Abstract
Objective
Our objective was to evaluate the efficacy and safety of Batroxobin on blood loss during spinal operations.
Methods
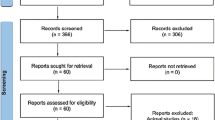
After obtaining approval from the ethics committee at the hospital along with informed written consent, we performed a double-blind, randomized, placebo-controlled study with 100 patients who were randomized equally into 2 groups (Batroxobin and placebo). Patients received either 2 ku IV 15 min before surgery and followed 1 ku IM of Batroxobin following surgery, or an equivalent volume of placebo (normal saline). Cost of Batroxobin treatment is amounted to 84.75 euros. The primary outcomes were intraoperative, 24 h postoperative, and total perioperative blood loss. Secondary outcomes were hemoglobin (Hb), red blood cell count (RBC), the volume of blood/fluid transfusion intraoperatively, and 24 h postoperatively. Safety evaluation parameters were the incidence of venous thrombosis in the lower extremities, active partial thromboplastin time, prothrombin time, thrombin time, and fibrinogen. The data were analyzed using the Statistical Package for the Social Science Version 12.0. The results were presented as mean ± SEM. The Mann–Whitney test and Independent Student t test, when appropriate, were used to compare the 2 groups, and differences were considered significant if the P value was <0.05.
Results
88 patients were included in the analysis while 12 patients were withdrawn from the study due to extended surgical duration, change of surgical procedure, or after the patients’ request. The total perioperative blood loss was approximately 31 % lower in patients given Batroxobin versus placebo (700.5 ± 45.81 vs 485.7 ± 30.01 mL, P = 0.001). The Batroxobin group had significantly less intraoperative blood loss (326.1 ± 24.16) compared to the placebo group (556.0 ± 43.58), but there was no difference in the amount of blood/fluid transfused, postoperatively Hb, or RBC between the two groups. After the operation, coagulation parameters were not significantly different between the 2 groups at the days 1 or 3 postoperatively. No adverse events related to the use of Batroxobin were recorded. There were no cases of superficial wound infection. None of the subjects died during the study.
Conclusions
In this study, prophylactic use of Batroxobin provided an effective and cheap method for reducing blood loss without coagulopathy during or after operations. The use of Batroxobin for patients undergoing one-level PLIF surgery safely and effectively reduced the total amount of perioperative blood loss.
Similar content being viewed by others
References
Alshryda S, Sarda P, Sukeik M, Nargol A, Blenkinsopp J, Mason JM (2011) Tranexamic acid in total knee replacement: a systematic review and meta-analysis. J Bone Joint Surg Br 93(12):1577–1585
Alshryda S, Sukeik M, Sarda P, Blenkinsopp J, Haddad FS, Mason JM (2014) A systematic review and meta-analysis of the topical administration of tranexamic acid in total hip and knee replacement. Bone Joint J 96-B(8):1005–1015
Baldus CR, Bridwell KH, Lenke LG, Okubadejo GO (2010) Can we safely reduce blood loss during lumbar pedicle subtraction osteotomy procedures using tranexamic acid or aprotinin? A comparative study with controls. Spine 35(2):235–239
Besser MW, Ortmann E, Klein AA (2015) Haemostatic management of cardiac surgical haemorrhage. Anaesthesia 70(Suppl 1):87-e31
Braud S, Bon C, Wisner A (2000) Snake venom proteins acting on hemostasis. Biochimie 82(9–10):851–859
Brown JR, Birkmeyer NJ, O’Connor GT (2007) Meta-analysis comparing the effectiveness and adverse outcomes of antifibrinolytic agents in cardiac surgery. Circulation 115(22):2801–2813
Crescenti A, Borghi G, Bignami E et al (2011) Intraoperative use of tranexamic acid to reduce transfusion rate in patients undergoing radical retropubic prostatectomy: double blind, randomised, placebo controlled trial. BMJ 343:d5701
Despotis GJ, Avidan MS, Hogue CW Jr (2001) Mechanisms and attenuation of hemostatic activation during extracorporeal circulation. Ann Thorac Surg 72(5):S1821–S1831
Devlin JW, Tyburski JG, Moed B (2001) Implementation and evaluation of guidelines for use of enoxaparin as deep vein thrombosis prophylaxis after major trauma. Pharmacotherapy 21(6):740–747
Ee PL, Kempen PM (2006) Elective surgery days after myocardial infarction: clinical and ethical considerations. J Clin Anesth 18(5):363–366
Elgafy H, Bransford RJ, McGuire RA, Dettori JR, Fischer D (2010) Blood loss in major spine surgery: are there effective measures to decrease massive hemorrhage in major spine fusion surgery? Spine 35(9 Suppl):S47–S56
Hardy JF, Belisle S (1997) Natural and synthetic antifibrinolytics: inert, poisonous or therapeutic agents? Can J Anaesth J Can d’anesthesie 44(9):913–917
Hassan N, Halanski M, Wincek J et al (2011) Blood management in pediatric spinal deformity surgery: review of a 2-year experience. Transfusion 51(10):2133–2141
Ho WK, Baccala M, Thom J, Eikelboom JW (2005) High prevalence of abnormal preoperative coagulation tests in patients with adolescent idiopathic scoliosis. J Thromb Haemost JTH 3(5):1094–1095
Machovec KA, Jooste EH, Walczak RJ et al (2014) A change in anticoagulation monitoring improves safety, reduces transfusion, and reduces costs in infants on cardiopulmonary bypass. Paediatr Anaesth. doi:10.1111/pan.12591 [Epub ahead of print]
Mitchell JP, Schuller D, Calandrino FS, Schuster DP (1992) Improved outcome based on fluid management in critically ill patients requiring pulmonary artery catheterization. Am Rev Respir Dis 145(5):990–998
Murray DJ, Gress K, Weinstein SL (1992) Coagulopathy after reinfusion of autologous scavenged red blood cells. Anesth Analg 75(1):125–129
Pirkle H (1998) Thrombin-like enzymes from snake venoms: an updated inventory. Scientific and Standardization Committee’s Registry of exogenous hemostatic factors. Thromb Haemost 79(3):675–683
Silliman CC, Paterson AJ, Dickey WO et al (1997) The association of biologically active lipids with the development of transfusion-related acute lung injury: a retrospective study. Transfusion 37(7):719–726
Stocker K, Barlow GH (1976) The coagulant enzyme from Bothrops atrox venom (batroxobin). Methods Enzymol 45:214–223
Sugai K, Imamura Y, Uechi S et al (1986) Metabolic fate of batroxobin in human. Yakugaku Zasshi J Pharm Soc Jpn 106(4):335–342
Tanaka KA, Key NS, Levy JH (2009) Blood coagulation: hemostasis and thrombin regulation. Anesth Analg 108(5):1433–1446
Verma K, Errico TJ, Vaz KM, Lonner BS (2010) A prospective, randomized, double-blinded single-site control study comparing blood loss prevention of tranexamic acid (TXA) to epsilon aminocaproic acid (EACA) for corrective spinal surgery. BMC Surg 10:13
Xu C, Wu A, Yue Y (2012) Which is more effective in adolescent idiopathic scoliosis surgery: batroxobin, tranexamic acid or a combination? Arch Orthop Trauma Surg 132(1):25–31
Yagi M, Hasegawa J, Nagoshi N et al (2012) Does the intraoperative tranexamic acid decrease operative blood loss during posterior spinal fusion for treatment of adolescent idiopathic scoliosis? Spine 37(21):E1336–E1342
You KE, Koo MA, Lee DH et al (2014) The effective control of a bleeding injury using a medical adhesive containing batroxobin. Biomed Mater 9(2):025002
Zeng Z, Xiao P, Chen J, Wei Y (2009) Are batroxobin agents effective for perioperative hemorrhage in thoracic surgery? A systematic review of randomized controlled trials. Blood Coagul Fibrinolysis Int J Haemost Thromb 20(2):101–107
Zhang H, Chen J, Chen F, Que W (2012) The effect of tranexamic acid on blood loss and use of blood products in total knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 20(9):1742–1752
Conflict of interest
The authors have no personal, financial, or institutional interest in any of the drugs, materials, or devices described in this article.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Hu, HM., Chen, L., Frary, C.E. et al. The beneficial effect of Batroxobin on blood loss reduction in spinal fusion surgery: a prospective, randomized, double-blind, placebo-controlled study. Arch Orthop Trauma Surg 135, 491–497 (2015). https://doi.org/10.1007/s00402-015-2183-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-015-2183-0