Abstract
Background
Since the detection of autoantibodies against neuronal surface antigens, autoimmune encephalitis (AE) has been more frequently diagnosed, especially in patients with symptoms typical of limbic encephalitis, such as seizures, short-term memory deficits, or psychosis. However, the clinical spectrum of AE may be much wider, making correct clinical diagnosis difficult.
Methods
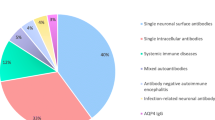
We retrospectively analysed symptoms and admission diagnoses at first clinical presentation in 50 AE patients. We included patients with a clinical diagnosis of AE for whom a FDG-PET imaging was available. Final diagnoses were re-evaluated by a blinded investigator according to the most recent consensus suggestions published in 2016 for AE diagnostic criteria. We additionally describe two patients with Morvan syndrome who showed CASPR2 antibodies.
Results
In 40 patients (80.0%), the clinical presentation at first admission was typical for AE. Ten patients (20.0%) initially suffered from atypical symptoms; among these patients, isolated headache and cerebellar dysfunction were most frequent (three patients each). However, an initial diagnosis of suspected encephalitis was only reached in 16 patients (32.0%), nine (18.0) of which were suspected to have infectious encephalitis, and seven (14.0%) patients were suspected to have AE. In 34 patients (68.0%), a diagnosis other than encephalitis was considered, (e.g., epilepsy, psychiatric diseases, transient ischemic attack, dementia, meningitis, and cerebellitis).
Conclusions
These data show the broad spectrum of initial symptoms of AE; the correct initial diagnosis of AE is often missed or delayed. Hence, clinicians in neurological and psychiatric hospitals should consider AE in the differential diagnosis of cases with atypical clinical presentations.
Similar content being viewed by others
References
Graus F, Titulaer MJ, Balu R et al (2016) A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol 15(4):391–404
Dalmau J, Lancaster E, Martinez-Hernandez E, Rosenfeld MR, Balice-Gordon R (2011) Clinical experience and laboratory investigations in patients with anti-NMDAR encephalitis. Lancet Neurol 10(1):63–74
Dalmau J. Neurology (2016) NMDA receptor encephalitis and other antibody-mediated disorders of the synapse: the 2016 Cotzias lecture. Neurology 87(23):2471–2482
Lancaster E, Dalmau J (2011) Encephalitis and antibodies to synaptic and neuronal cell surface proteins. Neurology 77(2): 179–189
Zuliani L, Graus F, Giometto B, Bien C, Vincent A (2012) Central nervous system neuronal surface antibody associated syndromes: review and guidelines for recognition. J Neurol Neurosurg Psychiatry 83(6):638–645
Tofaris GK, Irani SR, Cheeran BJ, Baker IW, Cader ZM, Vincent A (2012) Immunotherapy-responsive chorea as the presenting feature of LGI1-antibody encephalitis. Neurology 79(2):195–196
Klein CJ, Lennon VA, Aston PA, McKeon A, Pittock SJ (2012) Chronic pain as a manifestation of potassium channel-complex autoimmunity. Neurology 79(11):1136–1144
Tsuyusaki Y, Sakakibara R, Kishi M, Tateno F, Yoshida T (2014) Downbeat nystagmus as the initial manifestation of anti-NMDAR encephalitis. Neurol Sci 35(1):125–126
Jarius S, Steinmeyer F, Knobel A, Streitberger K, Hotter B, Horn S, Heuer H, Schreiber SJ, Wilhelm T, Trefzer U, Wildemann B, Ruprecht K (2013) GABAB receptor antibodies in paraneoplastic cerebellar ataxia. J Neuroimmunol 256(1–2):94–96
Vincent A, Bien CG, Irani SR, Waters P (2011) Autoantibodies associated with diseases of the CNS: new developments and future challenges. Lancet Neurol 10:759–772
Dalmau J, Gleichman AJ, Hughes EG, Rossi JE, Peng X, Lai M, Dessain SK, Rosenfeld MR, Balice-Gordon R, Lynch DR (2008) Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol 7(12):1091–1098
Sühs KW, Wegner F, Skripuletz T, Trebst C, Tayeb SB, Raab P, Stangel M (2015) Heterogeneity of clinical features and corresponding antibodies in seven patients with anti-NMDA receptor encephalitis. Exp Ther Med 10(4):1283–1292
Byrne S, McCoy B, Lynch B, Webb D, King MD (2014) Does early treatment improve outcomes in N-methyl-d-aspartate receptor encephalitis? Dev Med Child Neurol 56(8):794–796
Schankin CJ, Kästele F, Gerdes LA et al (2016) New-onset headache in patients with autoimmune encephalitis is associated with anti-NMDA-receptor antibodies. Headache 56(6):995–1003
Pandit AK, Ihtisham K, Garg A, Gulati S, Padma MV, Tripathi M (2013 Oct-Dec) Autoimmune encephalitis: a potentially reversible cause of status epilepticus, epilepsy, and cognitive decline. Ann Indian Acad Neurol 16(4):577–584
Titulaer MJ, McCracken L, Gabilondo I et al (2013) Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort study. Lancet Neurol 12(2):157–165
Titulaer MJ, Höftberger R, Iizuka T et al (2014 Mar) Overlapping demyelinating syndromes and anti–N-methyl-d-aspartate receptor encephalitis. Ann Neurol 75(3):411–428
Herken J, Prüss H (2017) Red flags: clinical signs for identifying autoimmune encephalitis in psychiatric patients. Front Psychiatry 8:25
Correll CM (2013) Antibodies in epilepsy. Curr Neurol Neurosci Rep 13(5):348
Van Sonderen A, Schreurs MW, de Bruijn MA, Boukhrissi S, Nagtzaam MM, Hulsenboom ES, Enting RH, Thijs RD, Wirtz PW, Sillevis Smitt PA, Titulaer MJ (2016) The relevance of VGKC positivity in the absence of LGI1 and Caspr2 antibodies. Neurology 86(18):1692–1699
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
S.R. received consulting and lecture fees, grant and research support from Bayer Vital GmbH, Biogen Idec, Merck Serono, Novartis, Sanofi-Aventis and Teva. He is a founding member of ravo Diagnostika GmbH, Freiburg. F.L. disclosures receiving speakers honoraria from Grifols, Teva, Biogen, Merck, Roche and Fresenius. He is employed by an academic institution offering commercial antibody testing. H.H. has participated in meetings sponsored by received speaker honoraria or travel funding from Bayer, Biogen, Merck, Novartis, Sanofi-Genzyme, Teva, and received honoraria for acting as consultant for Teva. J.L. has received honoraria for speaking and travel grants from Bayer, TEVA, CHDI and the Movement Disorders Society. F.D. has participated in meetings sponsored by or received honoraria for acting as an advisor/speaker for Biogen Idec, Celgene, Genzyme-Sanofi, Merck, Novartis Pharma, Roche, and TEVA ratiopharm. His institution has received research grants from Biogen and Genzyme Sanofi. He is section editor of the MSARD Journal (Multiple Sclerosis and Related Disorders). A.B., T.H., F.U., H.P. and O.S. report no conflicts of interest with this study. None of the authors has any financial or personal relationships with individuals or organisations that could inappropriately influence this submission.
Ethical standard
The authors confirm that the study is in accordance with ethical standards. The local ethics committee approved the study.
Rights and permissions
About this article
Cite this article
Baumgartner, A., Rauer, S., Hottenrott, T. et al. Admission diagnoses of patients later diagnosed with autoimmune encephalitis. J Neurol 266, 124–132 (2019). https://doi.org/10.1007/s00415-018-9105-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-018-9105-3