Abstract
Purpose
The authors evaluated the role of magnetic resonance (MR) imaging of the chest in comparison with chest X-ray in the follow-up of pulmonary abnormalities detected by computed tomography (CT) in paediatric patients with middle lobe syndrome.
Materials and methods
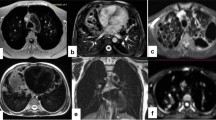
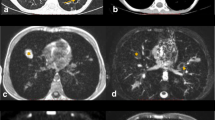
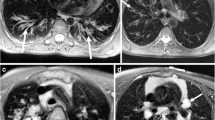
Seventeen patients with middle lobe syndrome (mean age 6.2 years) underwent chest CT at the time of diagnosis (100 kV, CARE dose with quality reference of 70 mAs; collimation 24×1.2 mm; rotation time 0.33 s; scan time 5 s); at follow-up after a mean of 15.3 months, all patients were evaluated with chest MR imaging with a respiratory-triggered T2-weighted BLADE sequence (TR 2,000; TE 27 ms; FOV 400 mm; flip angle 150°; slice thickness 5 mm) and chest X-ray. Images from each modality were assessed for the presence of pulmonary consolidations, bronchiectases, bronchial wall thickening and mucous plugging. Hilar and mediastinal lymphadenopathies were assessed on CT and MR images.
Results
Baseline CT detected consolidations in 100% of patients, bronchiectases in 35%, bronchial wall thickening in 53% and mucous plugging in 35%. MR imaging and chest X-ray identified consolidations in 65% and 35%, bronchiectases in 35% and 29%, bronchial wall thickening in 59% and 6% and mucous plugging in 25% and 0%, respectively. Lymphadenopathy was seen in 64% of patients at CT and in 47% at MR imaging.
Conclusions
Patients with middle lobe syndrome show a wide range of parenchymal and bronchial abnormalities at diagnosis. Compared with MR imaging, chest X-ray seems to underestimate these changes. Chest MR imaging might represent a feasible and radiation-free option for an overall assessment of the lung in the follow-up of patients with middle lobe syndrome.
Riassunto
Obiettivo
Scopo del presente lavoro è valutare il possibile ruolo della risonanza magnetica (RM) del torace, in confronto con l’Rx, nel follow-up delle alterazioni polmonari identificate con esame di tomografia computerizzata (TC) di diagnosi in un gruppo di pazienti pediatrici con sindrome del lobo medio (SLM).
Materiali e metodi
Diciassette pazienti (età media: 6,2 anni) hanno eseguito un esame TC del torace al momento della diagnosi (100 kV, CARE dose con riferimento di qualità: 70 mAs; collimation: 24×1,2 mm; rotation-time: 0,33 s; scan-time: 5 s); al follow-up (intervallo temporale medio: 15,3 mesi), tutti i pazienti hanno eseguito una RM polmonare [sequenza T2-pesata BLADE con triggeringrespiratorio: tempo di ripetizione (TR): 2000; tempo di eco (TE): 27 ms; campo di vista (FOV): 400 mm; flip-angle: 150°; spessore: 5 mm) ed un esame Rx del torace. La presenza di consolidazioni, bronchiectasie, ispessimento delle pareti bronchiali e mucous plugging (tappi di muco) è stato riportato per ogni modalità d’esame. La presenza di linfoadenopatie ilo-mediastiniche è stata riportata per TC ed RM.
Risultati
La TC di diagnosi ha riportato consolidazioni nel 100% dei pazienti; bronchiectasie: 35%; ispessimento delle pareti bronchiali: 53%; mucous plugging: 35%. RM/Rx hanno riportato, rispettivamente, consolidazioni: 65%/35%; bronchiectasie: 35%/29%; ispessimento delle pareti bronchiali: 59%/6%; mucous-plugging: 25%/0%. Linfoadenopatie sono state riportate nel 64% dei pazienti in TC e 47% in RM.
Conclusioni
I pazienti con SLM mostrano un ampio corteo di alterazioni polmonari sin dal momento della diagnosi. L’esame Rx sembra sottostimare, in confronto alla RM, la frequenza di tali alterazioni nel corso del follow-up; la RM polmonare può rappresentare una metodica promettente e priva di radiazioni ionizzanti nel follow-up di questi pazienti.
Similar content being viewed by others
References/Bibliografia
Boloorsaz MRI, Khalilzadeh S, Khodayari AA et al (2009) Middle lobe syndrome in children. Tanaffos 8:50–55
Livingston GL, Holinger LD, Luck SR (1987) Right middle lobe syndrome in children. Int J Pediatr Otorhinolaryngol 13:11–23
Gudmunddson G, Gross TJ (1996) Middle lobe syndrome. Am Fam Physician 53:2547–2550
Ring-Mrozik E, Hecker WC, Nerlich A et al (1991) Clinical findings in middle lobe syndrome and other processes of pulmonary shrinkage in children (atelectasis syndrome). Eur J Pediatr Surg 1:266–272
Heffelfinger JD, Davis TE, Gebrian B et al (2002) Evaluation of children with recurrent pneumonia diagnosed by WHO criteria. Pediatr Infect Dis J 21:108–112
Saha SP, Mayo P, Long GA et al (1982) Middle lobe syndrome. Diagnosis and management. Ann Thorac Surg 33:28–31
Inners CR, Terry PB, Traystman RJ (1978) Collateral ventilation in the middle lobe syndrome. Am Rev Resp Dis 118:305–310
Gupta PP, Gupta KB, Agarwal D (2006) Middle lobe syndrome due to tuberculous etiology: a series of 12 cases. Indian J Tuberc 53:104–108
Khun JP, Brody AS (2002) High resolution CT of pediatric lung disease. Radiol Clin North Am 40:89–110
Billig DM, Darling DB (1972) Middle lobe atelectasis in children. J Dis Child 123:96–98
Wong KS, Lin TY, Lan RS (1996) Evaluation of chronic atelectasis in children using chest computed tomography and bronchoscopy. Zhonghua Min Guo Xiao Er Ke Yi Xue Hui Za Zhi 37:193–196
Nadel TR, Stringer DA, Levison H et al (1985) The immotile cilia syndrome: radiological manifestations. Radiology 154:651–655
O’Connor OJ, Vandeleur M, McGarrigle AM et al (2010) Development of low-dose protocols for thin-section CT assessment of cystic fibrosis in pediatric patients. Radiology 257:820–829
Failo R, Wielopolski PA, Tiddens HA et al (2009) Lung morphology assessment using MRI: a robust ultra-short TR/ TE 2D steady state free precession sequence used in cystic fibrosis patients. Magn Reson Med 61:299–306
Puderbach M, Eichinger M, Gahr J et al (2007) Proton MRI appearance of cystic fibrosis: comparison to CT. Eur Radiol 17:716–724
Bayramoglu S, Kilickesmez O, Cimilli T et al (2010) T2-weighted MRI of the upper abdomen: comparison of four fat-suppressed T2-weighted sequences including PROPELLER (BLADE) technique. Acad Radiol 17:368–374
Fujimoto K, Koyama T, Tamai K et al (2010) BLADE acquisition method improves T2-weighted MRI images of the female pelvis compared with a standard fast spin-echo sequence. Eur J Radiol 80:796–801
Koh DM, Thoeny HC (2010) Diffusionweighted MRI imaging: applications in the body. Springer, Heidelberg Dordrecht London New York
European Commission (2001) Referral guidelines for imaging. Radiation Protection 118:115–116
De Jong PA, Tiddens HA (2007) Cystic fibrosis-specific computed tomography scoring. Proc Am Thorac Soc 4:338–342
Priftis KN, Mermiri D, Papadopoulou A et al (2005) The role of timely intervention in middle lobe syndrome in children. Chest 128:2504–2510
De Boeck K, Willems T, Van Gysel D et al (1995) Outcome after right middle lobe syndrome. Chest 108:150–152
Kwon KY, Myers JL, Swensen SJ et al (1995) Middle lobe syndrome: a clinicopathological study of 21 patients. Hum Pathol 26:302–307
De Jong PA, Mayo JR, Golmohammadi K et al (2006) Estimation of cancer mortality associated with repetitive computed tomography scanning. Am J Respir Crit Care Med 173:199–203
Hatabu H, Gaa J, Tadamura E et al (1999) MRI imaging of pulmonary parenchyma with a half-Fourier single-shot turbo spin echo (HASTE) sequence. Eur J Radiol 29:152–159
Fink C, Puderbach M, Biederer J et al (2007) Lung MRI at 1.5 and 3 Tesla: observer preference study and lesion contrast using five different pulse sequences. Invest Radiol 42:377–383
Hatabu H, Chen Q, Stock KW et al (1999) Fast magnetic resonance imaging of the lung. Eur J Radiol 29:114–132
Chen Q, Stock KW, Prasad PV et al (1999) Fast magnetic resonance imaging techniques. Eur J Radiol 29:90–100
Puderbach M, Hintze C, Ley S et al (2007) MRI imaging of the chest: a practical approach at 1.5 T. Eur J Radiol 64:345–355
Serra G, Milito C, Mitrevski M et al (2011) Lung magnetic resonance imaging as a possible alternative to computed tomography for patients with primary immune deficiencies and increased radio sensitivity. Chest 140:1581–1589
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fraioli, F., Serra, G., Ciarlo, G. et al. Chest MR imaging in the follow-up of pulmonary alterations in paediatric patients with middle lobe syndrome: comparison with chest X-ray. Radiol med 118, 444–455 (2013). https://doi.org/10.1007/s11547-012-0889-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-012-0889-3