Abstract
Objectives
Anterior cruciate ligament (ACL) rupture is a common injury and has a non-union rate of 40–100%. Important cellular events, such as fibroblast proliferation, angiogenesis and change in collagen fibril thickness in the ACL remnant, as described in other dense connective tissue, might have an implication in graft recovery following ACL reconstruction. Thus we conducted a study with an aim to characterize the ultrastructural and histological features of ruptured ACL tibial stump and correlate the same with the duration of injury.
Materials and methods
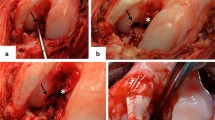
This was a prospective observational study in which 60 ruptured human ACLs were evaluated for collagen fibril thickness, blood vessel density (per mm2) and fibroblast density (per mm2) with the help of transmission electron microscopy, immunohistochemistry via CD34 antibody staining and light microscopy (H&E staining). The findings were correlated with duration of injury.
Results
Fifty-four male and six female patients with a mean duration of the injury of 23.01 weeks (SD = 26.09; range 2–108 weeks) were included for the study and were divided on the basis of duration of injury as follows: Group I (≤ 6 weeks; N = 16), Group II (7–12 weeks; N = 18), Group III (13–20 weeks; N = 7), Group IV (21–50 weeks; N = 12), Group V (> 50 weeks; N = 7). A significant correlation was seen with blood vessel density (r = 0.303, p = 0.01) and fibroblast density (r = − 0.503, p = 0.001). Thickness of collagen fibril did not correlate with the duration of injury (r = 0.15, p = 0.23). The thickness of the collagen reached its peak after 50 weeks following injury, whereas highest density of blood vessel and fibroblast was seen at 12–20 weeks. Matched pair analysis revealed a significant decrease in collagen fibril thickness and an increase in fibroblast density at 7–12 weeks.
Conclusion
Following injury to ACL, the ruptured tibial stump undergoes a series of changes at the cellular level vis-à-vis changes in collagen fibril thickness, vascular density and fibroblast density that possibly suggest an intrinsic healing response. This further may have implications on the functional outcome following ACL reconstruction with remnant preservation.
Level of evidence
III






Similar content being viewed by others
References
Mastrangelo AN, Haus BM, Vavken P, Palmer MP, Machan JT, Murray MM (2010) Immature animals have higher cellular density in the healing anterior cruciate ligament than adolescent or adult animals. J Orthop Res Off Publ Orthop Res Soc 28(8):1100–1106
Feagin JA, Curl WW (1976) Isolated tear of the anterior cruciate ligament: 5-year follow-up study. Am J Sports Med 4(3):95–100
Murray MM, Martin SD, Martin TL, Spector M (2000) Histological changes in the human anterior cruciate ligament after rupture. J Bone Joint Surg Am 82-A(10):1387–1397
Neurath MF, Printz H, Stofft E (1994) Cellular ultrastructure of the ruptured anterior cruciate ligament. A transmission electron microscopic and immunohistochemical study in 55 cases. Acta Orthop Scand 65(1):71–76
Everhart JS, Sojka JH, Kaeding CC, Bertone AL, Flanigan DC (2017) The ACL injury response: a collagen-based analysis. Knee 24(3):601–607
Frank C, McDonald D, Shrive N (1997) Collagen fibril diameters in the rabbit medial collateral ligament scar: a longer term assessment. Connect Tissue Res 36(3):261–269
Dodds JA, Arnoczky SP (1994) Anatomy of the anterior cruciate ligament: a blueprint for repair and reconstruction. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc 10(2):132–139
Arnoczky SP (1985) Blood supply to the anterior cruciate ligament and supporting structures. Orthop Clin North Am 16(1):15–28
Colombet P, Dejour D, Panisset J-C, Siebold R, French Arthroscopy Society (2010) Current concept of partial anterior cruciate ligament ruptures. Orthop Traumatol Surg Res OTSR 96(8 Suppl):S109–S118
Adachi N, Ochi M, Uchio Y, Iwasa J, Ryoke K, Kuriwaka M (2002) Mechanoreceptors in the anterior cruciate ligament contribute to the joint position sense. Acta Orthop Scand 73(3):330–334
Lee BI, Min KD, Choi HS, Kwon SW, Chun DI, Yun ES et al (2009) Immunohistochemical study of mechanoreceptors in the tibial remnant of the ruptured anterior cruciate ligament in human knees. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 17(9):1095–1101
Murray MM, Martin SD, Spector M (2000) Migration of cells from human anterior cruciate ligament explants into collagen-glycosaminoglycan scaffolds. J Orthop Res Off Publ Orthop Res Soc 18(4):557–564
Chambat P, Guier C, Sonnery-Cottet B, Fayard J-M, Thaunat M (2013) The evolution of ACL reconstruction over the last fifty years. Int Orthop 37(2):181–186
Yasuda K, Kondo E, Kitamura N, Kawaguchi Y, Kai S, Tanabe Y (2012) A pilot study of anatomic double-bundle anterior cruciate ligament reconstruction with ligament remnant tissue preservation. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc 28(3):343–353
Lee B-I, Kwon S-W, Kim J-B, Choi H-S, Min K-D (2008) Comparison of clinical results according to amount of preserved remnant in arthroscopic anterior cruciate ligament reconstruction using quadrupled hamstring graft. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc 24(5):560–568
Nambirajan A, Sharma MC, Gupta RK, Suri V, Singh M, Sarkar C (2014) Study of stem cell marker nestin and its correlation with vascular endothelial growth factor and microvascular density in ependymomas. Neuropathol Appl Neurobiol 40(6):714–725
Nguyen DT, Ramwadhdoebe TH, van der Hart CP, Blankevoort L, Tak PP, van Dijk CN (2014) Intrinsic healing response of the human anterior cruciate ligament: an histological study of reattached ACL remnants. J Orthop Res Off Publ Orthop Res Soc 32(2):296–301
Asgari M, Latifi N, Heris HK, Vali H, Mongeau L (2017) In vitro fibrillogenesis of tropocollagen type III in collagen type I affects its relative fibrillar topology and mechanics. Sci Rep 7(1):1392
Robins SP, Milne G, Duncan A, Davies C, Butt R, Greiling D et al (2003) Increased skin collagen extractability and proportions of collagen type III are not normalized after 6 months healing of human excisional wounds. J Invest Dermatol 121(2):267–272
Murray MM, Spector M (1999) Fibroblast distribution in the anteromedial bundle of the human anterior cruciate ligament: the presence of α-smooth muscle actin-positive cells. J Orthop Res 17(1):18–27
Li B, Wang JH-C (2011) Fibroblasts and myofibroblasts in wound healing: force generation and measurement. J Tissue Viability 20(4):108–120
Ekdahl M, Wang JH-C, Ronga M, Fu FH (2008) Graft healing in anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 16(10):935–947
Fratzl P, Misof K, Zizak I, Rapp G, Amenitsch H, Bernstorff S (1998) Fibrillar structure and mechanical properties of collagen. J Struct Biol 122(1–2):119–122
Parry DA, Barnes GR, Craig AS (1978) A comparison of the size distribution of collagen fibrils in connective tissues as a function of age and a possible relation between fibril size distribution and mechanical properties. Proc R Soc Lond B Biol Sci 203(1152):305–321
Komuro T (1990) Re-evaluation of fibroblasts and fibroblast-like cells. Anat Embryol (Berl) 182(2):103–112
Regan MC, Kirk SJ, Wasserkrug HL, Barbul A (1991) The wound environment as a regulator of fibroblast phenotype. J Surg Res 50(5):442–448
Andersen RB, Gormsen J (1970) Fibrin dissolution in synovial fluid. Acta Rheumatol Scand 16(4):319–333
Wu B, Zhao Z, Li S, Sun L (2013) Preservation of remnant attachment improves graft healing in a rabbit model of anterior cruciate ligament reconstruction. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc 29(8):1362–1371
Bray RC, Leonard CA, Salo PT (2002) Vascular physiology and long-term healing of partial ligament tears. J Orthop Res Off Publ Orthop Res Soc 20(5):984–989
Scranton PE, Lanzer WL, Ferguson MS, Kirkman TR, Pflaster DS (1998) Mechanisms of anterior cruciate ligament neovascularization and ligamentization. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc 14(7):702–716
Bray RC, Leonard CA, Salo PT (2003) Correlation of healing capacity with vascular response in the anterior cruciate and medial collateral ligaments of the rabbit. J Orthop Res Off Publ Orthop Res Soc 21(6):1118–1123
Gohil S, Annear PO, Breidahl W (2007) Anterior cruciate ligament reconstruction using autologous double hamstrings: a comparison of standard versus minimal debridement techniques using MRI to assess revascularisation. A randomised prospective study with a one-year follow-up. J Bone Joint Surg Br 89(9):1165–1171
Unterhauser FN, Bail HJ, Höher J, Haas NP, Weiler A (2003) Endoligamentous revascularization of an anterior cruciate ligament graft. Clin Orthop 414:276–288
Löcherbach C, Zayni R, Chambat P, Sonnery-Cottet B (2010) Biologically enhanced ACL reconstruction. Orthop Traumatol Surg Res OTSR 96(7):810–815
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nayak, M., Nag, H.L., Nag, T.C. et al. Ultrastructural and histological changes in tibial remnant of ruptured anterior cruciate ligament stumps: a transmission electron microscopy and immunochemistry-based observational study. Musculoskelet Surg 104, 67–74 (2020). https://doi.org/10.1007/s12306-019-00599-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12306-019-00599-x