Abstract
Purpose
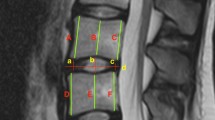
Even though phenotypes of disc degeneration vary on different sagittal magnetic resonance images (MRI), measurements typically are acquired on the mid-sagittal MRI. This study investigated the appropriateness of using the mid-sagittal MRI to measure various phenotypes of age-related disc degeneration.
Methods
Lumbar spine MRIs of 66 subjects (mean age 50.3 years, standard deviation 16.5 years, range 22–84 years) were studied. An image analysis program Spine Explorer was used to obtain quantitative measurements for disc height, bulging, and signal on para- and mid-sagittal T2-weighted MRIs. Measurements on para- and mid-sagittal MRIs and their associations with age were compared.
Results
Measurements of disc height, signal, and posterior disc bulging acquired on the mid-sagittal MRI were greater than those on the para-sagittal MRIs. Disc height measurements were not linearly associated with age. Greater age was correlated with greater anterior (r = 0.45, P < 0.001) and posterior (r = 0.33, P < 0.01) bulging on para-sagittal MRIs, but not posterior disc bulging on the mid-sagittal MRI (r = − 0.10, P > 0.05). Disc signal intensity measurements on the mid-sagittal MRI had stronger correlations with age than those on para-sagittal MRIs. Mean and standard deviation of disc signal intensity acquired on the mid-sagittal MRI had the strongest correlations with age among all measures of disc degeneration studied (r = − 0.50, − 0.67, respectively, P < 0.001 for both).
Conclusions
Disc signal measurements acquired on the mid-sagittal MRI were reliable and had strong correlations with age and thus can be used as an appropriate measure of disc degeneration. Disc bulging had better be measured on para-sagittal MRIs. Although severe disc narrowing clearly is a sign of severe disc degeneration, disc height was not linearly associated with age.




Similar content being viewed by others
References
Deyo RA, Weinstein JN (2001) Low back pain. N Engl J Med 344:363–370. https://doi.org/10.1056/NEJM200102013440508
Luoma K, Riihimaki H, Luukkonen R, Raininko R, Viikari-Juntura E, Lamminen A (2000) Low back pain in relation to lumbar disc degeneration. Spine 25:487–492
Battie MC, Videman T (2006) Lumbar disc degeneration: epidemiology and genetics. J Bone Joint Surg Am 88(Suppl 2):3–9. https://doi.org/10.2106/JBJS.E.01313
Cheung KM, Karppinen J, Chan D, Ho DW, Song YQ, Sham P, Cheah KS, Leong JC, Luk KD (2009) Prevalence and pattern of lumbar magnetic resonance imaging changes in a population study of one thousand forty-three individuals. Spine 34:934–940. https://doi.org/10.1097/BRS.0b013e3181a01b3f
Adams MA, Roughley PJ (2006) What is intervertebral disc degeneration, and what causes it? Spine 31:2151–2161. https://doi.org/10.1097/01.brs.0000231761.73859.2c
Kettler A, Wilke HJ (2006) Review of existing grading systems for cervical or lumbar disc and facet joint degeneration. Eur Spine J 15:705–718. https://doi.org/10.1007/s00586-005-0954-y
Videman T, Gibbons LE, Battie MC (2008) Age- and pathology-specific measures of disc degeneration. Spine 33:2781–2788. https://doi.org/10.1097/BRS.0b013e31817e1d11
Sambrook PN, MacGregor AJ, Spector TD (1999) Genetic influences on cervical and lumbar disc degeneration: a magnetic resonance imaging study in twins. Arthritis Rheum 42:366–372. https://doi.org/10.1002/1529-0131(199902)42:2<366:AID-ANR20>3.0.CO;2-6
Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N (2001) Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine 26:1873–1878
Haughton VM (2006) Dynamic MR and quantitative MR applied to the study of intervertebral disk degeneration. Neuroradiol J 19:496–503
Griffith JF, Wang YX, Antonio GE, Choi KC, Yu A, Ahuja AT, Leung PC (2007) Modified Pfirrmann grading system for lumbar intervertebral disc degeneration. Spine 32:E708–E712. https://doi.org/10.1097/BRS.0b013e31815a59a0
Videman T, Nummi P, Battie MC, Gill K (1994) Digital assessment of MRI for lumbar disc desiccation. A comparison of digital versus subjective assessments and digital intensity profiles versus discogram and macroanatomic findings. Spine 19:192–198
Videman T, Battie MC, Parent E, Gibbons LE, Vainio P, Kaprio J (2008) Progression and determinants of quantitative magnetic resonance imaging measures of lumbar disc degeneration: a five-year follow-up of adult male monozygotic twins. Spine 33:1484–1490. https://doi.org/10.1097/BRS.0b013e3181753bb1
Jarman JP, Arpinar VE, Baruah D, Klein AP, Maiman DJ, Muftuler LT (2015) Intervertebral disc height loss demonstrates the threshold of major pathological changes during degeneration. Eur Spine J 24:1944–1950. https://doi.org/10.1007/s00586-014-3564-8
Harry NH, Steven RG, Frank JE, Dordon RB, Richard AB (2011) Lumbar Disc Herniations. In: Rothman-Simeone The Spine, 6th edn. Saunders, Philadelphia, pp 762–790. https://doi.org/10.1016/b978-1-4160-6726-9.00046-8
Hu X, Chen L, Battié MC, Wang Y (2017) Methodology and cohort profile for The Hangzhou Lumbar Spine Study: a population-based study focusing on back health in a Chinese population. J Zhejiang Univ Sci B. https://doi.org/10.1631/jzus.B1700484
Battie MC, Videman T, Gibbons LE, Fisher LD, Manninen H, Gill K (1995) 1995 Volvo Award in clinical sciences. Determinants of lumbar disc degeneration. A study relating lifetime exposures and magnetic resonance imaging findings in identical twins. Spine 20:2601–2612
Masuda K, Aota Y, Muehleman C, Imai Y, Okuma M, Thonar EJ, Andersson GB, An HS (2005) A novel rabbit model of mild, reproducible disc degeneration by an anulus needle puncture: correlation between the degree of disc injury and radiological and histological appearances of disc degeneration. Spine 30:5–14
Feng Z, Liu Y, Wei W, Hu S, Wang Y (2016) Type II modic changes may not always represent fat degeneration: a study using MR fat suppression sequence. Spine 41:E987–E994. https://doi.org/10.1097/BRS.0000000000001526
Landis JRKG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Boos N, Weissbach S, Rohrbach H, Weiler C, Spratt KF, Nerlich AG (2002) Classification of age-related changes in lumbar intervertebral discs: 2002 Volvo Award in basic science. Spine 27:2631–2644. https://doi.org/10.1097/01.BRS.0000035304.27153.5B
Heine J (1926) Ûber die Arthritis deformans. Virch Arch Pathol Anat 260:521–663
Coventry MBGR, Kernohan JW (1945) The intervertebral disc: its microscopic anatomy and pathology: II. Changes in the intervertebral disc concomitant with age. J Bone Joint Surg Am 27:233–247
Schmorl GJH (1971) The human spine in health and disease. Grune and Stratton, New York
Dolan P, Luo J, Pollintine P, Landham PR, Stefanakis M, Adams MA (2013) Intervertebral disc decompression following endplate damage: implications for disc degeneration depend on spinal level and age. Spine 38:1473–1481. https://doi.org/10.1097/BRS.0b013e318290f3cc
Schmorl CG (1926) Die pathologische Anatomie der Wirbelsäule. Verhandlungen der Deutschen Orthopädischen Gesellschaft 21:3–41
Kellgren jh lj (1952) Rheumatism in miners. II. X-raystudy. Br J Ind Med 9:197–207
Frobin W, Brinckmann P, Kramer M, Hartwig E (2001) Height of lumbar discs measured from radiographs compared with degeneration and height classified from MR images. Eur Radiol 11:263–269. https://doi.org/10.1007/s003300000556
Luoma K, Vehmas T, Riihimaki H, Raininko R (2001) Disc height and signal intensity of the nucleus pulposus on magnetic resonance imaging as indicators of lumbar disc degeneration. Spine 26:680–686. https://doi.org/10.1097/00007632-200103150-00026
Twomey L, Taylor J (1985) Age changes in lumbar intervertebral discs. Acta Orthop Scand 56:496–499. https://doi.org/10.3109/17453678508993043
Zou J, Yang H, Miyazaki M, Morishita Y, Wei F, McGovern S, Wang JC (2009) Dynamic bulging of intervertebral discs in the degenerative lumbar spine. Spine 34:2545–2550. https://doi.org/10.1097/BRS.0b013e3181b32998
Farshad-Amacker NA, Farshad M, Winklehner A, Andreisek G (2015) MR imaging of degenerative disc disease. Eur J Radiol 84:1768–1776. https://doi.org/10.1016/j.ejrad.2015.04.002
Vergroesen PP, Kingma I, Emanuel KS, Hoogendoorn RJ, Welting TJ, van Royen BJ, van Dieen JH, Smit TH (2015) Mechanics and biology in intervertebral disc degeneration: a vicious circle. Osteoarthritis Cartilage 23:1057–1070. https://doi.org/10.1016/j.joca.2015.03.028
Modic MT, Pavlicek W, Weinstein MA, Boumphrey F, Ngo F, Hardy R, Duchesneau PM (1984) Magnetic resonance imaging of intervertebral disk disease. Clinical and pulse sequence considerations. Radiology 152:103–111. https://doi.org/10.1148/radiology.152.1.6729099
Wang Y, Videman T, Battie MC (2013) Morphometrics and lesions of vertebral end plates are associated with lumbar disc degeneration: evidence from cadaveric spines. J Bone Joint Surg Am 95:e26. https://doi.org/10.2106/JBJS.L.00124
Duran S, Cavusoglu M, Hatipoglu HG, Sozmen Ciliz D, Sakman B (2017) Association between measures of vertebral endplate morphology and lumbar intervertebral disc degeneration. Can Assoc Radiol J 68:210–216. https://doi.org/10.1016/j.carj.2016.11.002
Wang Y, Videman T, Niemelainen R, Battie MC (2011) Quantitative measures of modic changes in lumbar spine magnetic resonance imaging: intra- and inter-rater reliability. Spine 36:1236–1243. https://doi.org/10.1097/BRS.0b013e3181ecf283
Kanna RM, Shanmuganathan R, Rajagopalan VR, Natesan S, Muthuraja R, Cheung KMC, Chan D, Kao PYP, Yee A, Shetty AP (2017) Prevalence, patterns, and genetic association analysis of modic vertebral endplate changes. Asian Spine J 11:594–600. https://doi.org/10.4184/asj.2017.11.4.594
Wang Y, Videman T, Battie MC (2012) Lumbar vertebral endplate lesions: prevalence, classification, and association with age. Spine 37:1432–1439. https://doi.org/10.1097/BRS.0b013e31824dd20a
Wang Y, Videman T, Battie MC (2012) ISSLS prize winner: lumbar vertebral endplate lesions: associations with disc degeneration and back pain history. Spine 37:1490–1496. https://doi.org/10.1097/BRS.0b013e3182608ac4
Mok FP, Samartzis D, Karppinen J, Luk KD, Fong DY, Cheung KM (2010) ISSLS prize winner: prevalence, determinants, and association of Schmorl nodes of the lumbar spine with disc degeneration: a population-based study of 2449 individuals. Spine 35:1944–1952. https://doi.org/10.1097/BRS.0b013e3181d534f3
Feng Z, Liu Y, Yang G, Battie MC, Wang Y (2017) Lumbar vertebral endplate defects on magnetic resonance images: classification, distribution patterns, and associations with modic changes and disc degeneration. Spine. https://doi.org/10.1097/BRS.0000000000002450
Zehra U, Bow C, Lotz JC, Williams FMK, Rajasekaran S, Karppinen J, Luk KDK, C Battie M, Samartzis D (2017) Structural vertebral endplate nomenclature and etiology: a study by the ISSLS Spinal Phenotype Focus Group. Eur Spine J. https://doi.org/10.1007/s00586-017-5292-3
Acknowledgements
We are indebted to Ms. Ying Yuan for her tremendous work in subject recruitment and data collection. We also thank the clinic staffs at the Department of Orthopedic Surgery and Radiology at the first affiliated hospital of Zhejiang University for their assistance in conducting the Hangzhou Lumbar Spine Study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was supported by the National Natural Science Foundation of China (81371995), Key Platform Project of the Health Department of Zhejiang Province (2015ZDA014) and 2015 Qianjiang Talent Plan of Zhejiang Province.
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Hu, X., Chen, M., Pan, J. et al. Is it appropriate to measure age-related lumbar disc degeneration on the mid-sagittal MR image? A quantitative image study. Eur Spine J 27, 1073–1081 (2018). https://doi.org/10.1007/s00586-017-5357-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-5357-3