Abstract
Background
Due to their relative scarcity and to limit single-center bias, multi-center data are needed to study femoral hernias. The aim of this study was to evaluate outcomes and quality of life (QOL) following laparoscopic vs. open repair of femoral hernias.
Methods
The International Hernia Mesh Registry was queried for femoral hernia repairs. Laparoscopic vs. open techniques were assessed for outcomes and QOL, as quantified by the Carolinas Comfort Scale (CCS), preoperatively and at 1, 6, 12, and 24 months postoperatively. Outcomes were evaluated using the standard statistical analysis.
Results
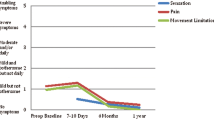
A total of 80 femoral hernia repairs were performed in 73 patients: 37 laparoscopic and 43 open. There was no difference in mean age (54.7 ± 14.6 years), body mass index (24.2 ± 3.8 kg/m2), gender (60.3 % female), or comorbidities (p > 0.05). The hernias were recurrent in 21 % of the cases with an average of 1.23 ± 0.6 prior repairs (p > 0.1). Preoperative CCS scores were similar for both groups and indicated that 59.7 % of patients reported pain and 46.4 % had movement limitations (p > 0.05). Operative time was equivalent (47.2 ± 21.2 vs. 45.9 ± 14.8 min, p = 0.82). There was no difference in postoperative complications, with an overall 8.2 % abdominal wall complications rate (p > 0.05). The length of stay was shorter in the laparoscopic group (0.5 ± 0.6 vs. 1.3 ± 1.6 days, p = 0.02). Follow-up was somewhat longer in the open group (23.8 ± 10.2 vs. 17.3 ± 10.9 months, p = 0.02). There was one recurrence, which was in the laparoscopic group (3.1 vs. 0 %, p = 0.4). QOL outcomes at all time points demonstrated no difference for pain, movement limitation, or mesh sensation. Postoperative QOL scores improved for both groups when compared to preoperative scores.
Conclusion
In this prospective international multi-institution study of 80 femoral hernia repairs, no difference was found for operative times, long-term outcomes, or QOL in the treatment of femoral hernias when comparing laparoscopic vs. open techniques. After repair, QOL at all time-points postoperatively improved compared to QOL scores preoperatively for laparoscopic and open femoral hernia repair. While international data supports improved outcomes with laparoscopic approach for femoral hernia repair, no data had existed prior to this study on the difference of approach impacting QOL. In the setting where recurrence and complication rates are equal after femoral hernia repair for either approach, surgeons should perform the technique with which they are most confident, as the operative approach does not appear to change QOL outcomes after femoral hernia repair.





Similar content being viewed by others
References
Rutkow IM (2003) Demographic and socioeconomic aspects of hernia repair in the United States in 2003. Surg Clin N Am 83(5):1045–1051. doi:10.1016/s0039-6109(03)00132-4 (v–vi)
Primatesta P, Goldacre MJ (1996) Inguinal hernia repair: incidence of elective and emergency surgery, readmission and mortality. Int J Epidemiol 25(4):835–839
Dahlstrand U, Wollert S, Nordin P, Sandblom G, Gunnarsson U (2009) Emergency femoral hernia repair: a study based on a national register. Ann Surg 249(4):672–676. doi:10.1097/SLA.0b013e31819ed943
Nilsson H, Stylianidis G, Haapamaki M, Nilsson E, Nordin P (2007) Mortality after groin hernia surgery. Ann Surg 245(4):656–660. doi:10.1097/01.sla.0000251364.32698.4b
Murray RW (1910) VIII. Is the sac of a femoral hernia of congenital origin, or acquired? Ann Surg 52(5):668–677
McVay CB, Savage LE (1961) Etiology of femoral hernia. Ann Surg 154(Suppl 6):25–32
Glassow F (1971) Femoral hernia in men. Am J Surg 121(6):637–640
Sandblom G, Haapaniemi S, Nilsson E (1999) Femoral hernias: a register analysis of 588 repairs. Hernia 3:131–134
Mikkelsen T, Bay-Nielsen M, Kehlet H (2002) Risk of femoral hernia after inguinal herniorrhaphy. Br J Surg 89(4):486–488. doi:10.1046/j.0007-1323.2002.02058.x
Burcharth J (2014) The epidemiology and risk factors for recurrence after inguinal hernia surgery. Dan Med J 61(5):B4846
Rosenberg J, Bisgaard T, Kehlet H, Wara P, Asmussen T, Juul P, Strand L, Andersen FH, Bay-Nielsen M, Danish Hernia D (2011) Danish hernia database recommendations for the management of inguinal and femoral hernia in adults. Dan Med Bull 58(2):C4243
Heniford BT, Walters AL, Lincourt AE, Novitsky YW, Hope WW, Kercher KW (2008) Comparison of generic versus specific quality-of-life scales for mesh hernia repairs. J Am Coll Surg 206(4):638–644. doi:10.1016/j.jamcollsurg.2007.11.025
Whalen HR, Kidd GA, O’Dwyer PJ (2011) Femoral hernias. BMJ (Clin Res Ed) 343:d7668. doi:10.1136/bmj.d7668
Gallegos NC, Dawson J, Jarvis M, Hobsley M (1991) Risk of strangulation in groin hernias. Br J Surg 78(10):1171–1173
Bay-Nielsen M, Kehlet H, Strand L, Malmstrom J, Andersen FH, Wara P, Juul P, Callesen T, Danish Hernia Database C (2001) Quality assessment of 26,304 herniorrhaphies in Denmark: a prospective nationwide study. Lancet 358(9288):1124–1128. doi:10.1016/s0140-6736(01)06251-1
Andresen K, Bisgaard T, Kehlet H, Wara P, Rosenberg J (2014) Reoperation rates for laparoscopic vs open repair of femoral hernias in Denmark: a nationwide analysis. JAMA Surg 149(8):853–857. doi:10.1001/jamasurg.2014.177
Crawford DL, Hiatt JR, Phillips EH (1998) Laparoscopy identifies unexpected groin hernias. Am Surg 64(10):976–978
Hair A, Paterson C, O’Dwyer PJ (2001) Diagnosis of a femoral hernia in the elective setting. J R Coll Surg Edinb 46(2):117–118
Naude GP, Ocon S, Bongard F (1997) Femoral hernia: the dire consequences of a missed diagnosis. Am J Emerg Med 15(7):680–682
Hernandez-Richter T, Schardey HM, Rau HG, Schildberg FW, Meyer G (2000) The femoral hernia: an ideal approach for the transabdominal preperitoneal technique (TAPP). Surg Endosc 14(8):736–740
Henriksen NA, Thorup J, Jorgensen LN (2012) Unsuspected femoral hernia in patients with a preoperative diagnosis of recurrent inguinal hernia. Hernia 16(4):381–385. doi:10.1007/s10029-012-0924-3
Glassow F (1985) Femoral hernia. Review of 2,105 repairs in a 17 year period. Am J Surg 150(3):353–356
McCormack K, Scott NW, Go PM, Ross S, Grant AM, Collaboration EUHT (2003) Laparoscopic techniques versus open techniques for inguinal hernia repair. Cochrane Database Syst Rev (1):CD001785. doi:10.1002/14651858.cd001785
Guarracino F, Baldassarri R, Priebe HJ (2015) Revised ESC/ESA guidelines on non-cardiac surgery: cardiovascular assessment and management. Implications for preoperative clinical evaluation. Minerva Anestesiol 81(2):226–233
Torres-Ruiz MF, Cardenas-Lailson LE, Quiroz-Villegas ME, Bravo-Leon J (2014) A standard questionnaire to reduce the routine battery of preoperative tests for elective surgery. Cir Cir 82(5):517–527
Onuoha OC, Arkoosh VA, Fleisher LA (2014) Choosing wisely in anesthesiology: the gap between evidence and practice. JAMA Intern Med 174(8):1391–1395. doi:10.1001/jamainternmed.2014.2309
Ali SM, Zendejas B, Yadav S, Hernandez-Irizarry RC, Lohse CM, Farley DR (2013) Predictors of chronic groin discomfort after laparoscopic totally extraperitoneal inguinal hernia repair. J Am Coll Surg 217(1):72–78. doi:10.1016/j.jamcollsurg.2013.03.005 (discussion 78–80)
Poobalan AS, Bruce J, King PM, Chambers WA, Krukowski ZH, Smith WC (2001) Chronic pain and quality of life following open inguinal hernia repair. Br J Surg 88(8):1122–1126. doi:10.1046/j.0007-1323.2001.01828.x
Franneby U, Sandblom G, Nordin P, Nyren O, Gunnarsson U (2006) Risk factors for long-term pain after hernia surgery. Ann Surg 244(2):212–219. doi:10.1097/01.sla.0000218081.53940.01
Dahlstrand U, Sandblom G, Nordin P, Wollert S, Gunnarsson U (2011) Chronic pain after femoral hernia repair: a cross-sectional study. Ann Surg 254(6):1017–1021. doi:10.1097/SLA.0b013e31822ba9b6
Awad SS, Fagan SP (2004) Current approaches to inguinal hernia repair. Am J Surg 188(6A Suppl):9S–16S. doi:10.1016/j.amjsurg.2004.09.007
Colavita PD, Tsirline VB, Belyansky I, Walters AL, Lincourt AE, Sing RF, Heniford BT (2012) Prospective, long-term comparison of quality of life in laparoscopic versus open ventral hernia repair. Ann Surg 256(5):714–722. doi:10.1097/SLA.0b013e3182734130 (discussion 722–713)
Belyansky I, Tsirline VB, Klima DA, Walters AL, Lincourt AE, Heniford TB (2011) Prospective, comparative study of postoperative quality of life in TEP, TAPP, and modified Lichtenstein repairs. Ann Surg 254(5):709–714. doi:10.1097/SLA.0b013e3182359d07 (discussion 714–705)
Lundstrom KJ, Sandblom G, Smedberg S, Nordin P (2012) Risk factors for complications in groin hernia surgery: a national register study. Ann Surg 255(4):784–788. doi:10.1097/SLA.0b013e31824b7cb3
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest for any authors related to this work. BTH has W.L. Gore and Associates, Ethicon, Novadaq, Bard/Davol, and LifeCell Inc not related to this work. VAA has W.L. Gore and Associates, Ethicon, Novadaq, Bard/Davol, and LifeCell Inc not related to this work. TCC has no conflicts of interest related or unrelated to this work. CRH has no conflicts of interest related or unrelated to this work. LJB has no conflicts of interest related or unrelated to this work. TP has no conflicts of interest related or unrelated to this work.
Ethical approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Accepted for podium presentation at the 1st World Conference on Abdominal Wall Surgery, Milan, Italy, April 2015.
Rights and permissions
About this article
Cite this article
Cox, T.C., Huntington, C.R., Blair, L.J. et al. Quality of life and outcomes for femoral hernia repair: does laparoscopy have an advantage?. Hernia 21, 79–88 (2017). https://doi.org/10.1007/s10029-016-1502-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-016-1502-x