Summary
Background
Glucometabolic status is an important predictor of prognosis in patients with acute myocardial infarction. Both plasma glucose levels and glycosylated hemoglobin A1c (HbA1c) were implicated as predictors of prognosis. However, previous data yielded conflicting results. We evaluated the prognostic role of plasma glucose levels and HbA1c in patients with non-ST elevation acute coronary syndrome (NSTEACS).
Methods
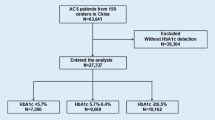
A total of 106 consecutive patients with NSTEACS (55 with unstable angina and 51 with non-ST elevation myocardial infarction) were included. The average age was 66.1 years; 61 % were male. HbA1c was measured at admission, along with other standard laboratory values. The follow-up period lasted for a year. The main combined outcome variable included death from cardiovascular causes and rehospitalization due to another acute coronary syndrome or due to heart failure.
Results
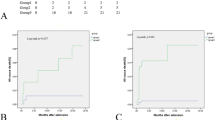
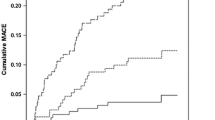
Combined end point occurred in 43 (41 %) patients. Mean HbA1c value was significantly higher in the group of patients who had complications (7.6 ± 2.6 vs. 5.8 ± 1.2, p < 0.05). Logistic regression identified HbA1c [odds ratio (OR): 1.6] and male sex (OR: 0.25) as the only independent predictors of major adverse cardiac events (MACE). A Kaplan–Meier analysis showed a 2.7 times higher risk of MACE in patients with HbA1c > 6.5 %.
Conclusions
Results from our study indicate that the admission level of HbA1c, but not admission or fasting glucose, is a predictor of mortality and major adverse events in patients with NSTEACS. These results identify HbA1c to be an independent predictor also in patients with NSTEACS, and not only in those with ST elevation myocardial infarction as observed before our study.
Zusammenfassung
Grundlagen
Glukosemetabolismus ist ein wichtiger Prädiktor für die Prognose bei Patienten mit akutem Herzinfarkt (AMI). Die Plasma Glucose-Konzentration sowie glykosyliertes Hämoglobin (HbA1c) waren Prädiktoren für die Prognose. Vorherige Daten brachten aber widersprüchliche Ergebnisse. Wir untersuchten die prognostische Rolle der Plasma Glucose-Konzentrationen und HbA1c bei Patienten mit akutem Koronarsyndrom ohne ST-Hebungen (NSTEACS).
Methodik
106 Patienten mit NSTEACS (55 mit instabiler Angina und 51 mit Nicht-ST-Hebungsinfarkt) wurden im prospektiven Design inkludiert. Das durchschnittliche Alter war 66,1 Jahre, 61 % waren Männer. HbA1c wurde bei der Einlieferung gemessen, gemeinsam mit den anderen Standardlaborwerten. Die Nachbeobachtungszeit dauerte ein Jahr. Die Zielvariable schließt Tod durch kardiovaskulare Ursachen und Rehospitalisierung wegen eines anderen akuten Koronarsyndroms oder wegen der Herzinsuffizienz ein (Major Adverse Cardiac Events – MACE).
Ergebnisse
Der kombinierte Endpunkt erschien bei 43 (41 %) Patienten. Der durchschnittliche HbA1c-Wert war deutlich höher bei der Gruppe der Patienten mit Störungen (7,6 ± 2,6 vs. 5,8 ± 1,2, p < 0,05). Die logistische Regression identifizierte nur HbA1c (OR 1,6) und das männliche Geschlecht (OR 0,25) als unabhängige Prädiktoren des MACE. Die Kaplan-Meier-Analyse zeigte ein 2,7 mal höheres MACE-Risiko bei Patienten mit HbA1c > 6,5 %.
Schlussfolgerungen
Die Ergebnisse unserer Studie zeigen, dass nur HbA1c zum Zeitpunkt der klinischen Aufnahme und nicht die Nüchternglukose-Konzentration ein Prädiktor für die Mortalität und MACE bei Patienten mit NSTEACS ist. Diese Ergebnisse erweitern frühere Beobachtungen über den prognostischen Wert von HbA1c bei Patienten mit ST-Hebungsinfarkt auf die NSTEACS-Gruppe.

Similar content being viewed by others
References
Mak KH, Moliterno DJ, Granger CB, et al. Influence of diabetes mellitus on clinical outcome in the thrombolytic era of acute myocardial infarction. GUSTO-I Investigators. Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries. J Am Coll Cardiol 1997;30:171–9.
Waldecker B, Waas W, Haberbosch W, et al. Type 2 diabetes and acute myocardial infarction. Angiographic findings and results of an invasive therapeutic approach in type 2 diabetic versus nondiabetic patients. Diabetes Care. 1999;22:1832–8.
Norhammar A, Malmberg K, Diderholm E, et al. Diabetes mellitus: the major risk factor in unstable coronary artery disease even after consideration of the extent of coronary artery disease and benefits of revascularization. J Am Coll Cardiol. 2004;43:585–91.
Aguilar D, Solomon SD, Kober L, et al. Newly diagnosed and previously known diabetes mellitus and 1-year outcomes of acute myocardial infarction: the VALsartan In Acute myocardial iNfarcTion (VALIANT) trial. Circulation. 2004;110:1572–8.
Harjai KJ, Stone GW, Boura J, et al. Comparison of outcomes of diabetic and non-diabetic patients undergoing primary angioplasty for acute myocardial infarction. Am J Cardiol. 2003;91:1041–5.
Adlerberth AM, Rosengren A, Wilhelmsen L. Diabetes and long-term risk of mortality from coronary and other causes in middle-aged Swedish men. A general population study. Diabetes Care. 1998;21:539–45.
Husband DJ, Alberti KG, Julian DG. ‘Stress’ hyperglycaemia during acute myocardial infarction: an indicator of preexisting diabetes? Lancet. 1983;II:179–81.
Haffner SM, Lehto S, Ronnemaa T, Pyorala K, Laakso M. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med. 1998;339:229–34.
Norhammar AM, Ryden L, Malmberg K. Admission plasma glucose, independent risk factor for long-term prognosis after myocardial infarction even in nondiabetic patients. Diabetes Care. 1999;22:1827–31.
Capes SE, Hunt D, Malmberg K, Gerstein HC. Stress hyperglycaemia and increased risk of death after myocardial infarction in patients with and without diabetes, systematic overview. Lancet. 2000;355:773–8.
Wahab NN, Cowden EA, Pearce NJ, et al. on behalf of the ICONS Investigators. Is blood glucose an independent predictor of mortality in acute myocardial infarction in the thrombolytic era. J Am Coll Cardiol. 2002;40:1748–54.
Foo K, Cooper J, Deaner A, et al. A single serum glucose measurement predicts adverse outcomes across the whole range of acute coronary syndromes. Heart. 2003;89:512–6.
Kosiborod M, Rathore SS, Inzucchi SE, et al. Admission glucose and mortality in elderly patients hospitalized with acute myocardial infarction: implications for patients with and without recognized diabetes. Circulation. 2005;111:3078–86.
Nordin C, Amiruddin R, Rucker L, Choi J, Kohli A, Marantz PR. Diabetes and stress hyperglycemia associated with myocardial infarctions at an urban municipal hospital: prevalence and effect on mortality. Cardiol Rev. 2005;13:223–30.
Gasior M, Pres D, Stasik-Pres G, et al. Effect of blood glucose levels on prognosis in acute myocardial infarction in patients with and without diabetes, undergoing percutaneous coronary intervention. Cardiol J. 2008;15:422–30.
The International Expert Committee. International Expert Committee report on the role of the A1c assay in the diagnosis of diabetes. Diab Care. 2009;32:1327–34.
Chowdhury TA, Lasker SS. Elevated glycated haemoglobin in non-diabetic patients is associated with an increased mortality in myocardial infarction. Postgrad Med J. 1998;74:480–1.
Tenerz A, Nilsson G, Forberg R, et al. Basal glucometabolic status has an impact on long-term prognosis following an acute myocardial infarction in non-diabetic patients. J Intern Med. 2003;254:494–503.
Gustafsson I, Kistorp CN, Jaes MK, Faber JO, Dickstein K, Hildebrandt PR (OPTIMAAL Study group). Unrecognized glycometabolic disturbance as measured by hemoglobin A1C is associated with a poor outcome after acute myocardial infarction. Am Heart J. 2007;154:470–6.
Timmer JR, Ottervanger JP, Bilo HP, et al. Prognostic value of admission glucose and glycosylated haemoglobin levels in acute coronary syndromes. QJM. 2006;99:237–43.
Hadjadj S, Coisne D, Mauco G, et al. Prognostic value of admission plasma glucose and HBA in acute myocardial infarction. Diabet Med. 2005;21;305–10.
Thygesen C, Alpert JS, White HD on behalf of the joint ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial Infarction. Universal definition of myocardial infarction. Eur Heart J. 2007;28:2525–38.
Sinnaeve PR, Steg G, Fox KAA, et al. Association of elevated fasting glucose with increased short-term and 6-month mortality in ST-segment elevation and non-ST segment elevation acute coronary syndromes. Arch Intern Med. 2009;169:402–9.
Petursson P, Herlitz J, Caidahl K, et al. Admission glycaemia and outcome after acute coronary syndrome. Int J Cardiol. 2007;116:315–20.
Aronson D, Hammerman H, Suleiman M, Markiewicz W. Usefulness of changes in fasting glucose during hospitalization to predict long-term mortality in patients with acute myocardial infarction. Am J Cardiol. 2009;104:1013–7.
Suleiman M, Hammerman H, Boulos M, et al. Fasting glucose is an important independent risk factor for 30-day mortality in patients with acute myocardial infarction: A prospective study. Circulation. 2005;111:754–60.
Kosiborod M, Inzucchi SE, Krumholz HM, et al. Glucometrics in patients hospitalized with acute myocardial infarction: defining the optimal outcomes-based measure of risk. Circulation. 2008;117:1018–27.
Hamm CW, Bassand J-P, Agewall S, et al. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2011;32:2999–3054.
Hsu LF, Mak KH, Lau KW, et al. Clinical outcomes of patients with diabetes mellitus and acute myocardial infarction treated with primary angioplasty or fibrinolysis. Heart. 2002;88:260–5.
Conflict of interest
The authors have no conflict of interest to declare nor financial relationships to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kmet, M., Rajer, B. & Pernat, A. Hemoglobin A1c is a better predictor of prognosis following the non-ST elevation acute coronary syndrome than fasting and admission glucose. Wien Klin Wochenschr 126, 156–162 (2014). https://doi.org/10.1007/s00508-013-0468-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-013-0468-2