 504-11.
Stafford-Smith M, Grocott HP. Renal medullary hypoxia during experimental cardiopulmonary bypass: a pilot study. Perfusion 2005; 20: 53-8.
Patel NN, Lin H, Toth T, et al. Reversal of anemia with allogenic RBC transfusion prevents post-cardiopulmonary bypass acute kidney injury in swine. Am J Physiol Renal Physiol 2011; 301: F605-14.
Zhu MZ, Martin A, Cochrane AD, et al. Urinary hypoxia: an intraoperative marker of risk of cardiac surgery-associated acute kidney injury. Nephrol Dial Transplant 2018. DOI: https://doi.org/10.1093/ndt/gfy047.
Kim-Campbell N, Gretchen C, Callaway C, et al. Cell-free plasma hemoglobin and male gender are risk factors for acute kidney injury in low risk children undergoing cardiopulmonary bypass. Crit Care Med 2017; 45: e1123-30.
Deuel JW, Schaer CA, Boretti FS, et al. Hemoglobinuria-related acute kidney injury is driven by intrarenal oxidative reactions triggering a heme toxicity response. Cell Death Dis 2016; 7: e2064.
Bamm VV, Henein ME, Sproul SL, Lanthier DK, Harauz G. Potential role of ferric hemoglobin in MS pathogenesis: effects of oxidative stress and extracellular methemoglobin or its degradation products on myelin components. Free Radic Biol Med 2017; 112: 494-503.
D’Angelo G. Role of hepcidin in the pathophysiology and diagnosis of anemia. Blood Res 2013; 48: 10-5.
Talbot NP, Lakhal S, Smith TG, et al. Regulation of hepcidin expression at high altitude. Blood 2012; 119: 857-60.
Park KH, Sawada T, Kosuge T, et al. Surgical inflammation induces hepcidin production after abdominal surgery. World J Surg 2012; 36: 800-6.
Liu Q, Davidoff O, Niss K, Haase VH. Hypoxia-inducible factor regulates hepcidin via erythropoietin-induced erythropoiesis. J Clin Invest 2012; 122: 4635-44.
Pak M, Lopez MA, Gabayan V, Ganz T, Rivera S. Suppression of hepcidin during anemia requires erythropoietic activity. Blood 2006; 108: 3730-5.
Deschamps A, Hall R, Grocott H, et al. Cerebral oximetry monitoring to maintain normal cerebral oxygen saturation during high-risk cardiac surgery: a randomized controlled feasibility trial. Anesthesiology 2016; 124: 826-36.
Murkin JM, Adams SJ, Novick RJ, et al. Monitoring brain oxygen saturation during coronary bypass surgery: a randomized, prospective study. Anesth Analg 2007; 104: 51-8.
Acknowledgements
This study was supported by the Canadian Anesthesiologists’ Society, Dr. Earl Wynands/Fresenius Kabi Research Award. Dr. Hare and Dr. Mazer are supported by University of Toronto, Department of Anesthesia Merit Awards, Academic Health Science Centre Alternative Funding Plan (SMH-15-012). The authors acknowledge Arkady Barbev for completing background research relating to this study, Eric Ferguson for contributing to data acquisition, and Suresh Tharmaradinam for contributions as research coordinator. The authors thank Nonin Medical Inc. for providing the oximeters and probes.
Disclosures
Dr. Hare has received funding from Forest Research Inc. for basic science studies and salary support from Johnson & Johnson Inc. for his role in the St. Michael’s Hospital Center of Excellence for Patient Blood Management from Johnson & Johnson Inc.
Conflicts of interest
None declared.
Editorial responsibility
This submission was handled by Dr. Hilary P. Grocott, Editor-in-Chief, Canadian Journal of Anesthesia.
Author contributions
Gregory M.T. Hare, Kaho Han, Yevheniy Leshchyshyn, Nikhil Mistry, Albert K.Y. Tsui, Jaideep Honavar, Rakesh P. Patel, Alexander Romaschin, Philip W. Connelly, W. Scott Beattie, and C. David Mazer contributed substantially to the conception and design of the manuscript. Gregory M.T. Hare, Kaho Han, Yevheniy Leshchyshyn, Tiffanie Kei, Si Yuan Dai, Albert K.Y. Tsui, Rakesh P. Patel, Sanjay Yagnik, Shelley L. Welker, and Tessa Tam contributed substantially to the acquisition of data. Gregory M.T. Hare, Kaho Han, Yevheniy Leshchyshyn, Nikhil Mistry, Albert K.Y. Tsui, Rakesh P. Patel, Alexander Romaschin, Philip W. Connelly, W. Scott Beattie, and C. David Mazer contributed substantially to the analysis and interpretation of data.
All authors contributed to drafting, revising, and adding important intellectual content to the manuscript. All authors have read and approved the final content of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hare, G.M.T., Han, K., Leshchyshyn, Y. et al. Potential biomarkers of tissue hypoxia during acute hemodilutional anemia in cardiac surgery: A prospective study to assess tissue hypoxia as a mechanism of organ injury. Can J Anesth/J Can Anesth 65, 901–913 (2018). https://doi.org/10.1007/s12630-018-1140-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-018-1140-0