Abstract
Background
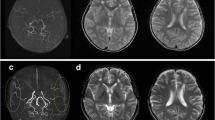
Moyamoya disease (MMD) concurrent with Graves’ disease (GD) is rare. There is no guideline about optimizing thyroid hormones and the appropriate timing of surgical treatment for MMD with GD.
Methods
We encountered eight patients with MMD and GD presenting with cerebral ischemia who were treated by direct bypass. Thyroid hormones [free thyroxin (fT4) and free triiodothyronine (fT3)], thyroid-stimulating hormone (TSH), and TSH receptor antibody (TRAb) were measured sequentially. After thyrotoxic conditions were medically optimized, revascularization surgery was performed by superficial temporal artery-middle cerebral artery (STA-MCA) double bypass in all cases. Clinical outcomes were estimated by modified Rankin scale (mRS) at discharge and 3 months after surgery.
Results
In six patients with thyrotoxicosis, the fT4, fT3, and TRAb (range) at the onset of cerebral ischemia were 4.81–10.30 pg/ml, 13.08–31.90 pg/ml, and 3.5–83.8 IU/l, respectively. At surgery, mean (range) fT3 and fT4 were optimized to 3.02 (1.01–4.87) pg/ml and 1.09 (0.41–1.68) ng/dl, respectively. In the thyrotoxic cases, it took 70–310 days (mean, 142 days) to optimize thyroid hormones before surgery. There was no neurological aggravation after surgery, and outcome was excellent at 3 months with mRS scores ≤2 in all cases.
Conclusions
For MMD concurrent with GD, optimizing thyroid hormones followed by STA-MCA double bypass was successful to prevent cerebral ischemic events.




Similar content being viewed by others
References
Akamizu T, Satoh T, Isozaki O, Suzuki A, Wakino S, Iburi T, Tsuboi K, Monden T, Kouki T, Otani H, Teramukai S, Uehara R, Nakamura Y, Nagai M, Mori M, Japan Thyroid Association (2012) Diagnostic criteria, clinical features, and incidence of thyroid storm based on nationwide surveys. Thyroid 22:661–679
Colleran KM, Ratliff DM, Burge MR (2003) Potential association of thyrotoxicosis with vitamin B and folate deficiencies, resulting in risk for hyperhomocysteinemia and subsequent thromboembolic events. Endocr Pract 9:290–295
Hintze G, Blombach O, Fink H, Burkhardt U, Köbberling J (1999) Risk of iodine-induced thyrotoxicosis after coronary angiography: an investigation in 788 unselected subjects. Eur J Endocrinol 140:264–267
Im SH, Oh CW, Kwon OK, Kim JE, Han DH (2005) Moyamoya disease associated with Graves’ disease, special considerations regarding clinical significance and management. J Neurosurg 102:1013–1017
Ishigami A, Toyoda K, Suzuki R, Miyashita F, Iihara K, Minematsu K (2014) Neurologic improvement without angiographic improvement after antithyroid therapy in a patient with moyamoya syndrome. J Stroke Cerebrovasc Dis 23:1256–1258
Iso H, Moriyama Y, Sato S, Kitamura A, Tanigawa T, Yamagishi K, Imano H, Ohira T, Okamura T, Naito Y, Shimamoto T (2004) Serum total homocysteine concentrations and risk of stroke and its subtypes in Japanese. Circulation 109:2766–2772
Japan Thyroid Association. Guideline for the diagnosis of Graves’ disease 2010. http://www.japanthyroid.jp/doctor/guideline/english.html#basedou. Accessed 24 Jun 2013
Kawamata T, Okada Y, Kawashima A, Yoneyama T, Yamaguchi K, Ono Y, Hori T (2009) Post-carotid endarterectomy cerebral hyperperfusion can be prevented by minimizing intraoperative cerebral ischemia and strict postoperative blood pressure control under continuous sedation. Neurosurgery 64:447–454
Kim SJ, Heo KG, Shin HY, Bang OY, Kim GM, Chung CS, Kim KH, Jeon P, Kim JS, Hong SC, Lee KH (2010) Association of thyroid autoantibodies with moyamoya-type cerebrovascular disease: a prospective study. Stroke 41:173–176
Kushima K, Satoh Y, Ban Y, Taniyama M, Ito K, Sugita K (1991) Graves’ thyrotoxicosis and moyamoya disease. Can J Neurol Sci 18:140–142
Lee R, Sung K, Park YM, Yu JJ, Koh YC, Chung S (2009) A case of moyamoya disease in a girl with thyrotoxicosis. Yonsei Med J 50:594–598
Li D, Yang W, Xian P, Liu P, Bao X, Zong R, Duan L (2013) Coexistence of moyamoya and Graves’ diseases: the clinical characteristics and treatment effects of 21 Chinese patients. Clin Neurol Neurosurg 115:1647–1652
Liu JS, Juo SH, Chen WH, Chang YY, Chen SS (1994) A case of Graves’ diseases associated with intracranial moyamoya vessels and tubular stenosis of extracranial internal carotid arteries. J Formos Med Assoc 93:806–809
Malik S, Russman AN, Katramados AM, Silver B, Mitsias PD (2011) Moyamoya syndrome associated with Graves’ disease: a case report and review of the literature. J Stroke Cerebrovasc Dis 20:528–536
McDermott MT (2012) Hyperthyroidism. Ann Intern Med 157:TIC1 1–16
Mikami T, Sugino T, Kanno A, Houkin K, Mikuni N (2012) Moyamoya syndrome associated with Graves’ disease [in Japanese]. Jpn J Stroke 34:82–88
Morisawa H, Kawamata T, Kawashima A, Hayashi M, Yamaguchi K, Yoneyama T, Okada Y (2013) Hemodynamics and changes after STA-MCA anastomosis in moyamoya disease and atherosclerotic cerebrovascular disease measured by micro-Doppler ultrasonography. Neurosurg Rev 36:411–419
Ohba S, Nakagawa T, Murakami H (2011) Concurrent Graves’ disease and intracranial arterial stenosis/occlusion. Special considerations regarding the state of thyroid function, etiology, and treatment. Neurosurg Rev 34:297–304
Okada Y, Shima T, Nishida M, Yamane K, Yamada T, Yamanaka C (1998) Effectiveness of superficial temporal artery–middle cerebral artery anastomosis in adult moyamoya disease: cerebral hemodynamics and clinical course in ischemic and hemorrhagic varieties. Stroke 29:625–630
Okada Y, Shima T, Yamane K, Yamanaka C, Kagawa R (1999) Cylindrical or T-shaped silicone rubber stents for microanastomosis. Technical note. Neurol Med Chir (Tokyo) 39:55–58
Panegyres PK, Morris JG, O’Neill PJ, Balleine R (1993) Moyamoya-like disease with inflammation. Eur Neurol 33:260–263
Recommendations for the management of moyamoya disease (2009) A statement from research committee on spontaneous occlusion of the circle of Willis (moyamoya disease) [in Japanese] Surgery for cerebral stroke 37:321–337
Siegert CE, Smelt AH, de Bruin TW (1995) Superior sagittal sinus thrombosis and thyrotoxicosis. Possible association in two cases. Stroke 26:496–497
Soliman M, Kaplan E, Yanagawa T, Hidaka Y, Fisfalen ME, DeGroot LJ (1995) T-cells recognize multiple epitopes in the human thyrotropin receptor extracellular domain. J Clin Endocrinol Metabol 80:905–914
Suzuki J, Kodama N (1983) Moyamoya disease: a review. Stroke 14:104–109
Suzuki J, Takaku A (1969) Cerebrovascular moyamoya disease. Disease showing abnormal net-like vessels in base of brain. Arch Neurol 20:288–299
Suzuki S, Mitsuyama T, Horiba A, Fukushima S, Hashimoto N, Kawamata T (2011) Moyamoya disease complicated by Graves’ disease and type 2 diabetes mellitus: report of two cases. Clin Neurol Neurosurg 113:325–329
Tendler BE, Shoukri K, Malchoff C, MacGillivray D, Duckrow R, Talmadge T, Ramsby GR (1997) Concurrence of Graves’ disease and dysplastic cerebral blood vessels of the moyamoya variety. Thyroid 7:625–629
Utku U, Asil T, Celik Y, Tucer D (2004) Reversible MR angiographic findings in a patient with autoimmune Graves’ disease. AJNR Am J Neuroradiol 25:1541–1543
Yamaguchi K, Kawamata T, Kawashima A, Hori T, Okada Y (2010) Incidence and predictive factors of cerebral hyperperfusion after extracranial-intracranial bypass for occlusive cerebrovascular diseases. Neurosurgery 67:1548–1554
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comment
Ryu and colleagues report about eight patients with moyamoya disease concurrent with Graves’ disease, and treated by superficial temporal artery-middle cerebral artery bypass. Even though the combination of moyamoya disease and Graves’ disease is rare, it is worth keeping it in mind, since both have similar pathogeneses and there are important risks to be considered in the perioperative period. The present paper provides important and interesting information about clinical features and treatment strategies of this exceptional group of patients.
Marcus Reinges
Giessen, Germany
Rights and permissions
About this article
Cite this article
Ryu, B., Kawamata, T., Yamaguchi, K. et al. Moyamoya disease concurrent with Graves’ disease treated by direct bypass: clinical features and treatment strategies. Acta Neurochir 157, 1095–1102 (2015). https://doi.org/10.1007/s00701-015-2422-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-015-2422-8