Abstract
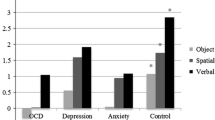
Visuospatial working memory (VSWM) is the ability of the brain to transiently store and manipulate visual information. VSWM deficiencies have been reported in obsessive–compulsive disorder (OCD), but not consistently, perhaps due to variability in task design and clinical patient factors. To explore this variability, this study assessed effects of the design factors task difficulty and executive organizational strategy and of the clinical factors gender, OCD symptom dimension, and duration of illness on VSWM in OCD. The CANTAB spatial working memory, spatial recognition memory, delayed matching to sample, and stop signal tasks were administered to 42 adult OCD patients and 42 age- and sex-matched healthy controls. Aims were to detect a possible VSWM deficit in the OCD sample, to evaluate influences of the above task and patient factors, to determine the specificity of the deficit to the visuospatial subdomain, and to examine effects of sustained attention as potential neurocognitive confound. We confirmed previous findings of a VSWM deficit in OCD that was more severe for greater memory load (task difficulty) and that was affected by task strategy (executive function). We failed to demonstrate significant deficits in neighboring or confounding neurocognitive subdomains (visual object recognition or visual object short-term memory, sustained attention). Notably, the VSWM deficit was only significant for female patients, adding to evidence for sexual dimorphism in OCD. Again as in prior work, more severe OCD symptoms in the symmetry dimension (but no other dimension) significantly negatively impacted VSWM. Duration of illness had no significant effect on VSWM. VSWM deficits in OCD appear more severe with higher task load and may be mediated through poor task strategy. Such deficits may present mainly in female patients and in (male and female) patients with symmetry symptoms.


Similar content being viewed by others
References
McAfoose J, Baune BT (2009) Exploring visual-spatial working memory: a critical review of concepts and models. Neuropsychol Rev 19(1):130–142
Baddeley AD, Hitch GJ (1974) Working memory. In: Bower G (ed) Recent advances in learning and motivation. Academic, New York, pp 47–89
Repovs G, Baddeley A (2006) The multi-component model of working memory: explorations in experimental cognitive psychology. Neuroscience 139(1):5–21
Vecchi T, Monticellai ML, Cornoldi C (1995) Visuo-spatial working memory: structures and variables affecting a capacity measure. Neuropsychologia 33(11):1549–1564
Ahmari SE, Eich E, Cebenoyan D, Smith EE, Simpson HB (2014) Assessing neurocognitive function in psychiatric disorders: a roadmap for enhancing consensus. Neurobiol Learn Mem. doi:10.1016/j.nlm.2014.06.011
Chang S, O’Neill J, Rosenberg DA (2013) Integration of neuropsychological assessment and clinical intervention for youth with obsessive–compulsive disorder. In: Reddy LA, Weissman AS, Hale JB (eds) Neuropsychological assessment and intervention for emotional and behavior disordered youth: an integrated step-by-step evidence-based approach. APA Press, Washington, DC, pp 41–72
Abramovitch A, Abramowitz JS, Mittelman A (2013) The neuropsychology of adult obsessive–compulsive disorder: a meta-analysis. Clin Psych Rev 33:1163–1171
Robbins TW, James M, Owen AM, Sahakian BJ, Lawrence AD, McInnes L, Rabbitt PM (1998) A study of performance on tests from the CANTAB battery sensitive to frontal lobe dysfunction in a large sample of normal volunteers: implications for theories of executive functioning and cognitive aging. Cambridge Neuropsychological Test Automated Battery. J Int Neuropsychol Soc 4(5):474–490
Purcell R, Maruff P, Kyrios M, Pantelis C (1998) Cognitive deficits in obsessive–compulsive disorder on tests of frontal–striatal function. Biol Psychiatry 43(5):348–357
Purcell R, Maruff P, Kyrios M, Pantelis C (1998) Neuropsychological deficits in obsessive–compulsive disorder: a comparison with unipolar depression, panic disorder, and normal controls. Arch Gen Psychiatry 55(5):415–423
Chamberlain SR, Fineberg NA, Blackwell AD, Clark L, Robbins TW, Sahakian BJ (2007) A neuropsychological comparison of obsessive–compulsive disorder and trichotillomania. Neuropsychologia 45(4):654–662
Chamberlain SR, Blackwell AD, Fineberg N, Robbins TW, Sahakian BJ (2005) The neuropsychology of obsessive compulsive disorder: the importance of failures in cognitive and behavioural inhibition as candidate endophenotypic markers. Neurosci Biobehav Rev 29(3):399–419
Grant JE, Potenza MN (2006) Compulsive aspects of impulse-control disorders. Psychiatr Clin North Am 29:539
Stein DJ, Simeon D, Cohen LJ, Hollander E (1995) Trichotillomania and obsessive–compulsive disorder. J Clin Psychiatry 56:28–34
Stein DJ, Grant JE, Franklin ME, Keuthen N, Lochner C, Singer SH, Woods DW (2010) Trichotillomania (hair pulling disorder), skin picking disorder, and stereotypic movement disorder: toward DSM-V. Depress Anxiety 27:611–626
Morein-Zamir S, Craig KJ, Ersche KD, Abbott S, Muller U, Fineberg NA, Bullmore ET, Sahakian BJ, Robbins TW (2010) Impaired visuospatial associative memory and attention in obsessive compulsive disorder but no evidence for differential dopaminergic modulation. Psychopharmacology 212(3):357–367
van der Wee NJ, Ramsey NF, Jansma JM, Deny DA, van Megen HJ, Westenberg HM, Kahn RS (2003) Spatial working memory deficits in obsessive compulsive disorder are associated with excessive engagement of the medial frontal cortex. Neuroimage 20(4):2271–2280
Harkin B, Kessler K (2011) The role of working memory in compulsive checking and OCD: a systematic classification of 58 experimental finding. Clin Psych Rev 31:1004–1021
de Vries FE, de Wit SJ, Cath DC, van der Werf YD, van der Borden V, van Rossum TB, van Balkom AJ, van der Wee NJ, Veltman DJ, van den Heuvel OA (2014) Compensatory frontoparietal activity during working memory: an endophenotype of obsessive compulsive disorder. Biol Psychiatry 76(11):878–887
Henseler I, Gruber O, Kraft S, Krick C, Reith W, Falkai P (2008) Compensatory hyperactivations as markers of latent working memory dysfunctions in patients with obsessive–compulsive disorder: an fMRI study. J Psychiatry Neurosci 33(3):209–215
Mathis MA, Alverenga PD, Funaro G, Torresan RC, Moraes I, Torres AR, Zilberman ML, Hounie AG (2011) Gender differences in obsessive–compulsive disorder: a literature review. Rev Bras Psiquiatr 33(4):390–399
Craske M (2003) Origins of phobias and anxiety disorders: Why more women than men?. Elsevier, Oxford
McCrae RR, Costa ET, Terracciano A, Parker WD, Mills CJ, De Fruyt E, Mervielde I (2002) Personality trait development from age 12 to 18: longitudinal, cross-sectional and cross-cultural analyses. J Personal Soc Psych 83:1456–1468
Weinberg MK, Tronick EZ, Cohn JE, Olson KL (1999) Gender differences in emotional expressivity and self-regulation during early infancy. Devel Psych 35:175–188
Borkovec TD, Lyonfields JD (1993) Worry: thought suppression of emotional processing. In: Krohne HW (ed) Attention and avoidance: strategies in coping with aversiveness. Hogrefe & Huber; Kirkland, WA, pp 101–118
Mor N, Winquist J (2002) Self-focused attention and negative affect: a meta-analysis. Psychol Bull 128:638–662
Pennebaker JW, Roberts T (1992) Toward a his and hers theory of emotion: gender differences in visceral perception. J Soc Clin Psych 11:199–212
Mataix-Cols D, Rahman Q, Spiller M, Alonso MP, Pifarré J, Menchón JM, Vallejo J (2006) Are there sex differences in neuropsychological functions among patients with obsessive–compulsive disorder? Appl Neuropsychol 13(1):42–50
Segalàs C, Alonso P, Labad J, Real E, Pertusa A, Jaurrieta N, Jiménez-Murcia S, Menchòn JM, Vallejo J (2010) A case–control study of sex differences in strategic processing and episodic memory in obsessive–compulsive disorder. Comp Psychiatry 51:303–311
Nedeljkovic M, Kyrios M, Moulding R, Doron G, Wainwright K, Pantelis C, Purcell R, Maruf P (2009) Differences in neuropsychological performance between subtypes of obsessive–compulsive disorder. Aust N Z J Psychiatry 43(3):216–226
Nakao T, Nakagawa A, Yoshiura T, Nakatani E, Nabeyama M, Sanematsu H, Togao O, Yoshioka K, Tomita M, Kuroki T, Kanba S (2009) Duration effect of obsessive–compulsive disorder on cognitive function: a functional MRI study. Depress Anxiety 26(9):814–823
American Psychiatric Association (2000) Diagnostic and statistical manual of mental disorders, 4th edn—TR. American Psychiatric Publishing, Arlington
Segalàs C, Alonso P, Labad J, Jaurrieta N, Real E, Jiménez S, Menchón JM, Vallejo J (2008) Verbal and nonverbal memory processing in patients with obsessive–compulsive disorder: its relationship to clinical variables. Neuropsychology 22(2):262–272
Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC (1998) The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 59(Suppl 20):22–33
Spielberger GO (1970) The State-Trait Anxiety Inventory. Consulting Psychologists Press, Palo Alto
Rosario-Campos MC, Miguel EC, Quatrano S, Chacon P, Ferrao Y, Findley D, Katsovich L, Scahill L, King RA, Woody SR, Tolin D, Hollander E, Kano Y, Leckman JF (2006) The Dimensional Yale-Brown Obsessive–Compulsive Scale (DY-BOCS): an instrument for assessing obsessive–compulsive symptom dimensions. Mol Psychiatry 11(5):495–504
Linn MC, Petersen AC (1985) Emergence and characterization of sex differences in spatial ability: a meta-analysis. Child Dev 56(6):1479–1498
Janowsky JS, Chiavez B, Orwoll E (2000) Sex steroid modify working memory. J Cogn Neurosci 12(3):407–414
Maki PM, Resnick SM (2000) Longitudinal effects of estrogen replacement therapy on PET cerebral blood flow and cognition. Neurobiol Aging 21(2):373–383
Peinado V, Gonzàlez JC, Leret ML (2004) Effect of 17-beta-estradiol on dopamine, serotonine and GABA striatal levels in 6-hydroxydopamine-trated rats. Toxicology 204(2–3):155–160
Aouizerate B, Guehl D, Cuny E, Rougier A, Burbaud P, Tignol J, Bioulac B (2005) Updated overview of the putative role of the serotoninergic system in obsessive–compulsive disorder. Neuropsychitr Dis Treat 1(3):231–243
Gong P, Li J, Wang J, Lei X, Chen D, Zhang K, Zhang W, Zhen A, Gao X, Zhang F (2011) Variations in 5-HT2A influence spatial cognitive abilities and working memory. Can J Neurol Sci 38(2):303–308
Labad J, Menchòn JM, Alonso P, Segalàs C, Jiménez S, Vallejo J (2005) Female reproductive cycle and obsessive–compulsive disorder. J Clin Psychiatry 66(4):428–435
Vulink NC, Denys D, Bus L, Westenberg HG (2006) Female hormones affect severity in obsessive compulsive disorder. Int Clin Psychopharmacol 21(3):171–175
Owen AM, Downes JJ, Sahakian BJ, Polkey CE, Robbins TW (1990) Planning and spatial working memory following frontal lobe lesions in man. Neuropsychologia 28(10):1021–1034
Kuelz AK, Hohagen F, Voderholzen U (2004) Neuropsychological performence in obsessive–compulsive disorder: a critical review. Biol Psych 65(3):185–236
Greisberg S, McKay D (2003) Neuropsychology of obsessive–compulsive disorder: a review and treatment implications. Clin Psychol Rev 23(1):95–117
Buhlmann U, Deckersbach T, Engelhard I, Cook LM, Rauch SL, Kathmann N, Wilhelm S, Savage CR (2006) Cognitive retraining for organizational impairment in obsessive–compulsive disorder. Psychiatry Res 144(2–3):109–116
Park HS, Shin YW, Ha TH, Shin MS, Kim YY, Lee YH, Kwon JS (2006) Effect of cognitive training focusing on organizational strategies in patients with obsessive–compulsive disorder. Psychiatry Clin Neurosci 60(6):718–726
Mataix-Cols D, Rosario-Campos MC, Leckman JF (2005) A multi-dimensional model of obsessive–compulsive disorder. Am J Psychiatry 162:228–238
Martoni RM, Brombin C, Nonis A, Salgari GC, Buongiorno A, Cavallini MC, Galimberti E, Bellodi L (in press). Evaluating effect of symptoms heterogeneity on decision-making ability in obsessive–compulsive disorder. Psychiatry Clin Neurosci. doi:10.1111/pcn.12264
Prasko J, Raszka M, Adamcova K, Grambal A, Koprivova J, Kudrnovská H, Latalova K, Vyskocilová J (2009) Predicting the therapeutic response to cognitive behavioural therapy in patients with pharmacoresistant obsessive–compulsive disorder. Neuroendocrin Lett 30(5):615–623
Williams MT, Farris SG, Turkheimer EN, Franklin ME, Simpson HB, Liebowitz M, Foa EB (2014) The impact of symptom dimensions on outcome for exposure and ritual prevention therapy in obsessive–compulsive disorder. J Anxiety Disord 28(6):553–558
Chamberlain S, Blackwell AD, Fineberg NA, Robbins T, Sahakian B (2005) Strategy implementation in obsessive–compulsive disorder and trichotillomania. Psychol Med 35:1–7
Dell’Osso B, Benatti B, Buoli M, Altamura AC, Marazziti D, Hollander E, Fineberg N, Stein DJ, Pallanti S, Nicolini H, Ameringen MV, Lochner C, Hranov G, Karamustafalioglu O, Hranov L, Menchon JM, Zohar J, ICOCS Group (2013) The influence of age at onset and duration of illness on long-term outcome in patients with obsessive–compulsive disorder: a report from the International College of Obsessive Compulsive Spectrum Disorders (ICOCS). Eur Neuropsychopharmacol 23(8):865–871
Nielen MM, Den Boer JA (2003) Neuropsychological performance of OCD patients before and after treatment with fluoxetine: evidence for persistent cognitive deficits. Psychol Med 33(5):917–925
Acknowledgments
All authors are grateful to Professor Laura Bellodi for the deepening of her support in this project.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Martoni, R.M., Salgari, G., Galimberti, E. et al. Effects of gender and executive function on visuospatial working memory in adult obsessive–compulsive disorder. Eur Arch Psychiatry Clin Neurosci 265, 707–718 (2015). https://doi.org/10.1007/s00406-015-0604-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-015-0604-2