Abstract
Purpose
We investigated whether ventilation volumes affected arterial blood sevoflurane concentration (A sev) and its uptake into the body during general anesthesia.
Methods
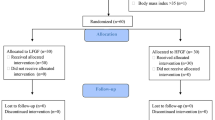
Thirty female patients undergoing elective gynecologic surgery were randomly allocated into three groups: hyperventilation, normal ventilation, and hypoventilation. Inspiratory (CIsev) and end-tidal (sev) sevoflurane concentrations were routinely measured by infrared analysis, and A sev were analyzed by gas chromatography for 40 min after intubation. Cardiac index and total peripheral vascular resistance were measured with a Finometer.
Results
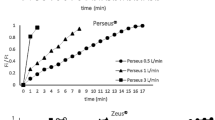
During the first 10 min after sevoflurane administration, A sev in the hyperventilation group was the highest and differed significantly from those in the normal ventilation group, followed by those in the hypoventilation group. In addition, hyperventilation significantly increased the slope of A sev over time in the first 5 min, but there were no differences in slopes in the 5–10, 10–20, and 20–40 min periods, which indicates no difference in sevoflurane bodily uptake among the three groups after 5 min.
Conclusion
Hyperventilation accelerated the rate of A sev increase immediately after sevoflurane administration, which was time dependent with respect to different alveolar ventilation levels.


Similar content being viewed by others
References
Lin TC, Lu CC, Li CY, Chang CC, Ho ST. Arterial blood concentration of sevoflurane during single-breath induction and tracheal intubation in gynecologic patients. J Clin Anesth. 2008;20:496–500.
Lin TC, Lu CC, Kuo CK, Hsu CH, Huang GS, Liu JY, Ho ST. Single vital-capacity and successive tidal-volume breathing of sevoflurane in induction of anesthesia for tracheal intubation in gynecologic patients. Acta Anaesthesiol Taiwan. 2008;46:66–70.
Lu CC, Tsai CS, Ho ST, Chen WY, Wong CS, Wang JJ, Hu OY, Lin CY. Pharmacokinetics of sevoflurane uptake into the brain and body. Anaesthesia. 2003;58:951–6.
Nakamura M, Sanjo Y, Ikeda K. Predicted sevoflurane partial pressure in the brain with an uptake and distribution model comparison with the measured value in internal jugular vein blood. J Clin Monit Comput. 1999;15:299–305.
Wissing H, Kuhn I, Rietbrock S, Fuhr U. Pharmacokinetics of inhaled anaesthetics in a clinical setting: comparison of desflurane, isoflurane and sevoflurane. Br J Anaesth. 2000;84:443–9.
Enekvist B, Bodelsson M, Sturesson LW, Johansson A. Larger tidal volume increases sevoflurane uptake in blood: a randomized clinical study. Acta Anaesthesiol Scand. 2010;54:1111–6.
Guelen I, Westerhof BE, Van Der Sar GL, Van Montfrans GA, Kiemeneij F, Wesseling KH, Bos WJ. Finometer, finger pressure measurements with the possibility to reconstruct brachial pressure. Blood Press Monit. 2003;8:27–30.
Lu CC, Lin TC, Yu MH, Chen TL, Lin CY, Chiang JS, Ho ST. Effects of changes in alveolar ventilation on isoflurane arterial blood concentration and its uptake into the human body. Pharmacology. 2009;83:150–6.
Nunn JF. Applied respiratory physiology. 2nd ed. London: Butterworths; 1977. p. 63–70.
Diggle P, Liang K-Y, Zeger SL. Analysis of longitudinal data. Oxford: Clarendon Press/Oxford University Press.
Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–30.
Lin CY. Uptake of anaesthetic gases and vapours. Anaesth Intensive Care. 1994;22:363–73.
Weismann D, Reissmann H, Maisch S, Fullekrug B, Schulte J. Monitoring of functional residual capacity by an oxygen washin/washout; technical description and evaluation. J Clin Monit Comput. 2006;20:251–60.
Di Marco F, Rota Sperti L, Milan B, Stucchi R, Centanni S, Brochard L, Fumagalli R. Measurement of functional residual capacity by helium dilution during partial support ventilation: in vitro accuracy and in vivo precision of the method. Intensive Care Med. 2007;33:2109–15.
Gray WM. A static calibration method for the gas chromatographic determination of per cent concentrations of volatile anaesthetic agents. Br J Anaesth. 1986;58:345–52.
Smith MA, Sapsed-Byrne SM, Lockwood GG. A new method for measurement of anaesthetic partial pressure in blood. Br J Anaesth. 1997;78:449–52.
Acknowledgments
This work was carried out in Tri-Service General Hospital/National Defense Medical Center, Taipei, Taiwan. It was supported by a grant (NSC96-2314-B-016-011-MY2) from the Taiwan National Council of Science.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix 1: Determination of blood/gas partition coefficient (λ) of sevoflurane in each patient’s blood
To obtain standard gas partial pressures, five 550-ml glass bottles, each with a turnable stopcock and Teflon septum were used [15]. After flushing each bottle with nitrogen for 6 min, each septum was pierced with the needle of a syringe, and 2, 5, 10, 20, or 50 μl of liquid sevoflurane at 20 °C was injected into the bottles. About 225 μl from each bottle of the calculated sevoflurane gas was then injected into a gas chromatograph using a 250-μl gas-tight Hamilton syringe (no. 81156). The calculated volume percent of sevoflurane was plotted against the measured gas chromatography counts. (Partial pressure was obtained by calculating the volume percent/100 × barometric pressure.)
We used a similar method to that described by Smith et al. [16] to determine blood/gas partition coefficient of sevoflurane (λ), as follows. Two milliliters of blood from each patient with an unknown sevoflurane partial pressure was added to the first 10-ml vial (with 2 ml of gas removed before injection), sealed with a Teflon septum in a 20 °C temperature room and then incubated at 37 °C for 30 min. The sevoflurane partial pressure in the headspace of the first vial (C1) was determined by GC. One milliliter of sample was immediately withdrawn from the first vial and transferred to a second 10-ml vial (with 1 ml of gas removed before injection), sealed with a Teflon septum, and then incubated at 37 °C for another 30 min. The sevoflurane partial pressure in the headspace of the second vial (C2) was again determined by GC. Thus, λ was calculated by the following equation:
Appendix 2: Conversion of sevoflurane liquid to vapor by the known blood/gas partition coefficient (λ) of sevoflurane
The physical properties of sevoflurane were as follows: molecular weight/density (MW/D) was the volume of sevoflurane liquid; the blood/gas partition coefficient (sevoflurane) was 0.66 (0.63–0.69); MW of sevoflurane was 200.05; D at 20 °C was 1.5203.
According to the ideal gas law, 1 mole of sevoflurane (MW = 200.05 g) is equal to 22.4 L of sevoflurane vapor at 1 atm pressure and 0 °C. Therefore, 1 ml of sevoflurane vapor is 8.925 mg. As the temperature increases from 0 to 37 °C, 1 ml of sevoflurane vapor should be equal to 7.859 mg [(273 K/37 + 273 K) × 8.925 mg]. The patient’s blood/gas partition coefficient was obtained as described in the above paragraph. If λ was assumed to be 0.66, a sample of 1 ml (1 % of 100 ml) of sevoflurane vapor equilibrated with 1 % 100 ml of blood contained 5.19 mg of sevoflurane. This means that 1 % of 100 ml of sevoflurane vapor (containing 7.859 mg) was equilibrated with 5.19 mg sevoflurane in 1 % of 100 ml of blood at 37 °C and 1 atm. Blood concentration (or partial pressure) of sevoflurane could be 1 %, which was comparable with the 1 % level of the gas phase. The 1 % blood concentration (or partial pressure) of sevoflurane indicated that there was 5.19 mg of sevoflurane liquid dissolved in the 100-ml blank blood sample of the patient, which was calculated according to the known blood/gas partition coefficient.
A standard of liquid sevoflurane was equilibrated in a cold bath at 20 °C for 1 h before use. Five known amounts of sevoflurane liquid were taken up into a Hamilton 0.5-μl microsyringe (PN: 86259) and then injected into five 10-ml glass vials (each containing 1 ml of a patient’s blank blood). These vials were swirled in a cool bath at 20 °C for 30 min, and then transferred to a water bath at 37 °C for 30 min. The sevoflurane partial pressure in the blood was obtained and was comparable with the sevoflurane partial pressure in the gas phase. Blood samples were analyzed with a GC, a headspace sampler, and a flame-ionization detector. A linear relationship between signals for peak area of sevoflurane (y axis) and sevoflurane partial pressure (x axis) was obtained and revealed an excellent correlation, with a range of 0.9959–0.9999 between signal and sevoflurane partial pressure. The analytical range of sevoflurane partial pressure was 0.47–11.7 %. The partial pressure of sevoflurane in the blood phase was calculated from the calibration curve of a known amount of sevoflurane. The chromatographic area was proportional to the sevoflurane partial pressure over the entire range of partial pressures studied. The precision and accuracy were determined on spiked human samples at six partial pressures (0.47–11.7 %) with respect to the calibration graph prepared each day. The limit of detection (LOD) was 0.03 % ml−1 of gas based on a signal-to-noise ratio of 3. The limit of quantification (LOQ) of the method for standard samples was 0.1 % ml−1 of blood. The precision of the method was expressed as within-day and between-day coefficients of variation (%) of <7.9 %.
About this article
Cite this article
Lu, CC., Lin, TC., Hsu, CH. et al. Hyperventilation accelerates rise in arterial blood concentrations of sevoflurane in gynecologic patients. J Anesth 27, 35–42 (2013). https://doi.org/10.1007/s00540-012-1483-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-012-1483-6