Opinion statement
Acute myeloid leukemia (AML) patients with a complex karyotype (CK-AML) show at least 3 unrelated clonal cytogenetic abnormalities with notoriously poor outcome. Such cases fall into either AML with myelodysplasia-related changes or therapy-related AML in the current World Health Organization classification of AML. Allogeneic stem cell transplantation is one of the only treatment modalities that can provide a long-term survival benefit and is recommended as a consolidative treatment in patients who are able to achieve complete remission. Unfortunately, transplantation is also associated with a higher relapse rate and more than half of CK-AML patients relapse from disease within the first 2 years. The probability of achieving remission with traditional induction using cytarabine and daunorubicin or idarubicin (“7 + 3”) is so small that investigational therapies should be considered up front in these patients. Less intensive therapeutic backbones, typically using one of the hypomethylating agents, azacitidine or decitabine, minimize toxicity and show a trend toward the improved overall survival. CPX 351 (Vyxeos) is a liposomal formulation of cytarabine and daunorubicin and this encapsulation leads to prolonged exposure to the two drugs. This drug is approved for AML patients with MDS-related changes and therapy-related AML, both of which are frequently associated with complex karyotype. Such patients show improved outcome in trials using this combination. Combination therapy that includes venetoclax (BCL2 inhibitor) with hypomethylating agents may also be appropriate for such patients.
Similar content being viewed by others
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Rubnitz JE, Gibson B, Smith FO. Acute myeloid leukemia. Pediatr Clin N Am. 2008;55(1):21–51.
Haferlach T, Kern W, Schnittger S, Schoch C. Modern diagnostics in acute leukemias. Crit Rev Oncol Hematol. 2005;56(2):223–34.
Haferlach T, Schoch C. Moderne Verfahren in der Leukämiediagnostik. Internist. 2002;43(10):1190–202.
• Mrózek K. Cytogenetic, molecular genetic, and clinical characteristics of acute myeloid leukemia with a complex karyotype. Semin Oncol. 2008;35(4):365–77 Overview of complex karyotype definitions and clinical features of AML patients with complex karyotype.
Jaffe ES. Pathology and genetics of tumours of haematopoietic and lymphoid tissues. In: Iarc; 2001.
Orozco JJ, Appelbaum FR. Unfavorable, complex, and monosomal karyotypes: the most challenging forms of acute myeloid leukemia. Oncology. 2012;26(8):706–12.
• Grimwade D, Hills RK, Moorman AV, Walker H, Chatters S, et al. National Cancer Research Institute Adult Leukaemia Working Group. Refinement of cytogenetic classification in acute myeloid leukemia: determination of prognostic significance of rare recurring chromosomal abnormalities among 5876 younger adult patients treated in the United Kingdom Medical Research Council trials. Blood. 2010;116(3):354–65 Cytogenetic classification in AML based on a large MRC trial.
Meng CY, Noor PJ, Ismail A, Ahid MF, Zakaria Z. Cytogenetic profile of de novo acute myeloid leukemia patients in Malaysia. Int J Biomed Sci. 2013;9(1):26.
Trivedi PJ, Patel DM, Brahmbhatt MM, Patel PS. Characterization of complex chromosomal rearrangements in acute myeloid leukemia: FISH and multicolor FISH add precision in defining abnormalities associated with poor prognosis. J Blood Res Hematol Dis. 2016;1(2). https://doi.org/10.4172/jbrhd.1000104.
•• Mrózek K, Marcucci G, Nicolet D, Maharry KS, Becker H, Whitman SP, et al. Prognostic significance of the European LeukemiaNet standardized system for reporting cytogenetic and molecular alterations in adults with acute myeloid leukemia. J Clin Oncol. 2012;30(36):4515 ELN recommendations for reporting genetic abnormalities in AML.
Röllig C, Bornhäuser M, Thiede C, Taube F, Kramer M, Mohr B, et al. Long-term prognosis of acute myeloid leukemia according to the new genetic risk classification of the European LeukemiaNet recommendations: evaluation of the proposed reporting system. J Clin Oncol. 2011;29(20):2758–65.
Grimwade D, Walker H, Harrison G, Oliver F, Chatters S, Harrison CJ, et al. The predictive value of hierarchical cytogenetic classification in older adults with acute myeloid leukemia (AML): analysis of 1065 patients entered into the United Kingdom Medical Research Council AML11 trial. Blood. 2001;98(5):1312–20.
• Slovak ML, Kopecky KJ, Cassileth PA, Harrington DH, Theil KS, Mohamed A, et al. Karyotypic analysis predicts outcome of preremission and postremission therapy in adult acute myeloid leukemia: a Southwest Oncology Group/Eastern Cooperative Oncology Group Study. Blood. 2000;96(13):4075–83 SWOG trial reported importance of karyotype analysis on outcome of preremission and postremission therapy in AML patients.
Appelbaum FR, Kopecky KJ, Tallman MS, Slovak ML, Gundacker HM, Kim HT, et al. The clinical spectrum of adult acute myeloid leukaemia associated with core binding factor translocations. Br J Haematol. 2006;135(2):165–73.
Burnett A, Wetzler M, Lowenberg B. Therapeutic advances in acute myeloid leukemia. J Clin Oncol. 2011;29(5):487–94.
Bae SY, Kim JS, Ryeu BJ, Lee KN, Lee CK, Kim YK, et al. Acute myeloid leukemia (AML-M2) associated with variant t (8; 21): report of three cases. Cancer Genet Cytogenet. 2010;199(1):31–7.
Park J, Jurcic JG, Rosenblat T, Tallman MS. Emerging new approaches for the treatment of acute promyelocytic leukemia. Ther Adv Hematol. 2011;2(5):335–52.
Bakshi SR, Brahmbhatt MM, Trivedi PJ, Dalal EN, Patel DM, Purani SS, et al. Trisomy 8 in leukemia: a GCRI experience. Indian J Hum Genet. 2012;18(1):106.
Greer JP, Arber DA, Glader B, List AF, Means RT, Paraskevas, et al. Wintrobe’s clinical hematology: Thirteen ed. Philadelphia. Lippincott Williams & Wilkins, a Wolters Kluwer business; cytogenetics. 2013; chapter 3: p.52.
Wiktor A, Rybicki BA, Piao ZS, Shurafa M, Barthel B, Maeda K, et al. Clinical significance of Y chromosomeloss in hematologic disease. Genes Chromosom Cancer. 2000;27(1):11–6.
United KC. Loss of the Y chromosome from normal and neoplastic bone marrows. Genes Chromosom Cancer. 1992;5:83–8.
Bilhou-Nabera C. 12p abnormalities in myeloid malignancies. Atlas Genet Cytogenet Oncol Haematol. 1998;2(4):125–6.
Hosono N, Makishima H, Mahfouz R, Przychodzen B, Yoshida K, Jerez A, et al. Recurrent genetic defects on chromosome 5q in myeloid neoplasms. Oncotarget. 2017;8(4):6483.
Zhang R. Kim Y2, Wang X, Li Y, Lu X, Sternenberger AR, Li S, Lee JY. Genomic copy number variations in the myelodysplastic syndrome and acute myeloid leukemia patients with del(5q) and/or -7/del(7q). Int J Med Sci. 2015;12(9):719–26.
Appelbaum FR, Gundacker H, Head DR, Slovak ML, Willman CL, Godwin JE, et al. Age andacute myeloid leukemia. Blood. 2006;107(9):3481–5.
Desangles F. 7/del(7q) in adults. Atlas Genet Cytogenet Oncol Haematol. 1999;3(3):139–40.
De Braekeleer E, Douet-Guilbert N, Basinko A, Bovo C, Gueganic N, Le Bris MJ, et al. Conventional cytogenetics and breakpoint distribution by fluorescent in situ hybridization in patients with malignant hemopathies associated with inv.(3)(q21;q26) and t(3;3)(q21;q26). Anticancer Res. 2011;31(10):3441–8.
Balgobind BV, Raimondi SC, Harbott J, Zimmermann M, Alonzo TA, Auvrignon A, et al. Novel prognostic subgroups in childhood 11q23/MLLrearranged acute myeloid leukemia: results of an international retrospective study. Blood. 2009;114(12):2489–96.
Chen Y, Kantarjian H, Pierce S, Faderl S, O’Brien S, Qiao W, et al. Prognostic significance of 11q23 aberrations in adult acute myeloid leukemia and the role of allogeneic stem cell transplantation. Leukemia. 2013;27(4):836.
Krauter J, Wagner K, Schafer I, Marschalek R, Meyer C, Heil G, et al. Prognostic factors in adult patients up to 60 years old with acute myeloid leukemia and translocations of chromosome band 11q23: individual patient data-based meta-analysis of the German Acute Myeloid Leukemia Intergroup. J Clin Oncol. 2009;27(18):3000–6.
•• Swerdlow S, Campo E, Harris N, Jaffe E, Pileri S, Stein H, et al., editors. World Health Organization classification of tumours of haematopoietic and lymphoid tissues. 4th ed. Lyons: IARC Press; 2008. WHO classification of hematologic malignancies.
Arsham MS, Barch MJ, Lawce HJ. (Eds.) The AGT Cytogenetics Laboratory Manual, 4th ed. John Wiley & Sons, Hoboken, NJ. 2017.
Labis E. t(11;16)(q23;p13.3). Atlas Genet Cytogenet Oncol Haematol. 2009. http://AtlasGeneticsOncology.org/Anomalies/t1116q23p13ID1120.html.
Fleischman EW, Reshmi S, Frenkel MA, Konovalova WI, Guleva GP, Kulagina OE, et al. MLL is involved in a t(2;11)(p21;q23) in a patient with acute myeloblastic leukemia. Genes Chromosom Cancer. 1999;24(2):151–5.
Shi LH, Ma P, Liu JS, Li Y, Wang YF, Guo MF, et al. Current views of chromosomal abnormalities in pediatric acute myeloid leukemia (AML). Eur Rev Med Pharmacol Sci. 2017;21(4 Suppl):25–30.
Bilhou-Nabera C. del(20q) in myeloid malignancies. Atlas Genet Cytogenet Oncol Haematol. 2001;5(1):33–4.
Ligon AH, DeAngelo DJ, Atkins L, Dal CP. Isochromosome of a deleted 20q may be a relatively common abnormality in myeloid malignancies. Cancer Genet Cytogenet. 2005;162(1):89–91.
Wei CH, Yu IT, Tzeng CH, Fan FS, Hsieh RK, Chiou TJ, et al. Trisomy 21 in acute myeloid leukemia. Cancer Genet Cytogenet. 1996;86(2):177–80.
Slovak ML, Gundacker H, Bloomfield CD, Dewald G, Appelbaum FR, Larson RA, et al. A retrospective study of 69 patients with t(6;9)(p23;q34) AML emphasizes the need for a prospective, multicenter initiative for rare ‘poor prognosis’ myeloid malignancies. Leukemia. 2006;20(7):1295–7.
Gajendra S, Sahoo MK. Philadelphia-positive acute myeloblastic leukemia: a rare entity. J Neoplasm. 2016;1:1.
Espersen AD, Noren, Nyström U, Abrahamsson J, Ha SY, Pronk CJ, et al. Acute myeloid leukemia (AML) with t (7; 12)(q36; p13) is associated with infancy and trisomy 19: data from Nordic Society for Pediatric Hematology and Oncology (NOPHO-AML) and review of the literature. Genes Chromosom Cancer. 2018;57(7):359–65.
Coenen EA, Zwaan CM, Reinhardt D, Harrison CJ, Haas OA, de Haas V, et al. Pediatric acute myeloid leukemia with t (8; 16)(p11; p13): a distinct clinical and biological entity, a collaborative study by the International-Berlin-Frankfurt-Munster AML-study group. Blood. 2013;122:2704–13.
Bernstein J, Dastugue N, Haas OA, Harbott J, Heerema NA, Huret JL, et al. Nineteen cases of the t(1;22)(p13;q13) acute megakaryblastic leukaemia of infants/children and a review of 39 cases: report from a t(1;22) study group. Leukemia. 2000;14(1):216–8.
• Breems DA, Van Putten WL, De Greef GE, et al. Monosomal karyotype in acute myeloid leukemia. A better indicator of poor prognosis than a complex karyotype. J Clin Oncol. 2008;26:4791–7. Monosomal karyotype definition and prognostic significance in AML.
Weinberg OK, Ohgami RS, Ma L, Seo K, Ren L, Gotlib JR, et al. Acute myeloid leukemia with monosomal karyotype: morphologic, immunophenotypic, and molecular findings. Am J Clin Pathol. 2014;142(2):190–5.
•• Dohner H, Estey EH, Amadori S, Appelbaum FR, Buchner T, Burnett AK, et al. Diagnosis and management of acute myeloid leukemia in adults: recommendations from an international expert panel, on behalf of the European LeukemiaNet. Blood. 2010;115:453–74 AML risk classification according to cytogenetic abnormality.
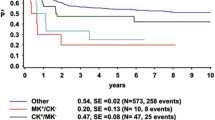
• Stölzel F, Mohr B, Kramer M, Oelschlägel U, Bochtler T, Berdel WE, et al. Karyotype complexity and prognosis in acute myeloid leukemia. Blood Cancer J. 2017;6(1):e386 First clinical study on prognostic significance of karyotype abnormalities in AML.
Göhring G, Michalova K, Beverloo HB, Betts D, Harbott J, Haas OA, et al. Complex karyotype newly defined: the strongest prognostic factor in advanced childhood myelodysplastic syndrome. Blood. 2010;116:3766–9.
Medeiros BC, Othus M, Fang M, Roulston D, Appelbaum FR. Prognostic impact of monosomal karyotype in young adult and elderly acute myeloid leukemia: the Southwest Oncology Group experience. Blood. 2010;116(13):2224–8.
Harrison CJ, Hills RK, Moorman AV, Grimwade DJ, Hann I, Webb DK, et al. Cytogenetics of childhood acute myeloid leukemia: United Kingdom Medical Research Council Treatment trials AML 10 and 12. J Clin Oncol. 2010;28(16):2674–81.
Pedersen-Bjergaard J, Andersen MK, Christiansen DH, Nerlov C. Genetic pathways in therapy-related myelodysplasia and acute myeloid leukemia. Blood. 2002;99(6):1909–12.
Perrot A, Luquet I, Pigneux A, Mugneret F, Delaunay J, Harousseau JL, et al. Dismal prognostic value of monosomal karyotype in elderly patients with acute myeloid leukemia: a GOELAMS study of 186 patients with unfavorable cytogenetic abnormalities. Blood. 2011;118(3):679–85.
Vaidya R, Caramazza D, Begna KH, et al. Monosomal karyotype in primary myelofibrosis is detrimental to both overall and leukemia-free survival. Blood. 2011;117:5612–5.
Wierzbowska A, Wawrzyniak E, Siemieniuk-Rys M, Kotkowska A, Pluta A, Golos A, et al. Concomitance of monosomal karyotype with at least 5 chromosomal abnormalities is associated with dismal treatment outcome of AML patients with complex karyotype–retrospective analysis of Polish Adult Leukemia Group (PALG). Leuk Lymphoma. 2017;58(4):889–97.
Haferlach C, Alpermann T, Schnittger S, Kern W, Chromik J, Schmid C, et al. Prognostic value of monosomal karyotype in comparison to complex aberrant karyotype in acute myeloid leukemia: a study on 824 cases with aberrant karyotype. Blood. 2012;119(9):2122–5.
Grimwade D. Impact of cytogenetics on clinical outcome in AML. In: Karp JE, editor. Acute Myelogenous Leukemia. Totowa, NJ: Humana Press. 2007;p.177–192.
Grimwade D, Hills RK. Independent prognostic factors for AML outcome. ASH Education Program Book. 2009;2009(1):385–95.
Hernandez JM, Martin G, Gutierrez NC, Cervera J, Ferro MT, Calasanz MJ, et al. Additional cytogenetic changes do not influence the outcome of patients with newly diagnosed acute promyelocytic leukemia treated with an ATRA plus anthracyclin based protocol. A report of the Spanish group PETHEMA. Haematologica. 2001;86(8):807–13.
Schlenk RF, Benner A, Krauter J, Buchner T, Sauerland C, Ehninger G, et al. Individual patient data–based meta-analysis of patients aged 16 to 60 years with core binding factor acute myeloid leukemia: a survey of the German Acute Myeloid Leukemia Intergroup. J Clin Oncol. 2004;22(18):3741–50.
Chen EC, Fathi AT, Brunner AM. Reformulating acute myeloid leukemia: liposomal cytarabine and daunorubicin (CPX-351) as an emerging therapy for secondary AML. OncoTargets Ther. 2018;11:3425.
Ohgami RS, Ma L, Merker JD, Gotlib JR, Schrijver I, Zehnder JL, et al. Next-generation sequencing of acute myeloid leukemia identifies the significance of TP53, U2AF1, ASXL1, and TET2 mutations. Mod Pathol. 2015;28(5):706.
•• Papaemmanuil E, Gerstung M, Bullinger L, Gaidzik VI, Paschka P, Roberts ND, et al. Genomic classification and prognosis in acute myeloid leukemia. N Engl J Med. 2016;374(23):2209–21 A large study on genomic classification and prognosis in AML.
Hou HA, Chou WC, Kuo YY, Liu CY, Lin LI, Tseng MH, et al. TP53 mutations in de novo acute myeloid leukemia patients: longitudinal follow-ups show the mutation is stable during disease evolution. Blood Cancer J. 2015;5(7):e331.
Fernandez-Pol S, Ma L, Ohgami RS, Arber DA. Immunohistochemistry for p53 is a useful tool to identify cases of acute myeloid leukemia with myelodysplasia-related changes that are TP53 mutated, have complex karyotype, and have poor prognosis. Mod Pathol. 2017;30(3):382.
Dombret H, Gardin C. An update of current treatments for adult acute myeloid leukemia. Blood. 2016;127(1):53–61.
Creutzig U, Van Den Heuvel-Eibrink MM, Gibson B, Dworzak MN, Adachi S, De Bont E, et al. Diagnosis and management of acute myeloid leukemia in children and adolescents: recommendations from an international expert panel. Blood. 2012;120(16):3187–205.
Döhner H, Estey E, Grimwade D, Amadori S, Appelbaum FR, Büchner T, et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood. 2017;129(4):424–47.
Ciurea SO, Labopin M, Socie G, Volin L, Passweg J, Chevallier P, et al. Relapse and survival after transplantation for complex karyotype acute myeloid leukemia: a report from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation and the University of Texas MD Anderson Cancer Center. Cancer. 2018;124(10):2134–41.
Umukoro, C. Post-transplant relapse is a main cause of treatment failure in patients with complex karyotype AML. 2018. Retrieved from https://amlglobalportal.com. Accessed 10 Sept 2018.
Dombret H, Seymour JF, Butrym A, Wierzbowska A, Selleslag D, Jang JH, et al. International phase 3 study of azacitidine vs conventional care regimens in older patients with newly diagnosed AML with >30% blasts. Blood 2015;126: 291–299.
Welch JS, Petti AA, Miller CA, Fronick CC, O’Laughlin M, Fulton RS, et al. TP53 and decitabine in acute myeloid leukemia and myelodysplastic syndromes. N Engl J Med. 2016;375(21):2023–36.
Montalban-Bravo G, Benton CB, Wang SA, Ravandi F, Kadia T, Cortes J, et al. More than 1 TP53 abnormality is a dominant characteristic of pure erythroid leukemia. Blood. 2017;129(18):2584–7.
Estey EH. Acute myeloid leukemia: 2019 update on riskstratification and management. Am J Hematol. 2018;93(10):1267–91.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Yahya Daneshbod, Leila Kohan, and Vahideh Taghadosi declare that they have no conflict of interest. Olga K. Weinberg has received compensation from Jazz Pharmaceuticals for service on an advisory board. Daniel A. Arber has received compensation from Jazz Pharmaceuticals for service on an advisory board and as a consultant.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Leukemia
Rights and permissions
About this article
Cite this article
Daneshbod, Y., Kohan, L., Taghadosi, V. et al. Prognostic Significance of Complex Karyotypes in Acute Myeloid Leukemia. Curr. Treat. Options in Oncol. 20, 15 (2019). https://doi.org/10.1007/s11864-019-0612-y
Published:
DOI: https://doi.org/10.1007/s11864-019-0612-y