Abstract
Background
In selected patients, stress-only SPECT imaging has been proposed as an alternative to rest-stress SPECT imaging to improve laboratory efficiency and reduce radiation exposure. The impact of attenuation correction (AC) upon interpretation, post-test patient management and cardiac risk stratification in relation to stress-only imaging is not well understood.
Objectives
The purpose of this study was to determine the clinical value for laboratory throughput and predicting outcomes of normal and abnormal stress-only SPECT imaging with AC in a consecutive series of clinically referred patients.
Methods
A retrospective analysis of 1,383 consecutive patients who were scheduled for stress-only SPECT imaging for symptom assessment of suspected myocardial ischemia was performed. All images had been interpreted and categorized using the standard 17-segment model without AC followed by AC. Follow-up data for 2.1 ± 1.3 years after SPECT imaging for the occurrence of cardiac events (non-fatal MI, cardiac death, and cardiac revascularization) previously collected by routine methods were reviewed.
Results
Non-AC SPECT image interpretation revealed that 58% (802/1383) of patients had abnormal stress images. AC image interpretation of the abnormal non-AC images re-classified 83% (666/802) of these as normal. Among patients with abnormal stress images after AC (136/1383), 63% (86/136) returned for additional rest scans, while the remaining 37% (50/136) were clinically managed without further rest images. The incidence of cardiac death or non-fatal MI was very low in patients with normal stress-only scans (0.7%).
Conclusion
A strategy of stress-only imaging with AC in symptomatic patients is an efficient method which appropriately identifies at risk and low-risk patients yielding a low percentage requiring rest imaging. Clinical decisions can be made based on abnormal stress-only imaging without further rest imaging if clinically appropriate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rest-stress Tc-99m single-photon emission computed tomography (SPECT) imaging is a widely used non-invasive technique for the assessment of patients with known or suspected coronary artery disease (CAD). Unfortunately, this procedure requires 3-4 hours to complete, with considerable time spent on a rest study that often is not necessary or useful. Stress-only imaging in selected patients has emerged as an alternative means of reducing both procedure time and radiation exposure.1,2 With this approach, the necessity for a comparative rest study is dependent upon the presence of an abnormal finding on stress imaging which frequently is due to attenuation artifact and has been estimated to occur in 50%-78% of studies.3 The use of attenuation correction (AC) with SPECT has been shown to significantly reduce false positive studies for both rest-stress and stress-only imaging.3,4
The value of stress-only imaging with normal results has been confirmed by outcomes data from previous studies.1,5-7 While most of these studies utilized AC, there is insufficient information on the impact of this technique with stress-only imaging regarding post-test patient management (necessity for additional rest imaging) and cardiac risk stratification. Accordingly, the purpose of this study was to determine the clinical value of stress-only SPECT imaging with AC in a consecutive series of clinically referred patients with symptoms suggestive of myocardial ischemia.
Methods
Patient Selection
This study was approved by and conducted within guidelines established by the Institutional Review Board of Hartford Hospital. This was a single-center, retrospective study. Consecutive patients referred for chest pain evaluation scheduled for stress-only Tc-99m SPECT imaging between January 2003 and December 2006 were identified in the Nuclear Cardiology Laboratory clinical database at Hartford Hospital. Complete demographics and medical history of all patients were obtained and systematically recorded in this clinical database prior to stress testing. History of CAD, congestive heart failure (CHF), and other risk factors was obtained by the stress lab physician from patient interview, referring physician’s office notes and requisitions for stress testing. Pretest probability of CAD was calculated for all patients using the standard Diamond and Forrester classification.8 Most patients referred for stress nuclear imaging for chest pain evaluation who did not have a history of CAD underwent a stress-only protocol. Routinely, patients with evident previous myocardial infarction (MI) or coronary artery bypass grafting (CABG) were discouraged from stress-only imaging assuming a high likelihood of a subsequent rest study being needed. The general considerations for utilizing a stress-only protocol are listed in Table 1. Patients were followed for necessity of rest imaging and cardiac events including revascularization.
Stress Protocols
Patients were scheduled for a specific stress modality according to the discretion of their referring physician, based upon perceived functional ability. Exercise was performed using symptom-limited treadmill testing according to the standard or modified Bruce protocol and within the guidelines recommended by the ACC/AHA. Vasodilator stress (with standard infusion of dipyridamole or adenosine) was performed either solely or with the addition of exercise (for those patients perceived unable to perform adequate exercise).
Imaging Protocol
Stress and, if obtained, rest images were acquired 15-60 minutes following injection of 30-45 mCi of Tc-99m sestamibi or tetrofosmin based upon body habitus. Resting images were acquired the following day on a subset of these patients to determine whether ischemia, scar, or attenuation artifact was present. All procedures followed ACC/ASNC guidelines. Specifically, all patients were imaged using 64 projections per study with at least 25-30 second per projection. Images were acquired using either Cardio 60 Vertex or Cardio MD fixed-90° dual-head SPECT cameras each outfitted with commercially available line source AC hardware and software (VantagePro [Philips Medical Systems, Milpitas, California] and ExSPECT II [Emory University, Atlanta, Georgia and Cardiovascular Imaging Technologies, Kansas City, Missouri]).
Image Reconstruction
Non-attenuation corrected (non-AC) myocardial perfusion and ECG-gated transverse images were reconstructed with filtered back-projection after low-pass filtering for noise. Butterworth filters with a cutoff of 0.46 times the Nyquist and an order of 5.0 and with a cutoff of 0.32 times the Nyquist and an order of 5.0 were used. Attenuation maps were reconstructed using a previously described algorithm that uses a Bayesian prior approach with Butterworth filter preprocessing with a cutoff of 0.43 and an order of 5.0.21. The attenuation map reconstruction used 12 iterations with a uniform initial estimate. AC of the emission images used maximum likelihood reconstruction with 30 iterations and uniform initial estimate.
Image Interpretation
Processed images with ECG gating, if performed, were displayed via the short-axis, vertical long-axis, and horizontal long-axis images in monochrome and color tables. Our standard clinical practice involved image interpretation by at least two board certified readers during daily reading sessions using the standard 17-segment model and scoring system.9 Each stress study was interpreted sequentially beginning with non-AC images first and then compared with AC images. Both non-AC and AC data were collected and recorded in our clinical database. Each segment was visually assessed and scored on a scale of 0-4 (0 = normal, 1 = mild, 2 = moderate, 3 = severe, 4 = absent photon activity). Both non-AC and AC data were included in the final reports, but the final conclusion was primarily based on AC image interpretation. Summed stress scores (SSS) were calculated by adding the 17-segment scores at stress. Based upon previous data, AC images were considered abnormal if the SSS > 0.10 An AC SSS of 1-8 was considered mildly abnormal and >8 considered moderate to severely abnormal.10 For the purpose of this study, non-AC images with SSS ≥ 1 were considered abnormal because small perfusion defects on stress imaging often prompt additional rest imaging. Summed rest scores (SRS) and summed difference scores (SDS) were calculated in patients who underwent additional rest imaging. Ejection fraction (EF) was reported separately in patients where gating could be performed. An EF < 50% was considered abnormal. For the purpose of this study, abnormal EF was not criteria to categorize an image as abnormal. An abnormal ECG response or chest pain during exercise or pharmacologic stress testing was routinely reported, but the final conclusion of the study was based on the SSS. For example, a patient who developed chest tightness with pharmacologic stress and T wave inversions on the ECG, but displayed normal perfusion and normal function on SPECT imaging, the final conclusion was reported as a normal study, even though the clinical symptoms and ECG changes were mentioned under stress test findings.
Follow-Up
Patient follow-up was routinely obtained by mailed questionnaires approximately 2 years after SPECT imaging. This is a tool that asks for endpoints including cardiac revascularization, non-fatal MI, and death from any cause. If there was no response or more information was needed, scripted telephone interviews were attempted. An investigator, unaware of clinical stress testing, and ECG-gated SPECT data, confirmed events by reviewing hospital records and the public social security database.
The endpoints for this study were cardiac revascularization including percutaneous coronary intervention (PCI) or CABG, non-fatal MI or cardiac death. The primary endpoint for the study was a composite of cardiac death or non-fatal MI. Cardiac death was defined as death due to heart failure, arrhythmia, or acute coronary syndrome. Patients with either non-fatal MI or cardiac death were censored after the first event.
Statistical Analysis
All statistical analysis was performed using SPSS version 17 (Chicago, IL).Clinical and demographic characteristics were expressed as percentages or mean ± standard deviation. Inter-group comparisons were performed using χ2 tests for categorical variables and t tests or ANOVA for continuous variables. Annualized cardiac event rates were calculated as the number of events divided by the sum of each individual follow-up period in years. A P value <.05 was considered significant in all analyses.
Results
Fifteen hundred and seven consecutive patients were scheduled for clinically indicated stress-only SPECT imaging. Complete follow-up was obtained in 92% (1,383/1,507) of these patients, which constituted the study cohort. All patients were followed for a mean of 2.1 ± 1.3 years. Patient characteristics are shown in Table 2. The mean age of the study population was 54 ± 12 years; 54% was males, 27% had diabetes, and 1% had prior CABG. Almost half of the study cohort (49% [681/1,383]) underwent pharmacologic stress. The mean pretest probability of CAD in the study cohort was 25 ± 27 (intermediate probability).8 By design, a history of prior MI or CABG was very low in the study cohort.
Impact of AC on Image Interpretation
Without AC, SPECT image interpretation revealed that 58% (802/1,383) of the stress images were abnormal, with only 42% (581/1,383) initially considered normal (Figure 1). Evaluation of the AC image re-classified 83% (666/802) of the abnormal stress images as completely normal, while 17% (136/802) remained abnormal (Figure 1). A majority (80% [532/666]) of the abnormal non-AC images that were re-classified as normal with AC had a non-AC SSS < 4 (mean 2.95 ± 1.6).
Image interpretation results and outcomes before and after AC. Flowchart summarizes this study by demonstrating the results of stress SPECT image interpretation before and after AC as well as a subgroup where additional rest imaging was performed. This figure shows how AC normalizes the majority of stress images initially considered abnormal without AC, subsequently resulting in a lesser need for additional rest imaging
Gated SPECT Data
ECG-gating could be performed in 88% (1,219/1,383) of the study patients. The mean EF of the study cohort was 64% ± 8%. Patients with normal AC images had a mean EF of 65% ± 8% whereas those with abnormal AC images had a mean EF of 60% ± 8%.
Clinical Decision With Versus Without Additional Rest Imaging
Referring physicians were provided with both non-AC and AC data. For those studies with abnormal AC images (n = 136), a rest study was requested and obtained in 67% (86/136) of patients. This constituted 6.2% of the entire study cohort (86/1,383). For the remaining 33% (50/136) of patients with an abnormal AC image, a clinical decision was made by the referring physician based on stress-only scan results. The demographic and SPECT MPI result differences between normal and abnormal imaging results are presented in Table 3. The mean SSS after AC in the abnormal stress-only group was significantly higher than the mean SSS after AC in the abnormal stress-rest group (5.4 ± 5.6 vs 4.6 ± 3.7, P = .03). In general, for patients with higher AC SSS on stress imaging, referring physicians made management decisions without additional rest scans.
A small percentage of patients with normal AC stress images returned for a rest study (3.4% [42/1,247]). This was probably because of indeterminate abnormalities on stress scans and lack of interpretive confidence without a comparative rest image. Upon reviewing both stress and rest images with AC, ultimately all these studies were considered normal.
Follow-Up for Cardiac Events
In follow-up, 0.6% (8/1,383) of patients sustained a non-fatal MI, 0.4% (6/1,383) suffered cardiac death and 2% (27/1,383) underwent coronary revascularization (Table 4). The annualized event rate for adverse cardiac outcomes (defined as cardiac death or non-fatal MI) was very low for patients with normal stress-only imaging results (0.7%, Figure 2). In patients with normal stress images who underwent additional rest imaging (3.4% [42/1,247]), there were no adverse cardiac events. The annualized event rate for adverse cardiac outcomes (cardiac death or non-fatal MI) in patients with abnormal imaging studies was very low in both the stress-only and stress-rest groups (0.9% and 0.4%, respectively, P = .6; Figures 1, 2).
Follow-up cardiac events in normal and abnormal stress-only studies and stress-rest cohorts: This bar diagram compares follow-up cardiac revascularization rates (revasc) and cardiac death or non-fatal myocardial infarction rates (cdth/MI) in stress-only and stress-rest cohorts based on normal or abnormal attenuation corrected (AC) SPECT images. A significant number of patients underwent revascularization based on abnormal stress-only imaging. Adverse cardiac events including cardiac death or non-fatal MI rates were very low for all groups of patients (normal and abnormal stress-only as well as stress-rest cohorts). This shows that a clinical decision based on abnormal stress-only imaging is a safe approach and is associated with very low cardiac morbidity or mortality
Early cardiac revascularization rates were also examined to determine the impact of stress-only imaging results on clinical decision making. As illustrated in Figure 2, 18% (9/50) of patients with abnormal stress-only images underwent early cardiac revascularization (within 60 days of SPECT) compared to 0.4% (5/1,247) of those with normal stress-only images (P < .001). In patients with abnormal stress-only images, the mean SSS after AC in those undergoing early cardiac revascularization (9/50) was 12.9 ± 6.3 versus 3.6 ± 3.5 in those who did not undergo early cardiac revascularization (41/50; P = .001). In the abnormal stress-rest group, 4.7% (4/86) of patients underwent early cardiac revascularization (mean AC SSS 8.6 ± 6.9) (Table 4).
Considering that a significant number of studies normalized after AC, cumulative adverse cardiac events were compared between patients with normal non-AC images and those with abnormal non-AC images which normalized with AC. A similarly low cumulative adverse cardiac event rate was observed within each normal scan group (1.2% without AC vs 0.9% with AC, P = .6; Table 5).
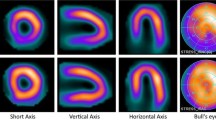
Two examples of patients who underwent cardiac catheterization and eventual revascularization based upon stress-only imaging results are shown in Figures 3 and 4. The first example (Figure 3) was a 63-year-old male with a history of chest pain but no previous CAD. After AC, a medium-size inferior and inferolateral perfusion abnormality persisted. ECG-gated SPECT imaging demonstrated normal wall motion. At catheterization, a 70% stenosis in the first circumferential marginal branch was noted with subsequent successful revascularization. A second example (Figure 4) was a 62-year-old male who also presented with chest pain and no history of CAD. After AC, a medium sized, mid and basal inferior defect of moderate to severe intensity was present with mild hypokinesis by ECG gating. At catheterization, a 90% proximal right coronary artery stenosis was identified with successful revascularization.
Example 1 of abnormal stress-only imaging in which subsequent cardiac catheterization occurred: Non-AC images are on top and AC images on bottom for short axis, vertical long axis, and horizontal axis. A medium inferior and inferolateral defect is present with moderate to severe reduction of activity and little change with AC
Example 2 of abnormal stress-only imaging in which subsequent cardiac catheterization occurred: Non-AC images are on top and AC images on bottom for short axis, vertical long axis, and horizontal axis. A medium inferior and septal defect is present with moderate to severe reduction of activity and little change with AC
Discussion
The concept of stress-only SPECT imaging has gained considerable momentum as a means of improving laboratory efficiency and reducing radiation exposure for selected patients.1,2 In order for this strategy to be successful, rest imaging should be minimized, and the results (either normal or abnormal) carry appropriate risk of future cardiac events. Previous stress-only studies without AC have suggested the necessity for rest imaging to be as high as 50%-78%, rendering the procedure inefficient.3,6,11 The American Society of Nuclear Cardiology has concluded in recent statements that the best use of a stress-only imaging strategy is likely to be in a population for whom it is anticipated that the stress study would be normal, or if abnormal, a clinical decision could be made without a rest study.12 This society has also recognized a need for additional studies addressing clinical outcomes of patients undergoing stress-only imaging.13 Two recent editorials emphasized the societal need for stress-only imaging.14,15
To this end, we examined 1,383 patients who were scheduled for clinically indicated stress-only imaging with Tc-99m AC SPECT and were successfully followed for cardiovascular-related procedures and outcomes. Without AC, less than half of the studies were considered normal. With AC, a high percentage of the studies were interpreted as normal.
During follow-up, the incidence of adverse cardiac outcomes (cardiac death or non-fatal MI) within the entire cohort was very low (0.9%). In a substantial proportion of patients, clinicians were able to make management decisions based upon attenuation-corrected stress imaging data alone with a very low percentage requiring a rest study. A considerable proportion of patients with abnormal stress images after AC underwent early cardiac revascularization without the need for additional rest imaging. Thus, our findings confirm that stress-only imaging with AC is a reasonable strategy for evaluating selected patients with symptoms suggestive of myocardial ischemia.
The group of patients with abnormal stress only imaging results also had similarly low adverse cardiovascular outcomes (1.4% cumulative MI or cardiac death). This is most likely explained by the fact that aggressive medical therapy with or without revascularization therapy instituted after identification of coronary disease in this patient population resulted in favorable short-term follow-up outcomes.
Recent studies examining stress-only imaging in selected patients continue to provide documentation of its clinical value, especially in those with normal scans.1,5-7 This report emphasizes two important additional findings: first, the inherent value of AC which results in very few patients requiring additional rest imaging and second, the confidence of physicians in that if the stress image is abnormal, clinical decisions often can be made without an additional rest scan (high cardiac revascularization rate in patients with abnormal stress-only images).
Reducing radiation exposure during imaging studies has been an ongoing issue. The American Society of Nuclear Cardiology in collaboration with other organization has issued guidelines based on the principle “as low as reasonably achievable” (ALARA) policy which recommends assessing the appropriateness of stress radionuclide imaging and if appropriate, to consider procedures with the lowest radiation dose such as a stress-only protocol and NH3 with PET imaging.16 A stress-only imaging strategy reduces the effective radiation dose from 9.3 to 11.3 mSv range for a traditional same day rest-stress Tc-99m sestamibi or tetrofosmin study to the 6.6-8 mSv range.17
Gibson et al6 in their outcome study of stress-only imaging in 652 patients demonstrated that 37% of the non-AC images had significant breast and diaphragmatic artifact and all these were eliminated with AC. Bateman et al18 in their study applying line source AC to half time stress-only imaging demonstrated no difference in image quality and diagnostic accuracy emphasizing the necessity of AC in stress-only imaging. This study provides further confirmation that AC is an important requirement for the successful implementation of a stress-only imaging protocol in routine clinical practice.
Our findings as well as those from previous studies1,5-7 demonstrate that normal AC stress-only imaging is associated with a very low incidence of short-term cardiac events (>11,722 patients in aggregate, including 1,247 from this study, Table 6) and suggests that such patients do not need to undergo additional rest imaging.
The feasibility of stress-only imaging has also been demonstrated to be very effective in an emergency room chest pain unit19 as well as in preoperative risk assessment for bariatric surgery.20 A recent study by Ryan et al21 suggests that rest images from prior studies can be effectively used in conjunction with more recent stress-only imaging in certain patient populations.
As there is no reference image for comparison, concern has been expressed that this approach may miss patients with balanced ischemia, in whom transient ischemic dilation in the absence of perfusion abnormalities is a marker of adverse cardiac outcome. The very low adverse cardiac event rate we have observed in a large number of patients argues that the incidence of balanced ischemia is minimal in patients selected for stress-only imaging (Table 6).
Selection Process for Stress-Only Imaging
The patients selected for stress-only imaging generally did not include those with a history of CABG or prior MI, based upon the assumption that such patients were more likely to require rest imaging for clinical decision-making. Thus, stress-only imaging might best be confined to patients without such histories, and not be the procedure for every patient in the laboratory. Table 1 delineates the general considerations we follow in our lab for utilizing a stress-only versus a rest-stress protocol. This selected approach has also been suggested by the recent information statements from the American Society of Nuclear Cardiology.13
Limitations
The clinical interpretations were not blinded and both AC and non-AC data were provided to referring clinicians. A SSS > 0 was considered abnormal for both non-AC and AC images for the purpose of this study based on a previous study by Baghdasarian et al.10 We feel this threshold is justified as even small abnormalities, likely due to attenuation artifact, may require rest imaging. Therefore, completely normal perfusion is an important prerequisite for effectively utilizing a stress-only protocol. The decision for additional rest imaging as well as cardiac catheterization in our study was made by physicians and was not protocol-driven.
Approximately 8% of the patients who were scheduled for stress-only imaging was lost to follow-up. Demographic characteristics and the risk profile of these patients, however, were very similar to those in whom follow-up was complete (Table 7). Thus, it is unlikely that this degree of lost follow-up would have altered the study findings. Finally, there is a lack of comparator group in this study. A controlled, study whereby patients are randomized to either a stress-only or a conventional rest-stress imaging protocol is needed to confirm our findings. Previous outcomes data from Chang et al1 did compare follow-up results between stress-only and rest-stress imaged patients and reported similar findings.
Conclusion
A strategy of stress-only imaging with AC in symptomatic patients is an efficient method which appropriately identifies at risk and low-risk patients yielding a low percentage requiring rest imaging. Clinical decisions can be made based on abnormal stress-only imaging without further rest imaging if clinically appropriate.
References
Chang SM, Nabi F, Xu J, Raza U, Mahmarian JJ. Normal stress-only versus standard stress/rest myocardial perfusion imaging: Similar patient mortality with reduced radiation exposure. J Am Coll Cardiol 2009;55:221-30.
Iskandrian AE. Stress-only myocardial perfusion imaging a new paradigm. J Am Coll Cardiol 2010;55:231-3.
Heller GV, Bateman TM, Johnson LL, et al. Clinical value of attenuation correction in stress-only Tc-99m sestamibi SPECT imaging. J Nucl Cardiol 2004;11:273-81.
Thompson RC, Heller GV, Johnson LL, et al. Value of attenuation correction on ECG-gated SPECT myocardial perfusion imaging related to body mass index. J Nucl Cardiol 2005;12:195-202.
Duvall WL, Wijetunga MN, Klein TM, et al. The prognosis of a normal stress-only Tc-99m myocardial perfusion imaging study. J Nucl Cardiol 2010;17:370-7.
Gibson PF, Demus D, Noto R, Hudson W, Johnson LL. Low event rate for stress-only perfusion imaging in patients evaluated for chest pain. J Am Coll Cardiol 2002;39:999-1004.
Gal R, Ahmad M. Cost-saving approach to normal technetium-99m sestamibi myocardial perfusion scan. Am J Cardiol 1996;78:1047-9.
Diamond GA, Forrester JS. Analysis of probability as an aid in the clinical diagnosis of coronary-artery disease. N Eng J Med 1979;300:1350-8.
Cerqueria MD, Weissman NJ, Dilsizian V, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart: A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 2002;105:539-42.
Baghdasarian SB, Noble GL, Ahlberg AW, Katten D, Heller GV. Risk stratification with attenuation corrected stress Tc-99m sestamibi SPECT myocardial perfusion imaging in the absence of ECG-gating due to arrhythmias. J Nucl Cardiol 2009;16:533-9.
Schroeder-Tanka JM, Tiel-van Buul MM, van der Wall EE, Roolker W, Lie KI, van Royen EA. Should imaging at stress always be followed by imaging at rest in Tc-99m MIBI SPECT? A proposal for a selective referral and imaging strategy. Int J Card Imaging 1997;13:323-9.
Mieres JH. JNC Prez Page. J Nucl Cardiol 2009;16:1008-10.
Des Prez RD, Dahlberg ST, Einstein AJ, et al. ASNC clinical update: Stress-only myocardial perfusion imaging. J Nuc Cardiol 2009;16:329-31.
Mahmarian JJ. Stress only myocardial perfusion imaging: Is it time for a change? J Nucl Cardiol 2010;17:529-35.
Bhavnani SP, Heller GV. Stress-only myocardial perfusion imaging. it is time for a change! J Nucl Cardiol 2011;18:836-9.
Cerqueira MD, Allman KC, Ficaro EP, Hansen CL, Nichols KJ, Thompson RC, et al. Recommendations for reducing radiation exposure in myocardial perfusion imaging. J Nucl Cardiol 2010;17:709-18.
Einstein AJ, Moser KW, Thompson RC, Cerqueira MD, Henzlova MJ. Radiation dose to patients from cardiac diagnostic imaging. Circulation 2007;116:1290-305.
Bateman TM, Heller GV, McGhie AI, Courter SA, Golub RA, Case JA, et al. Multicenter investigation comparing a highly efficient half-time stress-only attenuation correction approach against standard rest-stress Tc-99m SPECT imaging. J Nucl Cardiol 2009;16:726-35.
Duvall WL, Wijetunga MN, Klein TM, Hingorani R, Bewley B, Khan SM, Stress-only Tc-99m myocardial perfusion imaging in an emergency department chest pain unit. J Emerg Med 2011, Aug 27.
Gemignani AS, Muhlebach SG, Abbott BG, Roye GD, Harrington DT, et al. Stress-only or stress/rest myocardial perfusion imaging in patients undergoing evaluation for bariatric surgery. J Nucl Cardiol 2011;18:886-92.
Ryan JJ, Mehta R, Thiruvoipati T, Ward RP, Williams KA. Stress-only imaging in patients with prior SPECT MPI: A simulation study. J Nucl Cardiol 2012;19:311-8.
Disclosure
Investigator initiated research grant, Philips Medical Systems, San Jose, CA.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mathur, S., Heller, G.V., Bateman, T.M. et al. Clinical value of stress-only Tc-99m SPECT imaging: Importance of attenuation correction. J. Nucl. Cardiol. 20, 27–37 (2013). https://doi.org/10.1007/s12350-012-9633-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-012-9633-7