Abstract
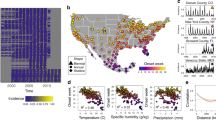
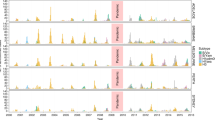
Characterizing how climate change will alter the burden of infectious diseases has clear public health implications. Despite our uniquely detailed understanding of the transmission process for directly transmitted immunizing infections, the impact of climate variables on these infections remains understudied. Here, we develop a novel approach that incorporates statistical analysis of climate effects with a mechanistic model of disease transmission, to investigate the dynamic response of directly transmitted, immunizing infections to climate change. We analyze the effect of climate on varicella, a common airborne childhood infection, by leveraging 30 years of reported cases across 32 states in Mexico. We use this to map the potential changes in the magnitude and variability of varicella incidence in Mexico as a result of predicted changes in future climate conditions. Our results indicate that the predicted decrease in relative humidity in Mexico towards the end of the century will increase incidence of varicella, all else equal. These changes in incidence will be non-uniform across the year such that cases will shift from winter to summer months. Climate-driven changes to the timing of future incidence, for these types of infections, may have substantial public health implications.





Similar content being viewed by others
References
Anderson R, May R (1991) Infectious diseases of humans: d and control. Oxford University Press
te Beest DE, van Boven M, Hooiveld M, van den Dool C, Wallinga J (2013) Driving factors of influenza transmission in the Netherlands. Am J Epidemiol 178:1469–1477
Bhadra A, Ionides EL, Laneri K, Pascual M, Bouma M, Dhiman RC (2011) Malaria in northwest india: data analysis via partially observed stochastic differential equation models driven by lévy noise. J Am Stat Assoc 106(494):440–451. https://doi.org/10.1198/jasa.2011.ap10323
Bjørnstad ON, Finkenstȧdt BF, Grenfell BT (2002) Dynamics of measles epidemics: estimating scaling of transmission rates using a time series SIR model. Ecol Monogr 72(2):169–184
Finkensädt BF, Grenfell BT (2000) Time series modelling of childhood diseases: a dynamical systems approach. J R Stat Soc Ser C Appl Stat 49(2):187–205. https://doi.org/10.1111/1467-9876.00187
Garnett GP, Grenfell BT (1992) The epidemiology of varicella-zoster virus infections: a mathematical model author. Epidemiol Infect 108(3):495–511
Garnett GP, Cox MJ, Bundy DA, Didier JM, St Catharine J (1993) The age of infection with varicella-zoster virus in St Lucia. West Indies., Epidemiology and infection 110(2):361–72. https://doi.org/10.1017/S0950268800068308
Knutti R, Furrer R, Tebaldi C, Cermak J, Meehl GA, Knutti R, Furrer R, Tebaldi C, Cermak J, Meehl GA (2010) Challenges in combining projections from multiple climate models. J Clim 23(10):2739–2758. https://doi.org/10.1175/2009JCLI3361.1
Koelle K, Rodȯ X, Pascual M, Yunus M, Mostafa G (2005) Refractory periods and climate forcing in cholera dynamics. Nature 436(7051):696–700. https://doi.org/10.1038/nature03820
Laneri K, Bhadra A, Ionides EL, Bouma M, Dhiman RC, Yadav RS, Pascual M (2010) Forcing versus feedback: epidemic malaria and monsoon rains in northwest india. PLoS Comput Biol 6(9):e1000,898. https://doi.org/10.1371/journal.pcbi.1000898
Laneri K, Paul RE, Tall A, Faye J, Diene-Sarr F, Sokhna C, Trape JF, Rodó X (2015) Dynamical malaria models reveal how immunity buffers effect of climate variability. Proc Natl Acad Sci U S A 112(28):8786–91. https://doi.org/10.1073/pnas.1419047112. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC4507245. http://www.ncbi.nlm.nih.gov/pubmed/26124134
Lolekha S, Tanthiphabha W, Sornchai P, Kosuwan P, Sutra S, Warachit B, Chup-Upprakarn S, Hutagalung Y, Weil J, Bock HL (2001) Effect of climatic factors and population density on varicella zoster virus epidemiology within a tropical country. Am J Trop Med Hyg 64(3):131–136
Lowen AC, Steel J (2014) Roles of humidity and temperature in shaping influenza seasonality. J Virol 88(14):7692–5. https://doi.org/10.1128/JVI.03544-13
Lowen AC, Mubareka S, Steel J, Palese P (2007) Influenza virus transmission is dependent on relative humidity and temperature. PLoS Pathog 3 (10):e151. https://doi.org/10.1371/journal.ppat.0030151
Mahmud AS, Metcalf CJE, Grenfell BT (2017) Comparative dynamics, seasonality in transmission, and predictability of childhood infections in Mexico. Epidemiol Infect 145(03):607–625. https://doi.org/10.1017/S0950268816002673
McCord G (2016) Malaria ecology and climate change. Eur Phys J Spec Top 225(3):459–470. https://doi.org/10.1140/epjst/e2015-50097-1
Metcalf CJE, Bjørnstad O.N., Grenfell BT, Andreasen V (2009) Seasonality and comparative dynamics of six childhood infections in pre-vaccination copenhagen. Proc Biol Sci / R Soc 276(1676):4111–8. https://doi.org/10.1098/rspb.2009.1058. http://rspb.royalsocietypublishing.org/content/276/1676/4111.short
Nardone A, de Ory F, Carton M, Cohen D, van Damme P, Davidkin I, Rota M, de Melker H, Mossong J, Slacikova M, Tischer A, Andrews N, Berbers G, Gabutti G, Gay N, Jones L, Jokinen S, Kafatos G, de Aragón MM, Schneider F, Smetana Z, Vargova B, Vranckx R, Miller E (2007) The comparative sero-epidemiology of varicella zoster virus in 11 countries in the european region. Vaccine 25(45):7866–7872. https://doi.org/10.1016/j.vaccine.2007.07.036. http://linkinghub.elsevier.com/retrieve/pii/S0264410X07008134
Pascual M, Cazelles B, Bouma M, Chaves L, Koelle K (2008) Shifting patterns: malaria dynamics and rainfall variability in an African highland. Proc R Soc B Biol Sci. 275(1631)
Pascual M, Chaves LF, Cash B, Rodȯ X, Yunus M (2008) Predicting endemic cholera: the role of climate variability and disease dynamics. Clim Res 36(2):131–140. https://doi.org/10.3354/cr00730
Pitzer VE, Viboud C, Alonso WJ, Wilcox T, Metcalf CJ, Steiner CA, Haynes AK, Grenfell BT (2015) Environmental drivers of the spatiotemporal dynamics of respiratory syncytial virus in the United States. PLoS Pathogens 11(1):e1004,591. https://doi.org/10.1371/journal.ppat.1004591. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC4287610. http://www.ncbi.nlm.nih.gov/pubmed/25569275
Plattner GK, Stocker T (2014) IPCC, 2014: Climate Change 2014: Synthesis report. Contribution of working groups I, II and III to the fifth assessment report of the intergovernmental panel on climate change., tech. rep., intergovernmental panel on climate change
Rinaldo A, Bertuzzo E, Mari L, Righetto L, Blokesch M, Gatto M, Casagrandi R, Murray M, Vesenbeckh SM, Rodriguez-Iturbe I (2012) Reassessment of the 2010-2011 Haiti cholera outbreak and rainfall-driven multiseason projections. Proc Natl Acad Sci U S A 109(17):6602–7. https://doi.org/10.1073/pnas.1203333109. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC3340092. http://www.ncbi.nlm.nih.gov/pubmed/22505737
Rodo X, Pascual M, Fuchs G, Faruque ASG (2002) ENSO And cholera: a nonstationary link related to climate change? Proc Natl Acad Sci U S A 99 (20):12,901–6. https://doi.org/10.1073/pnas.182203999. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC130557. http://www.ncbi.nlm.nih.gov/pubmed/12228724
Saddier P, Floret D, Guess HA, Du̇rr F, Peyrieux JC, Weber DJ, Plotkin SA (1998) Cost of Varicella in France: a study in day care centers. J Infect Dis 178(Suppl):58–63
Santermans E, Goeyvaerts N, Melegaro A, Edmunds WJ, Faes C, Aerts M, Beutels P, Hens N (2015) The social contact hypothesis under the assumption of endemic equilibrium: elucidating the transmission potential of VZV in Europe. Epidemics 11:14–23. https://doi.org/10.1016/j.epidem.2014.12.005
Shaman J, Kohn M (2009) Absolute humidity modulates influenza survival, transmission, and seasonality. Proc Natl Acad Sci U S A 106(9):3243–3248
Shaman J, Pitzer VE, Viboud C, Grenfell BT, Lipsitch M (2010) Absolute humidity and the seasonal onset of influenza in the continental United States. PLoS Biology 8:e1000316, 2
Tamerius J, Viboud C, Shaman J, Chowell G (2015) Impact of school cycles and environmental forcing on the timing of pandemic influenza activity in Mexican States, May–December 2009. PLoS Comput Biol 11(8)
Van Effelterre T, Shkedy Z, Aerts M, Molenberghs G, Van Damme P, Beutels P (2009) Contact patterns and their implied basic reproductive numbers: an illustration for Varicella-zoster virus. Epidemiology & Infection 137(1):48–57
Vergara-Castaṅeda A, Escobar-Gutiėrrez A, Ruiz-Tovar K, Sotelo J, Ordoṅez G, Cruz-Rivera MY, Fonseca-Coronado S, Martinez-Guarneros A, Carpio-Pedroza JC, Vaughan G (2012) Epidemiology of varicella in Mexico. J Clin Virol 55(1):51–57. https://doi.org/10.1016/j.jcv.2012.06.004
Yang HM, Macoris MLG, Galvani KC, Andrighetti MTM, Wanderley DMV (2009) Assessing the effects of temperature on dengue transmission. Epidemiol Infect 137(08):1179. https://doi.org/10.1017/S0950268809002052
Funding
This work was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (A.S.M., grant number 5R24HD047879); the National Institutes of Health training grant (A.S.M., grant number 5T32HD007163); the Rockefeller Foundation Planetary Health Fellowship (A.S.M.); the Walbridge Fund in the Princeton Environmental Institute at Princeton University (R.E.B); the Bill and Melinda Gates Foundation; and a Wellcome Trust Sustaining Health grant (C.J.E.M., grant number 106866/Z/15/Z).
Author information
Authors and Affiliations
Corresponding author
Additional information
Rachel E. Baker and Ayesha S. Mahmud contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Baker, R.E., Mahmud, A.S. & Metcalf, C.J.E. Dynamic response of airborne infections to climate change: predictions for varicella. Climatic Change 148, 547–560 (2018). https://doi.org/10.1007/s10584-018-2204-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10584-018-2204-4