Abstract
Background
Tendon-bone healing after rotator cuff repair occurs by fibrovascular scar tissue formation, which is weaker than a normal tendon-bone insertion site. Growth factors play a role in tissue formation and have the potential to augment soft tissue healing in the perioperative period.
Questions/purposes
Our study aim was to determine if rhPDGF-BB delivery on a collagen scaffold can improve tendon-to-bone healing after supraspinatus tendon repair compared with no growth factor in rats as measured by (1) gross observations; (2) histologic analysis; and (3) biomechanical testing.
Methods
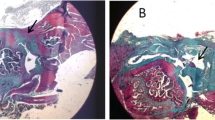
Ninety-five male Sprague-Dawley rats underwent acute repair of the supraspinatus tendon. Rats were randomized into one of five groups: control (ie, repair only), scaffold only, and three different platelet-derived growth factor (PDGF) doses on the collagen scaffold. Animals were euthanized 5 days after surgery to assess cellular proliferation and angiogenesis. The remaining animals were analyzed at 4 weeks to assess repair site integrity by gross visualization, fibrocartilage formation with safranin-O staining, and collagen fiber organization with picrosirius red staining, and to determine the biomechanical properties (ie, load-to-failure testing) of the supraspinatus tendon-bone construct.
Results
The repaired supraspinatus tendon was in continuity with the bone in all animals. At 5 days, rhPDGF-BB delivery on a scaffold demonstrated a dose-dependent response in cellular proliferation and angiogenesis compared with the control and scaffold groups. At 28 days, with the numbers available, rhPDGF-BB had no effect on increasing fibrocartilage formation or improving collagen fiber maturity at the tendon-bone insertion site compared with controls. The control group had higher tensile loads to failure and stiffness (35.5 ± 8.8 N and 20.3 ± 4.5 N/mm) than all the groups receiving the scaffold, including the PDGF groups (scaffold: 27 ± 6.4 N, p = 0.021 and 13 ± 5.7 N/mm, p = 0.01; 30 µg/mL PDGF: 26.5 ± 7.5 N, p = 0.014 and 13.3 ± 3.2 N/mm, p = 0.01; 100 µg/mL PDGF: 25.7 ± 6.1 N, p = 0.005 and 11.6 ± 3.3 N/mm, p = 0.01; 300 µg/mL PDGF: 27 ± 6.9 N, p = 0.014 and 12.7 ± 4.1 N/mm, p = 0.01).
Conclusions
rhPDGF-BB delivery on a collagen scaffold enhanced cellular proliferation and angiogenesis during the early phase of healing, but this did not result in either a more structurally organized or stronger attachment site at later stages of healing. The collagen scaffold had a detrimental effect on healing strength at 28 days, and its relatively larger size compared with the rat tendon may have caused mechanical impingement and extrinsic compression of the healing tendon. Future studies should be performed in larger animal models where healing occurs more slowly.
Clinical Relevance
Augmenting the healing environment to improve the structural integrity and to reduce the retear rate after rotator cuff repair may be realized with continued understanding and optimization of growth factor delivery systems.









Similar content being viewed by others
References
Barber FA, Burns JP, Deutsch A, Labbé MR, Litchfield RB. A prospective, randomized evaluation of acellular human dermal matrix augmentation for arthroscopic rotator cuff repair. Arthroscopy. 2012;28:8–15.
Bhargava MM, Hidaka C, Hannafin JA, Doty S, Warren RF; Laboratory for Soft Tissue Research. Effects of hepatocyte growth factor and platelet-derived growth factor on the repair of mensical defects in vitro. In Vitro Cell Dev Biol Anim. 2005;41:305–310.
Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am. 2005;87:1229–1240.
Carpenter JE, Thomopoulos S, Flanagan CL, DeBano CM, Soslowsky LJ. Rotator cuff defect healing: a biomechanical and histologic analysis in an animal model. J Shoulder Elbow Surg. 1998;7:599–605.
Chan BP, Fu SC, Qin L, Rolf C, Chan KM. Supplementation-time dependence of growth factors in promoting tendon healing. Clin Orthop Relat Res. 2006;448:240–247.
Chen RR, Silva EA, Yuen WW, Brock AA, Fischback C, Lin AS, Guldberg RE, Mooney DJ. Integrated approach to designing growth factor delivery systems. FASEB J. 2007;21:3896–3903.
Chen RR, Silva EA, Yuen WW, Mooney DJ. Spatio-temporal VEGF and PDGF delivery patterns blood vessel formation and maturation. Pharm Res. 2007;24:258–264.
Cohen DB, Kawamura S, Ehteshami JR, Rodeo SA. Indomethacin and celecoxib impair rotator cuff tendon-to-bone healing. Am J Sports Med. 2006;34:362–369.
Coons DA, Barber AF. Tendon graft substitutes—rotator cuff patches. Sports Med Arthrosc. 2006;14:185–190.
Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86:219–224.
Gazielly DF, Gleyze P, Montagnon C. Functional and anatomical results after rotator cuff repair. Clin Orthop Relat Res. 1994;304:43–53.
Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2000;82:505–515.
Gerber C, Schneeberger AG, Perren SM, Nyffeler RW. Experimental rotator cuff repair: a preliminary study. J Bone Joint Surg Am. 1999;81:1281–1290.
Harryman DT, Mack LA, Wang KY, Jackins SE, Richardson ML, Matsen FA. Repairs of the rotator cuff: correlation of functional results with integrity of the cuff. J Bone Joint Surg Am. 1991;73:982–989.
Hee CK, Dines JS, Dines DM, Roden CM, Wisner-Lynch LA, Turner AS, McGilvray KC, Lyons AS, Puttlitz CM, Santoni BG. Augmentation of a rotator cuff suture repair using rhPDGF-BB and a type I bovine collagen matrix in an ovine model. Am J Sports Med. 2011;39:1630–1639.
Hildebrand KA, Woo SL, Smith DW, Allen CR, Deie M, Taylor BJ, Schmidt CC. The effects of platelet-derived growth factor-BB on healing of the rabbit medial collateral ligament. Am J Sports Med. 1998;26:549–554.
Iannotti JP, Codsi MJ, Kwon YW, Derwin K, Ciccone J, Brems JJ. Porcine small intestine submucosa augmentation of surgical repair of chronic two-tendon rotator cuff tears: a randomized, controlled trial. J Bone Joint Surg Am. 2006;88:1238–1244.
Kobayashi M, Itoi E, Minagawa H, Miyakoshi N, Takahashi S, Tuoheti Y, Okada K, Shimada Y. Expression of growth factors in the early phase of supraspinatus tendon healing in rabbits. J Shoulder Elbow Surg. 2006;15:371–377.
Koike Y, Trudel G, Curran D, Uhthoff HK. Delay of supraspinatus repair by up to 12 weeks does not impair enthesis formation: a quantitative histologic study in rabbits. J Orthop Res. 2006;24:202–210.
Kong HJ, Kim ES, Huang YC, Mooney DJ. Design of biodegradable hydrogel for the local and sustained delivery of angiogenic plasmid DNA. Pharm Res. 2008;25:1230–1238.
Kondo E, Yasuda K, Yamanaka M, Minami A, Tohyama H. Effects of administration of exogenous growth factors on biomechanical properties of the elongation-type anterior cruciate ligament injury with partial laceration. Am J Sports Med. 2005;33:188–196.
Letson AK, Dahners LE. The effect of combinations of growth factors on ligament healing. Clin Orthop Relat Res. 1994;308:207–212.
Nakamura N, Shino K, Natsuume T, Horibe S, Matsumoto N, Kaneda Y, Ochi T. Early biological effect of in vivo gene transfer of platelet-derived growth factor (PDGF)-B into healing patellar ligament. Gene Ther. 1998;5:1165–1170.
Rodeo SA, Potter HG, Kawamura S, Turner AS, Kim HJ, Atkinson BL. Biologic augmentation of rotator cuff tendon healing using a mixture of osteoinductive growth factors: an experimental study in sheep. J Bone Joint Surg Am. 2007;89:2485–2497.
Soslowsky LJ, Carpenter JE, DeBano CM, Banerji I, Moalli MR. Development and use of an animal model for investigations on rotator cuff disease. J Shoulder Elbow Surg. 1996;5:383–392.
Soslowsky LJ, Thomopoulos S, Esmail A, Flanagan CL, Iannotti JP, Williamson JD 3rd, Carpenter JE. Rotator cuff tendinosis in an animal model: role of extrinsic and overuse factors. Ann Biomed Eng. 2002;30:1057–1063.
Tallquist M, Kazlauskas A. PDGF signaling in cells and mice. Cytokine Growth Factor Rev. 2004;15:205–213.
Uggen JC, Dines J, Uggen CW, Mason JS, Razzano P, Dines D, Grande DA. Tendon gene therapy modulates the local repair environment in the shoulder. J Am Osteopath Assoc. 2005;105:20–21.
Uhthoff HK, Sano H, Trudel G, Ishii H. Early reactions after reimplantation of the tendon of supraspinatus into bone: a study in rabbits. J Bone Joint Surg Br. 2000;82:1072–1076.
Wang XT, Liu PY, Tang JB. Tendon healing in vitro: genetic modification of tenocytes with exogenous PDGF gene and promotion of collagen gene expression. J Hand Surg. 2004;29:884–890.
Weiler A, Förster C, Hunt P, Falk R, Jung T, Unterhauser FN, Bergmann V, Schmidmaier G, Haas NP. The influence of locally applied platelet-derived growth factor-BB on free tendon graft remodeling after anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32:881–891.
Acknowledgments
We acknowledge Stephen Goldman PhD, for providing the collagen sponge material (ie, Type I collagen scaffold) from Kensey Nash, Inc (Exton, PA, USA). We also thank Ran Stark MD, for his assistance with the animal surgeries.
Author information
Authors and Affiliations
Corresponding author
Additional information
The institution of one of the authors (SAR) has received less than USD 10,000, in any one year, funding from BioMimetic Therapeutics, Inc (Franklin, TN, USA). One or more of the authors is a paid consultant for Biomet (Warsaw, IN, USA) (LVG) and Smith & Nephew (Memphis, TN, USA) (SAR), has stock or stock options in Cayenne Medical (Scottsdale, AZ, USA) (SAR), and is on the medical/orthopaedic publications editorial/governing board of the HSS Journal (LVG).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the animal protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the Hospital for Special Surgery, New York, NY, USA.
About this article
Cite this article
Kovacevic, D., Gulotta, L.V., Ying, L. et al. rhPDGF-BB Promotes Early Healing in a Rat Rotator Cuff Repair Model. Clin Orthop Relat Res 473, 1644–1654 (2015). https://doi.org/10.1007/s11999-014-4020-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-014-4020-0