Abstract
Purpose
Actual 5-year survival rates after resection of colorectal liver metastases (CLM) are 25–45 %, whereas 10-year survival rates are extrapolated from survival curves. Few studies have reported long-term survivors with 10 years of actual follow-up. Therefore, no recurrences occurring after 10-plus years have been reported. The aim of our study was to analyze actual 10-year survival rates and prognostic factors.
Methods
Clinical data of patients with CLM who had undergone first liver resection in our center between January 1990 and December 2000 were retrospectively analyzed.
Results
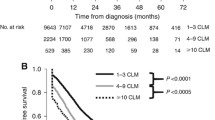
Eighty-nine patients of mean age 64 years were studied. Three patients were excluded from the study: one because of postoperative death, and two from being lost to follow-up. All other subjects had a potential 10-year follow-up. Only 33 % patients received perioperative chemotherapy. The actual 10-year overall and disease-free survival rate were 22 and 19 %, respectively. Poor prognostic factors were disease-free interval less than 1 year, wedge liver resection, clinical risk score >2, segment 1 CLM location, and peritumoral lymphangitis. Good prognostic factors were tumors having mucinous components in primary tumor and CLM located in the right lobe.
Conclusions
With actual long-term follow-up for 10 years, disease-free survival rate is 19 % and mainly depends on surgical management. Recurrence continues to occur more than 5 years after liver resection for CLM; cure cannot be assumed at this time. Clinical risk score is a good predictor of cure and should be taken into account when choosing perioperative treatment.


Similar content being viewed by others
References
Garden OJ, Rees M, Poston GJ, Mirza D, Saunders M, Ledermann J et al (2006) Guidelines for resection of colorectal cancer liver metastases. Gut 55(Suppl 3):iii1–iii8
Tomlinson JS, Jarnagin WR, DeMatteo RP, Fong Y, Kornprat P, Gonen M et al (2007) Actual 10-year survival after resection of colorectal liver metastases defines cure. J Clin Oncol 25(29):4575–4580
Viganò L, Ferrero A, Lo Tesoriere R, Capussotti L (2008) Liver surgery for colorectal metastases: results after 10 years of follow-up. Long-term survivors, late recurrences, and prognostic role of morbidity. Ann Surg Oncol 15(9):2458–2464
Pulitanò C, Castillo F, Aldrighetti L, Bodingbauer M, Parks RW, Ferla G et al (2010) What defines ‘cure’ after liver resection for colorectal metastases? Results after 10 years of follow-up. HPB (Oxford) 12(4):244–249
Nordlinger B, Sorbye H, Glimelius B, Poston GJ, Schlag PM, Rougier P et al (2008) Perioperative chemotherapy with FOLFOX4 and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC Intergroup trial 40983): a randomised controlled trial. Lancet 371(9617):1007–1016
Nordlinger B, Sorbye H, Glimelius B, Poston GJ, Schlag PM, Rougier P et al (2013) Perioperative FOLFOX4 chemotherapy and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC 40983): long-term results of a randomised, controlled, phase 3 trial. Lancet Oncol 14(12):1208–1215
Dindo D, Clavien P-A (2008) What is a surgical complication? World J Surg 32(6):939–941
Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH (1999) Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg 230(3):309–318, discussion 318–321
Lopez P, Marzano E, Piardi T, Pessaux P (2012) Repeat hepatectomy for liver metastases from colorectal primary cancer: a review of the literature. J Visc Surg 149(2):e97–e103
Kanemitsu Y, Kato T, Hirai T, Yasui K, Morimoto T, Shimizu Y et al (2003) Survival after curative resection for mucinous adenocarcinoma of the colorectum. Dis Colon Rectum 46(2):160–167
Song W, Wu S, He Y, Cai S, Zhang C, Zhang X et al (2009) Clinicopathologic features and survival of patients with colorectal mucinous, signet-ring cell or non-mucinous adenocarcinoma: experience at an institution in southern China. Chin Med J 122(13):1486–1491
Maksimović S (2007) Survival rates of patients with mucinous adenocarcinoma of the colorectum. Med Arh 61(1):26–29
Green JB, Timmcke AE, Mitchell WT, Hicks TC, Gathright JB Jr, Ray JE (1993) Mucinous carcinoma—just another colon cancer? Dis Colon Rectum 36(1):49–54
Kang H, O’Connell JB, Maggard MA, Sack J, Ko CY (2005) A 10-year outcomes evaluation of mucinous and signet-ring cell carcinoma of the colon and rectum. Dis Colon Rectum 48(6):1161–1168
King-Yin Lam A, Ong K, Ho Y-H (2006) Colorectal mucinous adenocarcinoma: the clinicopathologic features and significance of p16 and p53 expression. Dis Colon Rectum 49(9):1275–1283
Elias D, Saric J, Jaeck D, Arnaud JP, Gayet B, Rivoire M et al (1996) Prospective study of microscopic lymph node involvement of the hepatic pedicle during curative hepatectomy for colorectal metastases. Br J Surg 83(7):942–945
Schmidt T, Koch M, Antolovic D, Reissfelder C, Schmitz-Winnenthal FH, Rahbari NN et al (2008) Influence of two different resection techniques (conventional liver resection versus anterior approach) of liver metastases from colorectal cancer on hematogenous tumor cell dissemination—prospective randomized multicenter trial. BMC Surg 8:6
(2009) Cancérologie digestive: pratiques chirurgicales. J Chir 146:S11–S80
Abbas S, Lam V, Hollands M (2011) Ten-year survival after liver resection for colorectal metastases: systematic review and meta-analysis. ISRN Oncol 2011:763245
Scheele J, Altendorf-Hofmann A, Stangl R, Schmidt K (1996) Surgical resection of colorectal liver metastases: Gold standard for solitary and radically resectable lesions. Swiss Surg Suppl 4:4–17
Yasui K, Shimizu Y (2005) Surgical treatment for metastatic malignancies. Anatomical resection of liver metastasis: indications and outcomes. Int J Clin Oncol 10(2):86–96
Sarpel U, Bonavia AS, Grucela A, Roayaie S, Schwartz ME, Labow DM (2009) Does anatomic versus nonanatomic resection affect recurrence and survival in patients undergoing surgery for colorectal liver metastasis? Ann Surg Oncol 16(2):379–384
Acknowledgments
Marc Puyraveau equally contributed to this paper.
Author’s contributions
Study conception and design: Nicolas Bouviez , Georges Mantion.
Acquisition of data: Nicolas Bouviez.
Analysis and interpretation of data: Nicolas Bouviez.
Drafting of manuscript: Nicolas Bouviez.
Critical revision of manuscript: Georges Mantion, Zaher Lakkis, Jean Lubrano, Tuxun Tuerhongjiang, Brice Paquette, Bruno Heyd.
All authors have read and reviewed the final version of the manuscript.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bouviez, N., Lakkis, Z., Lubrano, J. et al. Liver resection for colorectal metastases: results and prognostic factors with 10-year follow-up. Langenbecks Arch Surg 399, 1031–1038 (2014). https://doi.org/10.1007/s00423-014-1229-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-014-1229-z