Abstract
Background
Subcutaneous tissue oxygen tension (PsqO2) is a major predictor for wound healing and the occurrence of wound infections. Perioperative subcutaneous wound and tissue oxygen tension is significantly reduced in morbidly obese patients. Even during intraoperative supplemental oxygen administration, PsqO2 remains low. Tissue hypoxia is pronounced during surgery and might explain the substantial increase in infection risk in obese patients. It remains unknown whether long-term supplemental postoperative oxygen augments tissue oxygen tension. Consequently, we tested the hypothesis that 80% inspired oxygen administration during 12–18 postoperative hours significantly increases PsqO2 compared to 30% inspired oxygen fraction.
Methods
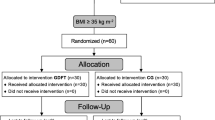
After IRB approval and informed consent, 42 patients undergoing laparoscopic bariatric surgery were randomly assigned to receive either 80% inspired oxygen via a PULMANEX Hi-Ox™ Mask (Viasys MedSystems, Wheeling, IL) (10 L/min) or 30% oxygen via nasal cannula (2 L/min) after surgery until the next morning. PsqO2 was measured with a temperature-corrected Clark-type electrode in the subcutaneous tissue of the upper arm and adjacent to the wound.
Results
Postoperative subcutaneous tissue oxygen tension was significantly increased in the Hi-Ox group: 58 (47.7, 74.1) mmHg vs. 43 (38.7, 55.2) mmHg, P = 0.002. Also, wound tissue oxygen tension was improved during supplemental oxygen administration: 75.2 (69.8, 95.5) mmHg vs. 52.4 (46.3, 66.1) mmHg, P < 0.001.
Conclusion
Subcutaneous tissue oxygen tension was significantly increased by supplemental postoperative oxygen administration. Whether there is an effect on the incidence of wound infection in morbidly obese patients is matter of further research.




Similar content being viewed by others
References
Levy BI, Schiffrin EL, Mourad JJ, et al. Impaired tissue perfusion: a pathology common to hypertension, obesity, and diabetes mellitus. Circulation. 2008;118:968–76.
de Divitiis O, Fazio S, Petitto M, et al. Obesity and cardiac function. Circulation. 1981;64:477–82.
Alpert MA. Obesity cardiomyopathy: pathophysiology and evolution of the clinical syndrome. Am J Med Sci. 2001;321:225–36.
Di Girolamo M, Skinner Jr NS, Hanley HG, et al. Relationship of adipose tissue blood flow to fat cell size and number. Am J Physiol. 1971;220:932–7.
Choban PS, Heckler R, Burge JC, et al. Increased incidence of nosocomial infections in obese surgical patients. Am Surg. 1995;61:1001–5.
Gendall KA, Raniga S, Kennedy R, et al. The impact of obesity on outcome after major colorectal surgery. Dis Colon Rectum. 2007;50:2223–37.
Babior BM. Oxygen-dependent microbial killing by phagocytes (first of two parts). N Engl J Med. 1978;298:659–68.
Hopf HW, Hunt TK, West JM, et al. Wound tissue oxygen tension predicts the risk of wound infection in surgical patients. Arch Surg. 1997;132:997–1004. discussion 5.
Greif R, Akca O, Horn EP, et al. Supplemental perioperative oxygen to reduce the incidence of surgical-wound infection Outcomes Research Group. N Engl J Med. 2000;342:161–7.
Belda FJ, Aguilera L, Garcia de la Asuncion J, et al. Supplemental perioperative oxygen and the risk of surgical wound infection: a randomized controlled trial. JAMA. 2005;294:2035–42.
Fleischmann E, Kurz A, Niedermayr M, et al. Tissue oxygenation in obese and non-obese patients during laparoscopy. Obes Surg. 2005;15:813–9.
Kabon B, Nagele A, Reddy D, et al. Obesity decreases perioperative tissue oxygenation. Anesthesiology. 2004;100:274–80.
Hiltebrand LB, Kaiser HA, Niedhart DJ, et al. Subcutaneous oxygen pressure in spontaneously breathing lean and obese volunteers: a pilot study. Obes Surg. 2008;18:77–83.
Robinson JD, Lupkiewicz SM, Palenik L, et al. Determination of ideal body weight for drug dosage calculations. Am J Hosp Pharm. 1983;40:1016–9.
Hopf HW, Viele M, Watson JJ, et al. Subcutaneous perfusion and oxygen during acute severe isovolemic hemodilution in healthy volunteers. Arch Surg. 2000;135:1443–9.
Mokdad AH, Ford ES, Bowman BA, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003;289:76–9.
Kopelman PG. Obesity as a medical problem. Nature. 2000;404:635–43.
Dindo D, Muller MK, Weber M, et al. Obesity in general elective surgery. Lancet. 2003;361:2032–5.
Choban PS, Flancbaum L. The impact of obesity on surgical outcomes: a review. J Am Coll Surg. 1997;185:593–603.
Goodson 3rd WH, Hunt TK. Deficient collagen formation by obese mice in a standard wound model. Am J Surg. 1979;138:692–4.
Nguyen NT, Goldman CD, Ho HS, et al. Systemic stress response after laparoscopic and open gastric bypass. J Am Coll Surg. 2002;194:557–66. discussion 66-7.
Nguyen NT, Wolfe BM. The physiologic effects of pneumoperitoneum in the morbidly obese. Ann Surg. 2005;241:219–26.
Artuso D, Wayne M, Cassaro S, et al. Hemodynamic changes during laparoscopic gastric bypass procedures. Arch Surg. 2005;140:289–92.
Jonsson K, Jensen JA, Goodson 3rd WH, et al. Assessment of perfusion in postoperative patients using tissue oxygen measurements. Br J Surg. 1987;74:263–7.
Miles AA, Miles EM, Burke JP. The value and duration of defense reactions of the skin to the primary lodgement of bacteria. Br J Exp Pathol. 1957;38:79.
Knighton DR, Halliday B, Hunt TK. Oxygen as an antibiotic. The effect of inspired oxygen on infection. Arch Surg. 1984;119:199–204.
Sido B, Teklote JR, Hartel M, et al. Inflammatory response after abdominal surgery. Best Pract Res Clin Anaesthesiol. 2004;18:439–54.
Daly WJ, Bondurant S. Effects of oxygen breathing on the heart rate, blood pressure, and cardiac index of normal men–resting, with reactive hyperemia, and after atropine. J Clin Invest. 1962;41:126–32.
Aubier M, Murciano D, Milic-Emili J, et al. Effects of the administration of O2 on ventilation and blood gases in patients with chronic obstructive pulmonary disease during acute respiratory failure. Am Rev Respir Dis. 1980;122:747–54.
Becker H, Polo O, McNamara SG, et al. Ventilatory response to isocapnic hyperoxia. J Appl Physiol. 1995;78:696–701.
Chang N, Goodson 3rd WH, Gottrup F, et al. Direct measurement of wound and tissue oxygen tension in postoperative patients. Ann Surg. 1983;197:470–8.
Akca O, Podolsky A, Eisenhuber E, et al. Comparable postoperative pulmonary atelectasis in patients given 30% or 80% oxygen during and 2 hours after colon resection. Anesthesiology. 1999;91:991–8.
Conflict of Interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Received from the Department of Anesthesiology and General Intensive Care, Medical University of Vienna, Austria, and the Outcomes Research Department, Anesthesiology Institute, Cleveland Clinic Lerner College of Medicine, Cleveland, OH, USA.
The study equipment was bought through an institutional research grant. None of the authors has any personal financial interest in this research.
Rights and permissions
About this article
Cite this article
Kabon, B., Rozum, R., Marschalek, C. et al. Supplemental Postoperative Oxygen and Tissue Oxygen Tension in Morbidly Obese Patients. OBES SURG 20, 885–894 (2010). https://doi.org/10.1007/s11695-010-0168-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-010-0168-1