Abstract
Background
Successful precut sphincterotomy (PS) in difficult biliary cannulation (DBC) requires a large incision for deroofing the papilla. However, the high complication rate poses a substantial problem, in addition to the need for expert skills. Pancreatic stent placement could facilitate this procedure. Needle-knife precut papillotomy with a small incision using a layer-by-layer method over a pancreatic stent (NKPP-SIPS) could potentially improve the success rate and reduce the complication rate of PS.
Aims
To validate the efficacy, feasibility and safety of NKPP-SIPS in DBC.
Methods
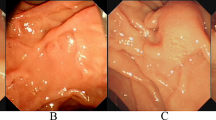
Therapeutic endoscopic retrograde cholangiopancreatography with a naïve papilla was performed in 1619 cases between May 2004 and July 2011. We prospectively divided the patients chronologically, in terms of the period during which the procedure was performed, into two groups: group A; needle-knife precut papillotomy (NKPP) performed between April 2004 and October 2006; group B; NKPP-SIPS performed between November 2006 and July 2011. The success rates and complication rates were evaluated. NKPP was performed without pancreatic stent placement and the cut was made starting at the papillary orifice, extended upward over a length of more than 5–10 mm for deroofing the papilla. On the other hand, in NKPP-SIPS, a pancreatic stent was placed initially as a guide, and to prevent post-ERCP pancreatitis, the incision was begun at the papillary orifice in a layer-by-layer fashion and extended upward in 1–2 mm increments, not going beyond the oral protrusion, finally measuring less than 5 mm in length.
Results
PS was performed in 8.3 % of the patients (134/1619). The cannulation success rate of PS in the entire group was 94.0 % (126/134). NKPP and NKPP-SIPS were performed in 36 and 98 of the patients, respectively. There was one case of major bleeding in group A, and no severe complications in group B. The success rates of bile duct cannulation increased from 86.1 % (31/36) in group A to 96.9 % (95/98) in group B (p = 0.0189). The overall complication rate of PS was YC 33 % (12/36) in group A (major bleeding 8.3 %; mild to moderate pancreatitis 19.4 %; perforation requiring surgery 2.8 %), and 7.1 % (7/98) in group B (mild to moderate pancreatitis 6.1 %; minor perforation 1 %) (p < 0.001).
Conclusions
NKPP-SIPS has significantly improved the success rate and reduced the complication rate of DBC, proving that a small incision starting at the orifice of the PS is sufficient, feasible and safe in DBC, when a pancreatic stent is inserted at the outset.




Similar content being viewed by others
References
Freeman ML, Disario JA, Nelson DB, Fennetry MB, Lee JG, Bjoukman DJ, et al. Risk factors for post-ERCP pancreatitis: a prospective, multicenter study. GIE. 2001;54:425–534.
Figueiredo FA, Pelosi AD, Machado L, Francioni E, Freitas G, Hatum PB, et al. Precut papillotomy: a risky technique not only for experts but also for average endoscopists skilled in ERCP. Dig Dis Sci. 2010;55:1485–9.
Fukatsu H, Kawamoto H, Harada R, Tsutsumi K, Fujii M, Kato H, et al. Quantitative assessment of technical proficiency in performing needle-knife precut papillotomy. Surg Endosc. 2009;23:2066–72.
Shah JN, Marson F, Weilert F, Bhat YM, Nguyen-Tang T, Binmoeller KF, et al. Single-operator, single-session EUS-guided anterograde cholangiopancreatography in failed ERCP or inaccessible papilla. GIE. 2012;75:56–64.
Siegel JH. Precut papillotomy: a method to improve success of ERCP and papillotomy. Endoscopy. 1980;12:130–3.
Donnellan F, Zeb F, Courtney G, Affab AR. Suprapapillary needle knife fistulotomy: a safe and effective method for accessing the biliary system. Surg Endsc. 2010;24:1937–40.
Freeman ML, Guda NM. ERCP cannulation: a review of reported techniques. GIE. 2005;61:112–25.
Huibregtse K, Katon RM, Tyygat GN. Precut papillotomy via fine-needle knife papillotome: a safe and effective technique. GIE. 1986;32:403–5.
Cavallini G, Tittobello A, Frulloni L, Masci E, Mariana A, Di Francesco V. Gabexate for the prevention of pancreatic damage related to endoscopic retrograde cholangiopancreatography. Gabexate in digestive endoscopy. Italian Group. N Engl J Med. 1996;335:919–23.
Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N. Endoscopic sphincterotomy complications and their management: an attempt at consensus. GIE. 1991;37:383–93.
Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335:909–18.
Coté GA, Ansstas M, Pawa R, Edmundowicz SA, Jonnalagadda SS, Pleskow DK, Azar RR. Difficult biliary cannulation: use of physician-controlled wire-guided cannulation over a pancreatic duct stent to reduce the rate of precut sphincterotomy (with video). GIE. 2010;71:275–9.
Wang P, Zhang W, Liu F, Li ZS, Ren X, Fan ZN, et al. Success and complication rates of two precut techniques, transpancreatic sphincterotomy and needle-knife sphincterotomy for bile duct cannulation. J Gastrointest Surg. 2010;14:697–704.
Bailey AA, Bourke MJ, Kaffes AJ, Byth K, Lee EY, Williams SJ. Needle knife sphincterotomy: factors predicting its use and the relationship with post-ERCP pancreatitis. GIE. 2010;71:266–71.
Manes G, Giorgio PD, Repici A, Macarri G, Ardizzone S, Porro GB. An analysis of the factors associated with the development of complications in patients undergoing precut sphincterotomy: a prospective, controlled, randomized, multicenter study. Am J Gastroenterol. 2009;104:2412–7.
Cennamo V, Fuccio L, Repici A, Fabbri C, Grilli D, Conio M, et al. Timing of precut procedure does not influence success rate and complications of ERCP procedure: a prospective randomized comparative study. GIE. 2009;69:473–9.
Kaffes AJ, Srian PVJ, Rao GV, Santosh D, Reddy N. Early institution of pre-cutting for difficult cannulation: a prospective study comparing conventional vs. a modified technique. GIE. 2005;62:669–74.
Mavrogiannis C, Liatsos C, Romanos A, Petoumenos C, Nakos A, Karvountzis G. Needle knife fistulotomy versus needle-knife precut papillotomy for the treatment of common bile duct stones. GIE. 1999;50:334–9.
Gong B, Hao L, Bie L, Sun B, Wang M. Does precut technique improve selective bile duct cannulation or increase post-ERCP pancreatitis rate? A meta-analysis of randomized controlled trials. Surg Endosc. 2010;24:2670–80.
Goldberg E, Titus M, Haluszka O, Darwin P. Pancreatic-duct stent placement facilitates difficult common bile duct cannulation. GIE. 2005;62:592–6.
Cotton PB. Precut papillotomy—a risky technique for experts only. GIE. 1989;35:578–9.
Bruins Slot W, Schoeman MN, Disario JA, Wolters F, Tytgat GN, Huibregtse K. Needle-knife sphincterotomy as a precut procedure: a retrospective evaluation of efficacy and complications. Endoscopy. 1996;28:334–9.
Masci E, Mariani A, Curioni S, Testoni PA. Risk factors for pancreatitis following endoscopic retrograde cholangiopancreatography: a meta-analysis. Endoscopy. 2003;35:830–4.
Akashi R, Kiyozumi T, Jinnouchi K, Yoshida M, Adachi Y, Sagara K. Pancreatic sphincter precutting to gain selective access to the common bile duct: a series of 172 patients. Endoscopy. 2004;36:405–10.
Halttumen J, Keranen I, Udd M, Kylanpaa L. Pancreatic sphincterotomy versus needle knife precut in difficult biliary cannulation. Surg Endsc. 2009;745–749.
Katsinelos P, Gkagkalis S, Chatzimavroudis G, Beltssi A, Terzoudis S, Zavos C, et al. Comparison of three types of precut technique to archive common bile duct cannulation: a retrospective analysis of 274 cases. Dig Dis Sci. 2012 (E-pub).
Conflict of interest
Drs. Kensuke Kubota, Takamitsu Sato, Shingo Kato, Seitaro Watanabe, Kunihiro Hosono, Noritoshi Kobayashi, Kantaro Hisatomi, Nobuyuki Matsuhashi and Atsushi Nakajima have no interest or financial ties to disclosure.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Kubota, K., Sato, T., Kato, S. et al. Needle-knife precut papillotomy with a small incision over a pancreatic stent improves the success rate and reduces the complication rate in difficult biliary cannulations. J Hepatobiliary Pancreat Sci 20, 382–388 (2013). https://doi.org/10.1007/s00534-012-0552-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00534-012-0552-4